CHAPTER 20 Humeral Prosthetic Positioning
Humeral prosthetic positioning remains the most difficult step in performing unconstrained shoulder arthroplasty for fracture. Placing the humeral component excessively proud or in excessive retroversion may result in loss of fixation and subsequent migration of the greater tuberosity (Figs. 20-1 and 20-2). The complication of tuberosity migration has been found to be a key factor in poor results after unconstrained shoulder arthroplasty performed for the treatment of proximal humeral fractures.1 This chapter details humeral prosthetic positioning with each of the techniques described in Chapter 18.
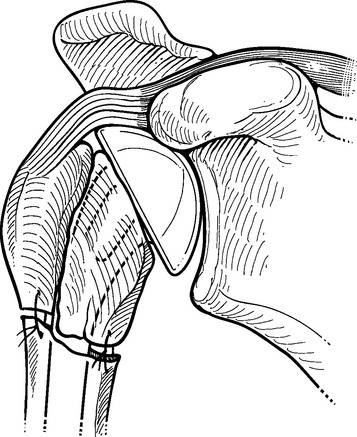
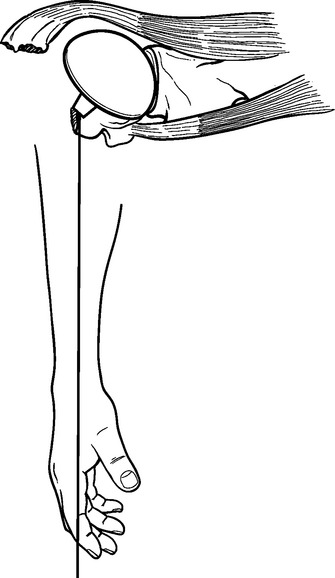
Figure 20-1 Placement of the humeral prosthesis excessively proud can result in loss of greater tuberosity fixation.
IDENTIFICATION AND PREPARATION OF THE HUMERAL DIAPHYSIS
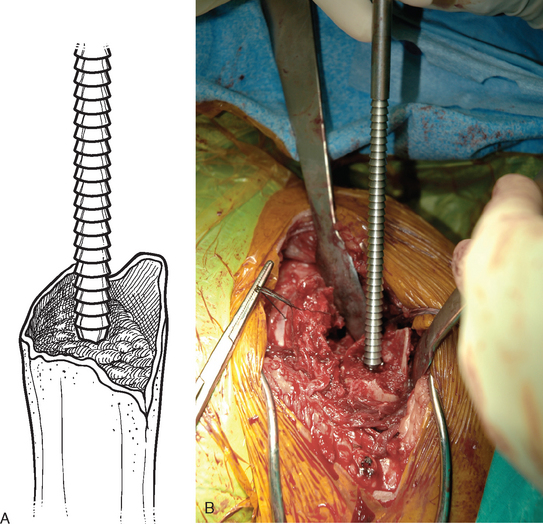
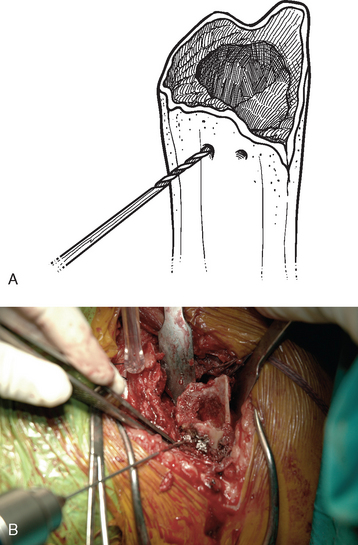
After control of both tuberosities has been achieved, the humeral shaft is identified. The humeral shaft is progressively reamed until the reamer that is used corresponds to the diameter of the prosthesis to be implanted (Fig. 20-3). Using the largest diaphyseal reamer that is possible to advance down the humeral canal without difficulty avoids selecting too small a diameter of the humeral implant, which can inadvertently be positioned in valgus or varus (Fig. 20-4). Because most of these patients are severely osteopenic, however, no effort is made to force too large a reamer down the humeral canal for fear of iatrogenic fracture. The bicipital groove is located and two 2-mm holes are drilled in the humeral shaft approximately 1 cm distal to the fracture site, one on each side of the bicipital groove, for use later in tuberosity fixation (Fig. 20-5). The intra-articular portion of the long head of the biceps, which is frequently at least partially torn, is excised, and suture tenodesis of the remaining stump to the pectoralis major tendon is carried out with no. 1 nonabsorbable braided suture in a figure-of-eight stitch as described in Chapter 5.2
SELECTION OF THE HUMERAL IMPLANT
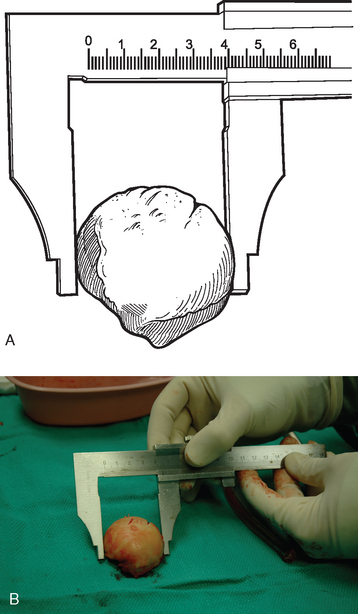
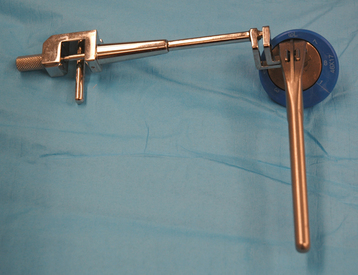
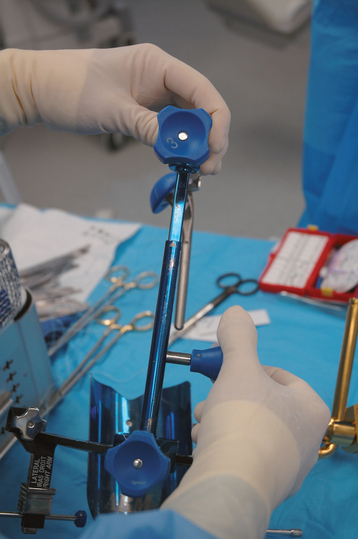
The trial humeral implant is then assembled by selecting a stem with a diameter corresponding to the largest diaphyseal reamer used and a head size corresponding to the size of the removed head fracture fragment. The humeral head fragment is usually slightly ovoid and has a lesser and greater diameter. A head size corresponding to the lesser diameter is selected to avoid insertion of too large a component, which can lead to nonunion of the tuberosities (Fig. 20-6). The prosthetic system that we use allows variation of the posterior and medial offset of the humeral head seen in normal anatomy. The “R” and “L” positions correspond to the average anatomic posterior and medial offset of a given head size for a right and left shoulder, respectively (Fig. 20-7). The variable offset is set to the “R” or “L” position, depending on whether surgery is being performed on the right or left shoulder. Once selected, the trial implant is attached to the prosthetic holder (Fig. 20-8).
PROSTHETIC POSITIONING WITH ANCILLARY INSTRUMENTATION—THE FRACTURE JIG TECHNIQUE
Placement of the prosthesis at the correct height and version remains one of the most difficult challenges when performing shoulder arthroplasty for fracture. Use of ancillary instrumentation enhances the surgeon’s ability to place the prosthesis at the correct height and in the correct amount of retroversion. The fracture jig references the humeral epicondyles to allow intraoperative estimation of proper prosthetic height and retroversion. More importantly, the fracture jig permits trial reduction of the glenohumeral joint and reduction of the tuberosities before final cementation of the humeral implant, thereby allowing adjustment of prosthetic position.
Selection of appropriate humeral height is initiated preoperatively by evaluating the length of the uninjured humerus from the superior aspect of the greater tuberosity to the transepicondylar axis radiographically, as described in Chapter 18. This measurement provides an estimated height at which to set the fracture jig during the procedure (Fig. 20-9). Appropriate humeral retroversion is provided by the protractor component of the fracture jig and is usually between 20 and 30 degrees relative to the transepicondylar humeral axis (Fig. 20-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree