Chapter 5 Imaging of the Elbow
Background – imaging modalities
Digital, computed or conventional radiographs
Radiographic imaging is the first-line investigation of many elbow pathologies as it provides a cost-effective, reliable, easily accessible, quick and safe method of assessing acute and chronic elbow conditions. Frontal and lateral views are considered standard and further imaging with oblique radiographs is now rarely requested, as CT, US or MRI is usually better placed to provide further insight.1
Sensitivity of elbow radiographs to bone injury and pathology is relatively high, although sensitivity falls when the clinician reviewing the film is inexperienced.2 While most of the information available from radiographs relates to bone, the value of the soft tissue signs visible on many radiographs should not be underestimated. Elevation of the anterior and posterior fat pads may indicate a joint effusion or haemarthrosis, which in turn may predict the presence of an occult fracture in the context of trauma. Alternatively, the elevated fat pad may indicate an effusion or synovitis secondary to an erosive arthropathy, infection or loose intra-articular bodies. Periarticular mineralization is often present in crystal arthropathies, hydroxyapatite deposition or in relation to ligaments and muscle following trauma.
Radiographic imaging is often the only imaging that is required in the follow-up of fractures, dislocation and after surgical intervention (Fig. 5.1).
Magnetic resonance imaging
In many ways magnetic resonance imaging (MRI) provides the ideal modality for investigating the elbow, where it gives excellent anatomical resolution, particularly of ligaments,3 tendons, articular cartilage and subchondral bone and neurovascular structures.4 Multi-planar imaging allows these structures to be clearly identified from several ‘viewpoints’, usually the axial, coronal or sagittal plane. MRI holds the greatest advantage over ultrasound where multiple structures are thought to be abnormal and where the suspected pathology is deep within the joint, rather than superficial.
Where possible the elbow should be imaged using a surface or circular coil with the joint extended and forearm supinated, although in practice this may not be possible because of pain or deformity. In order to maximize MR image quality, the patient should be as comfortable as possible. Careful positioning of the upper limb and elbow during MRI may be used to better demonstrate structures that present an imaging challenge, such as the distal biceps tendon,5 where the elbow is flexed, the arm abducted and the forearm supinated (FABS). Oblique structures may be better visualized by additional imaging with a microscopy coil applied close to the ligament or joint region in question and acquiring thin-slice (1–2 mm) volume data with a T2* gradient echo (GRE), STIR or PD FS TSE sequence, although image acquisition time is significantly increased with this technique.3
Bone scintigraphy
Bone scintigraphy (or a bone scan) may be used to identify metabolically active bone lesions in the elbow, particularly where MRI, CT, plain films and radiographs have not produced a definitive diagnosis, or where one or more of these modalities cannot be utilized. The bone scan uses a radioactive tracer (technetium 99m) attached to methylene diphosphonate (MDP); the MDP is taken up by osteoblasts and is therefore a marker of physiological bone activity. The gamma radiation emitted by decay of technetium 99m is used by a gamma camera to form an image. Single-positron emission computed tomography (SPECT) produces a CT image of the joint, allowing more exact anatomical resolution of pathology. While bone scanning involves the injection of radioactive material into the body, it produces a relatively low effective radiation dose of the order of 0.008 mSv in an adult and 0.025 mSv in a child,6 compared with 2 mSv for a standard appendicular CT scan.
Elbow arthrography
Arthrography may be used in conjunction with CT, MRI and US in the investigation of elbow disorders.7–9 While there are several approaches to intra-articular injection, I find that a posterolateral approach into the radiocapitellar joint, immediately posterior to the radial collateral ligament, is the most reliable method of safely accessing the joint space.
In CT arthrography 2–3 mL of dilute low osmolar contrast medium (LOCM), followed by 5–10 mL of air, as tolerated by the patient, may be injected under ultrasound, fluoroscopic or CT guidance to produce a double-contrast CT arthrogram. Alternatively, 8–15 mL of dilute LOCM (50 : 50 mix with 0.9% saline solution) may be injected to produce a single-contrast CT arthrogram. Axial slices are acquired, preferably with ultra-thin multi-slice CT, and then reconstructed in the coronal and sagittal plane (or any plane required). CT arthrography is most useful when looking for loose bodies and osteophyte impingement, although it may be used to demonstrate chondral and osteochondral fractures.7
MR arthrography is a useful adjunct to conventional MRI, particularly in the assessment of the collateral ligaments, synovial and capsular pathology, and articular cartilage and osteochondral injuries.7,8 Direct arthrography involves injection of LOCM under ultrasound or fluoroscopic guidance, followed by 8–15 mL of either saline or, more commonly, a 1 : 200 solution (2 mmol/L) of gadolinium DTPA, into the elbow joint, followed by MRI.
US arthrography is mainly used to look for the presence of osteochondral loose bodies and involves the injection of 8–15 mL of saline into the joint under US guidance.9
Musculotendinous pathology
Anterior muscle group
The biceps brachii and brachialis muscles are found anteriorly and insert into the radial and ulnar tuberosities, respectively. The distal biceps tendon is made up of a weak aponeurosis, the lacertus fibrosus, which inserts into the antebrachial fascia of the ulnar aspect of the proximal forearm, and a strong lateral tendon that passes through the deep part of the antecubital fossa to insert into the medial aspect of the radial tuberosity. The lacertus fibrosus and the lateral tendon components of the distal biceps tendon correspond to the short and long head of the biceps muscle and may be found as separate bifurcated muscles in a significant minority of normal individuals.10
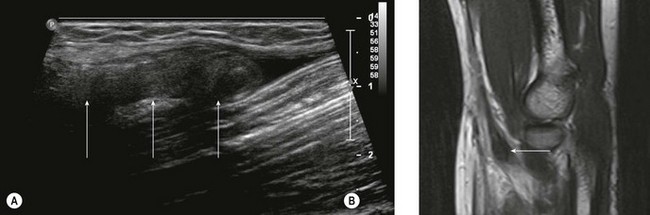
While the majority of biceps injuries involve the proximal, long head of the biceps tendon, the distal tendon is also prone to injury and accounts for approximately 5% of biceps injuries. US provides a good first-line investigation of the biceps tendon.11,12 Complete tendon rupture can be confirmed with US, which will also define the extent of tendon retraction (Fig. 5.2). When looking at the tendon in longitudinal section, the US probe should be oriented with inferolateral angulation, with the elbow flexed and the forearm supinated. When looking at the tendon in transverse section, the probe is held at right angles to the long axis of the forearm. If the heel of the probe is gently pressed into the interosseous groove towards the radial tuberosity, better imaging of the tendon insertion is possible.
Partial tears of the distal biceps tendon may be diagnosed by identifying thickening of the tendon close to the radial tuberosity, together with a wavy appearance of the distal tendon on longitudinal scanning.13 The tendon is most prone to tendinosis and tears close to the radial tuberosity as a result of distal tendon impingement between the radius and ulna and relative hypovascularity of the tendon in this region (Fig. 5.3). Unfortunately, it is also this region of the tendon that is most difficult to visualize with US and most prone to anisotropic artefact as a result of its oblique route. If there is doubt about the US findings, further imaging with MRI is advised.
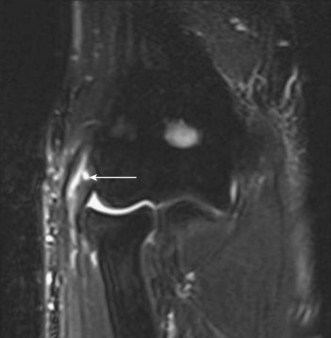
MRI of the distal biceps tendon is best performed with axial and sagittal imaging. However, the oblique course of the tendon often makes standard MRI imaging less than satisfactory. Improved visualization of the distal tendon and insertion can be achieved with the FABS view, where the elbow is flexed, the arm abducted and the forearm supinated.5 The images are acquired in the coronal plane of the elbow, perpendicular to the radius, with proton density with and without fat suppression, or T1 SE and T2 TSE with fat suppression, in addition to standard elbow sequences. This method of imaging the biceps tendon is particularly useful in detecting partial tears of the tendon (Fig. 5.4).5
Lateral muscle group
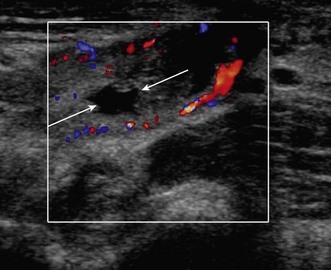
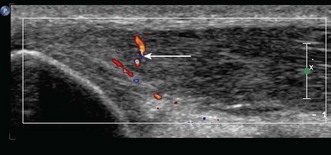
Lateral epicondylitis or tennis elbow is the most frequent cause of elbow discomfort.14 The diagnosis is often made from the history and clinical examination alone. Activities that may lead to overuse injury include throwing and racket sports and occupations involving repetitive forearm movement. It is most common in people aged 30–50, smokers and weekend warriors, who undertake intermittent bursts of high activity. Where there is clinical doubt about the diagnosis, or where the patient is not responding to treatment, the diagnosis may be confirmed with ultrasound or MRI. US will show a thickened common extensor origin, often with areas of hypoechoic change or hypervascularity on Doppler imaging (Fig. 5.5).15
US has been shown to be less sensitive than MRI in demonstrating epicondylitis, but has a similar specificity.16 However, US has a number of advantages over MRI. The tendon origin is often tender to US probe pressure, allowing a degree of clinical correlation with the imaging findings. Comparison can be made with the contralateral elbow, particularly where the findings are subtle. Gentle valgus stress during US imaging may demonstrate gaping of partial- or full-thickness tears.
MRI will demonstrate ill-defined, increased T2 signal on fluid-sensitive sequences, (STIR or fat saturation), within the common extensor origin, often with oedema surrounding the tendon or within the lateral epicondyle. Partial or complete tears may show a better-defined focus of high T2 signal within the tear, with partial or complete disruption of muscle fibres (Fig. 5.6). Partial tears can show both a thickened or thinned appearance. MRI may also be used to assess an associated lateral ulnar collateral ligament injury.17
Medial muscle group
Injuries of the medial muscle group are less common, with lateral epicondylitis occurring 10 times more frequently than medial epicondylitis (tendinosis of the common flexor origin). Medial epicondylitis or golfer’s elbow usually involves the pronator teres, flexor carpi radialis and palmaris longus muscle origins. Precipitating factors include an acute injury with valgus strain and sudden deceleration, such as when a golf club hits a tree root, and chronic repetitive valgus strain in racket sport, golf and during throwing activities. Ultrasound examination will show a thickened, hypoechoic tendon origin with increased vascularity on Doppler imaging. There may be enthesial change within the cortex of the medial epicondyle, particularly where the injury is chronic or where there is a history of long-term overuse or valgus stress (Fig. 5.7).
Posterior muscle group
Injury to the triceps muscle is relatively infrequent and usually follows a fall onto an outstretched arm or a direct blow to the muscle.18 The diagnosis of triceps rupture can be made with US, with the probe oriented in the sagittal plane. The tendon appears corrugated and is often outlined by fluid, with haematoma and debris in the rupture defect. Triceps rupture is often associated with bony avulsion of the insertion and in this situation the retracted bony avulsion fragment can be easily identified with US. In addition, the presence of a large haematoma that may lead to compartment syndrome and radial nerve compression19 can be identified quickly and easily. Compression of the ulnar nerve has also been reported,20,21 and fluid or haematoma within the cubital tunnel is visible with US.
Triceps tendinosis shows US changes identical to those seen in epicondylitis. The difficulty lies in differentiating a partial tendon tear from tendinosis, as both may have a similar appearance on US, with hypoechoic change within a thickened tendon. Disruption of the usual striated, fibrillar pattern indicates a tear rather than tendinosis.18,22 If doubt persists, sagittal T2 FS MRI will show a better-defined focus of altered T2 signal change within a partial tear and ill-defined or diffuse oedema with tendinosis.
A snapping triceps tendon, caused by subluxation of the medial head of triceps over the medial malleolus, may be demonstrated with US if the probe is held over the distal triceps while the elbow is flexed.23 This may be associated with a swollen ulnar nerve indicating neuropathy, or occasionally with coexistent subluxation of the ulnar nerve.23
Entrapment neuropathy, neural tumours and trauma
Ulnar nerve
Ulnar nerve compression is relatively common, with the incidence of ulnar nerve entrapment at the elbow second only to entrapment of the median nerve in the carpal tunnel.24 The ulnar nerve lies immediately posterior to the medial malleolus and reaches the forearm through the cubital tunnel. From proximal to distal the nerve courses through the condylar groove and then deep to the tunnel retinaculum and arcuate ligament, before passing between the ulnar and humeral heads of flexor carpi ulnaris. Compression of the ulnar nerve is most common at two points in the cubital tunnel: proximally, within the condylar groove; and distally, at the point where the nerve reaches the flexor carpi ulnaris.
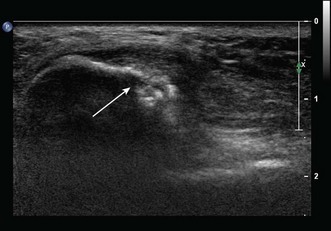
US examination of the ulnar nerve is best performed with the arm abducted and externally rotated. A high-frequency probe with a narrow footprint should be held at right angles to the long axis of the arm, allowing the ulnar nerve to be identified in cross-section posterior to the medial malleolus before it enters the cubital tunnel. Ulnar nerve dislocation may be demonstrated if the probe is held over the ulnar nerve at the cubital tunnel while the patient moves the elbow from extension to flexion.23
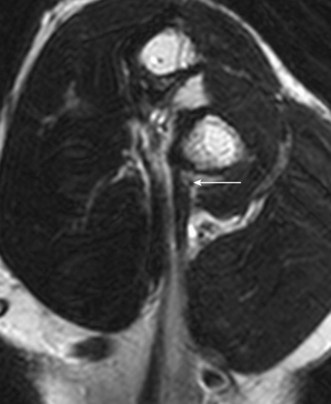
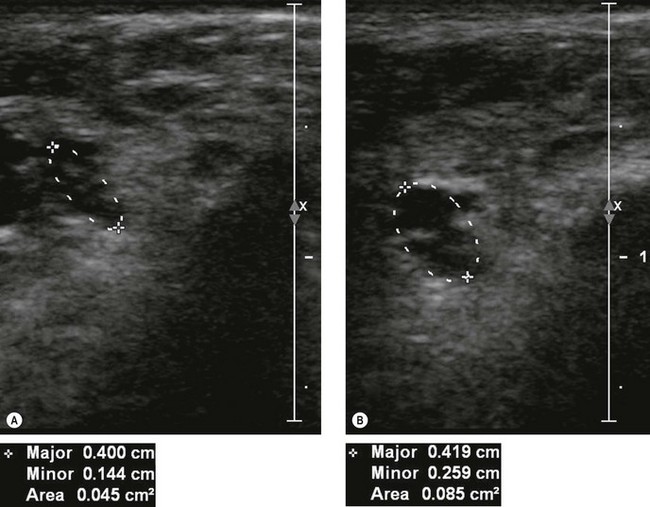
If US shows a thickened nerve proximal to the cubital tunnel,25 with a cross-sectional area greater than 7.5 mm2 (0.075 cm2) at the level of the medial epicondyle this is diagnostic of entrapment neuropathy (Fig. 5.8).26 It is helpful to compare the cross-sectional diameter with the normal, contralateral ulnar nerve to confirm that the nerve is swollen. US may also be used to look for extrinsic causes of compression such as an accessory medial anconeus muscle, the anconeus epitrochlearis, ganglion cysts, synovial thickening and osteophytes arising from the posteromedial margin of the ulnar trochlear joint.27
When MRI is used to examine the ulnar nerve, the nerve is most easily identified with axial T1 SE or PD sequences. The ulnar nerve will appear enlarged at the level of the cubital tunnel, with increased T2 signal in the nerve on T2 FSE or T2 FSE with fat suppression imaging.24
The ulnar nerve is also more prone to injury at the elbow and proximal forearm than the wrist or upper arm, typically as a result of a laceration, blunt trauma or in association with an elbow fracture or dislocation.28 Many injuries will show improvement in neurological function over time and will not need surgical repair, particularly where the trauma is blunt.28 In addition, there is frequently distortion of soft tissue anatomy in the acute phase, which makes both US and MRI less reliable. For these reasons it may be advisable to delay imaging until the swelling has subsided and to limit further investigation to those patients who show no sign of improvement of clinical signs or electromyography (EMG).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree