CHAPTER 39 Humeral Component
Reconstruction of the proximal humerus can be a very difficult aspect of revision shoulder arthroplasty. During extraction of the previous humeral stem, every effort should be made to preserve as much native proximal humeral bone as possible (see Chapter 38). The overall condition of the proximal humerus and rotator cuff plays a significant role in determining the type of implant to be used in revision surgery (unconstrained versus semiconstrained). In cases in which the rotator cuff is largely functional, preservation of the greater and lesser tuberosities helps dictate which type of revision implant to use during revision surgery. Once the type of revision implant to be used is selected, preparation of the proximal humerus and implantation of the humeral component proceed just as for primary arthroplasty. This chapter details our techniques for reconstruction and preparation of the proximal humerus and implantation of the humeral component in revision shoulder arthroplasty.
TECHNIQUE FOR PREPARATION OF THE PROXIMAL HUMERUS
Unconstrained Humeral Stem
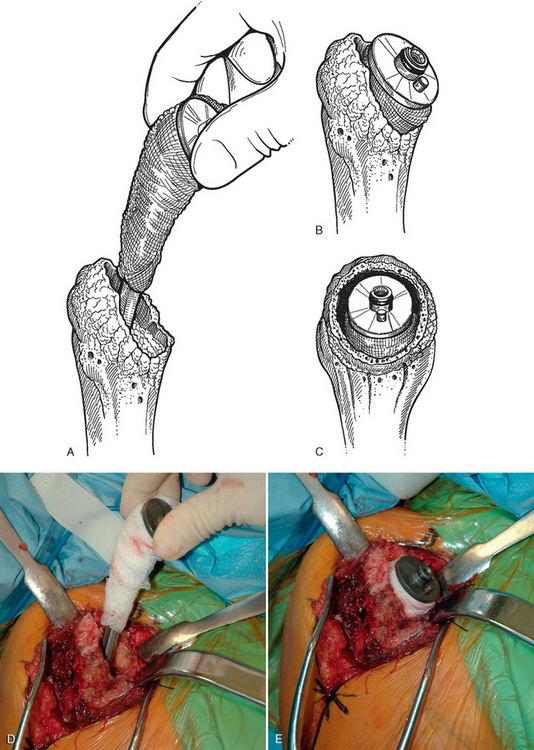
In cases in which we are going to implant an unconstrained proximal humeral stem, we prefer to implant a stem with geometry designed originally for use in proximal humeral fractures. This cemented stem design allows a good fit into the humeral metaphysis and comes in a variety of lengths. This allows the surgeon to treat periprosthetic fractures or bypass the distal aspect of a humeral diaphyseal osteotomy used for extraction of the humeral stem (Fig. 39-1).
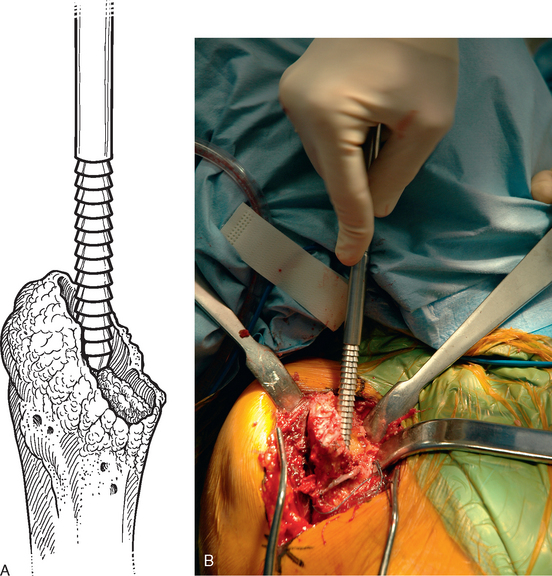
For this revision stem, no metaphyseal broaching is necessary. The diaphysis is progressively reamed with the hand reamers provided (Fig. 39-2). Frequently, after removing an uncemented humeral stem, a small pedestal of bone exists in the intramedullary canal at the level just distal to the tip of the original humeral stem (Fig. 39-3). It is easy to tap the smallest diaphyseal reamer through this osseous pedestal. Subsequent reamers pass through this area without difficulty.
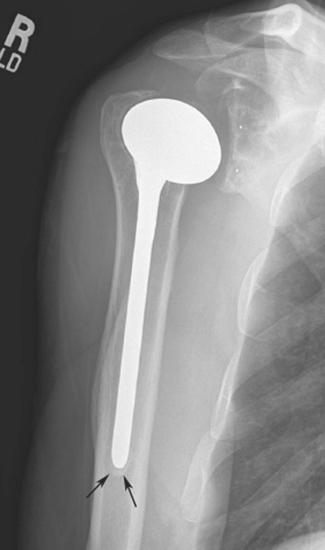
Figure 39-3 Pedestal of intramedullary cortical bone (arrows) distal to the tip of an uncemented humeral stem.
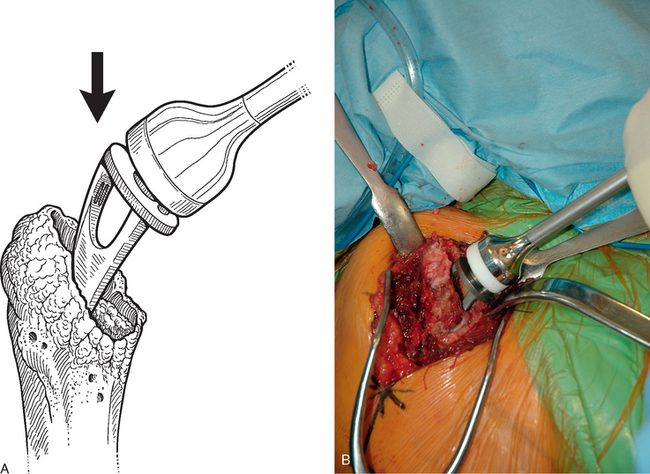
Once a humeral stem diameter of appropriate size is selected, the trial humeral stem is inserted by impacting the stem into the proximal humerus (Fig. 39-4). Effort is made to impact the stem laterally into the tuberosities (Fig. 39-5). It is not necessary to broach the humeral metaphysis because the bone in this area is relatively soft and compresses sufficiently to allow full seating of the implant. On occasion, the metaphyseal bone will be moderately to severely osteopenic, and the trial humeral stem will fall into the medial portion of the metaphysis (Fig. 39-6). This “loose fit” hinders testing of the trial implant. The trial may be stabilized within the proximal humerus in this scenario by wrapping a sterile sponge (or portion of a sterile sponge) around the metaphyseal portion of the trial implant before placing it in the humeral canal (Fig. 39-7).
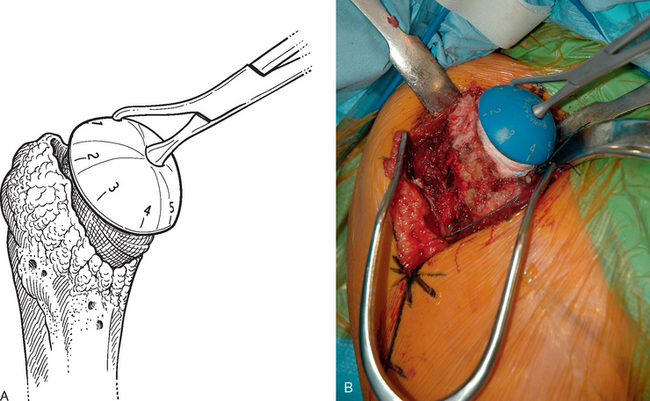
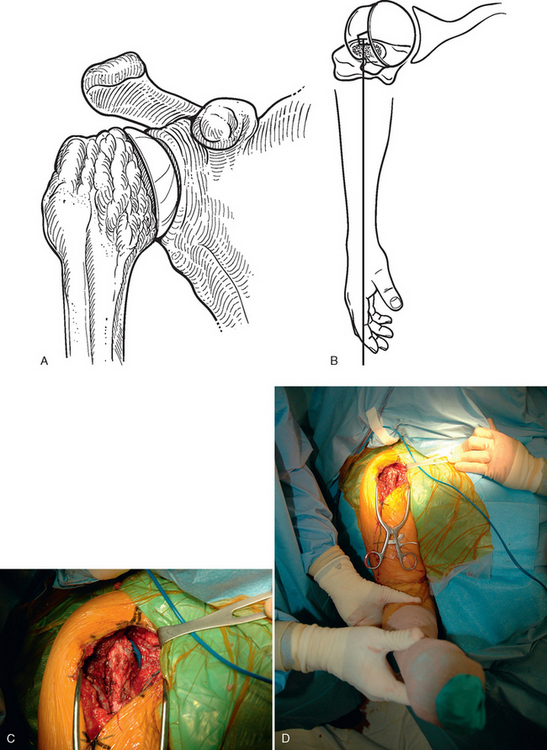
Once the trial humeral stem is securely placed in the proximal humerus, a humeral head implant of appropriate size is selected. The prosthetic head should provide adequate coverage of the proximal humeral metaphysis but not overhang the humerus at any portion. The system that we use allows variable medial-to-lateral and anterior-to-posterior offset. The prosthetic humeral head is placed on the trial humeral stem at the various offset positions to allow selection of the best offset index (Fig. 39-8). Once the proper index has been selected, the glenohumeral joint is reduced and humeral version is judged. With the arm in neutral rotation, the center of the prosthetic humeral head should align with the center of the glenoid, provided that osseous glenoid morphology is intact and does not demonstrate a nonconcentric wear pattern (Fig. 39-9). In cases with nonconcentric glenoid morphology or cases in which the osseous glenoid is compromised, we judge humeral version by placing the prosthesis in approximately 30 degrees of retroversion relative to the long axis of the forearm (Fig. 39-10). If the version of the trial humeral stem is unacceptable, the humeral trial is removed and humeral version changed by revising the original plane of humeral head resection by way of a revision humeral cut to introduce more retroversion or anteversion, as deemed appropriate by the trial glenohumeral reduction. The trial humeral implant is reinserted and the trial reduction repeated to ensure that humeral version has been corrected acceptably.
Reverse-Design Humeral Stem
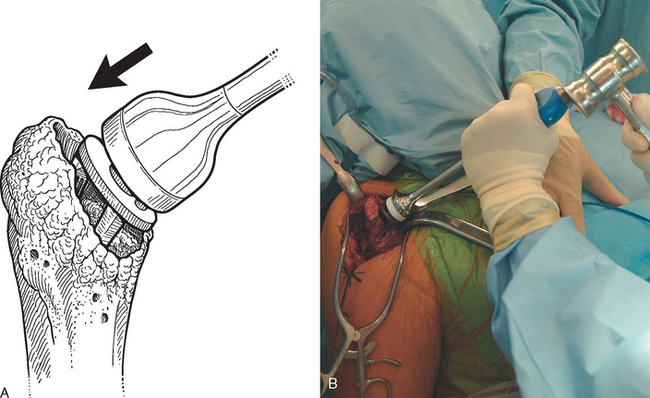
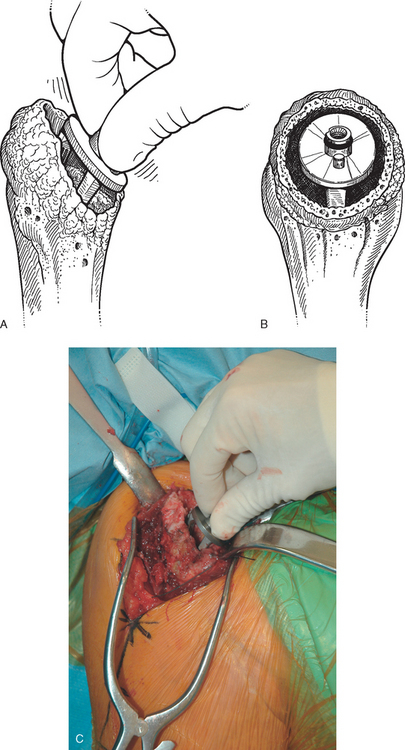
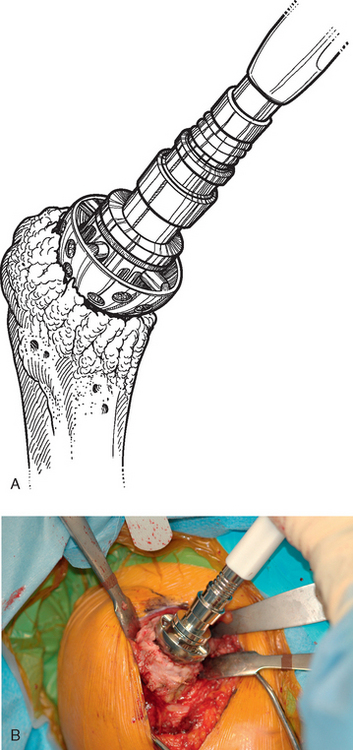
In cases in which a reverse-design humeral implant is to be used as the revision humeral stem and the osseous proximal humerus is relatively preserved, the epiphysis, metaphysis, and diaphysis are prepared in much the same way as for insertion of a reverse prosthesis as a primary implant. The epiphyseal reamer is first used to create a place for the proximal portion of the humeral implant (Fig. 39-11), after which the metaphyseal hand reamer is used (Fig. 39-12). Progressive diaphyseal reaming is then performed, with penetration of any osseous pedestal present in the humeral canal (Fig. 39-13). The trial humeral stem is assembled by using an implant diameter corresponding to the largest-diameter diaphyseal reamer that was used. The trial humeral implant is placed in approximately 10 degrees of humeral retroversion by using the forearm referencing insertion instrument and is fully impacted (Fig. 39-14). The position of the fin is marked on the proximal humerus with the electrocautery (Fig. 39-15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree