CHAPTER 11 Humeral Component
For unconstrained shoulder arthroplasty, both cemented and uncemented humeral stemmed components are available (Figs. 11-1 and 11-2). The incidence of aseptic loosening of cemented humeral stems is less than 2%.1 Similarly, the incidence of aseptic loosening of uncemented textured humeral stems is negligible.2 Implantation of smooth, polished humeral components without cement has led to a 55% incidence of humeral loosening and should be avoided.1 In most cases of unconstrained shoulder arthroplasty, the choice of cemented or uncemented humeral stems is based on surgeon preference. In our practice we prefer the use of uncemented humeral stems in most cases. Use of uncemented humeral stems eliminates the time required for cement preparation and insertion. Our indication for use of a cemented humeral stem is preexisting deformity of the proximal humerus or severe proximal humeral osteopenia precluding initial fixation of an uncemented humeral stem (Fig. 11-3). Many different prosthetic systems are available for unconstrained shoulder arthroplasty, and it is beyond the scope of this textbook to describe the specific techniques used for each of these systems. This chapter describes the technique for preparation of the proximal humerus with our preferred prosthetic system. Most of the steps are applicable regardless of the system used.
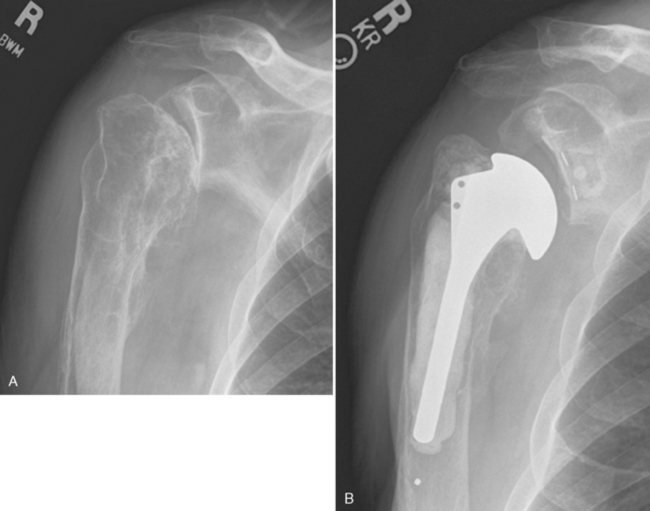
Figure 11-3 A and B, Proximal humeral malunion necessitating use of a smaller-diameter cemented humeral stem.
TECHNIQUE FOR INSERTION OF AN UNCEMENTED HUMERAL COMPONENT
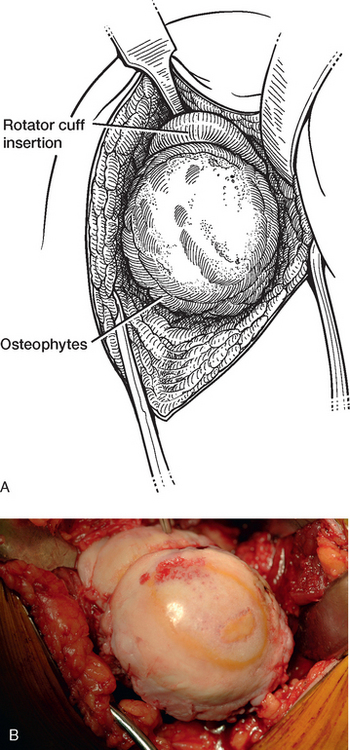
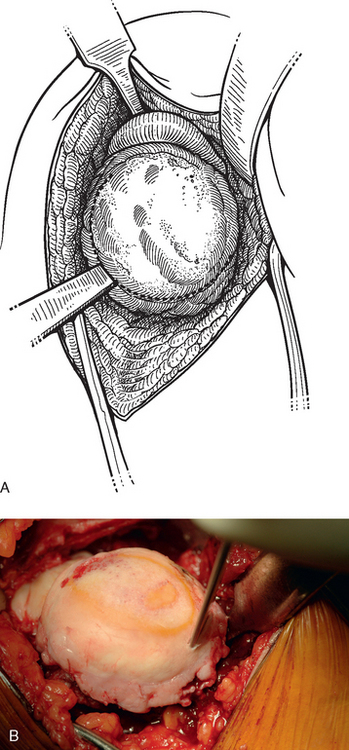
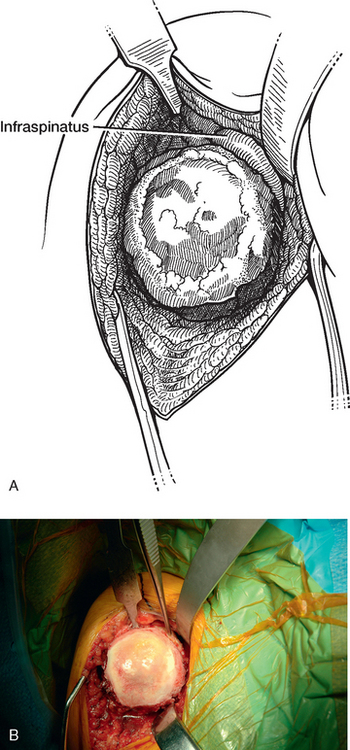
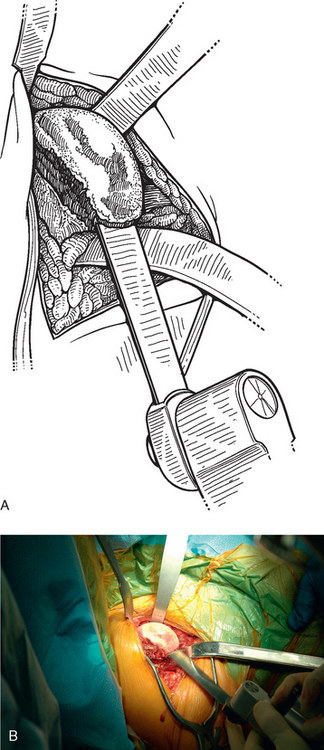
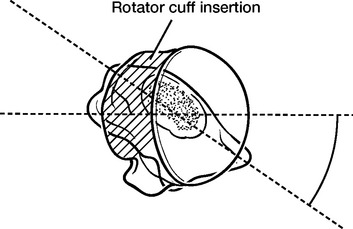
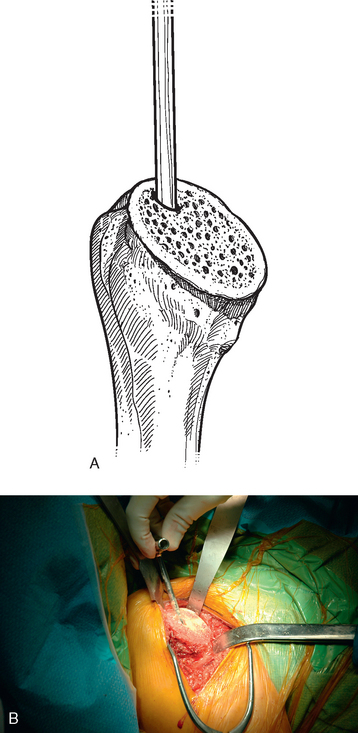
Once the inferior capsule is released from the neck of the glenoid as described in Chapter 10, humeral preparation begins. The humeral head retractor is removed, and the humeral head is dislocated by externally rotating and extending the arm (Fig. 11-4). A Hohmann retractor positioned superior to the coracoid process is moved to the margin of the bare area of the humeral head articular surface (junction of the supraspinatus and infraspinatus), and a modified Hohmann retractor (see Chapter 3) is placed inferiorly and medially at the surgical neck of the humerus. This completes the proximal humeral exposure (Fig. 11-5). The presence and extent of humeral head osteophytes vary with the underlying diagnosis. Whereas conditions such as primary osteoarthritis typically have large osteophytes, other conditions such as rheumatoid arthritis have a paucity of osteophytes. The anteroposterior radiograph is helpful in determining the presence and extent of humeral osteophytes. To identify the true anatomic neck of the humerus, the osteophytes are removed with a ½-inch straight osteotome (Fig. 11-6). Typically, a layer of adipose tissue is present between the osteophytes and the native humerus and aids in identification of the normal margin of the humeral head articular surface (Fig. 11-7). The insertion of the infraspinatus tendon should be readily visible on the posterior aspect of the humerus (Fig. 11-8). It is critical to visualize the infraspinatus to prevent damage to the posterior rotator cuff during humeral head resection. Additionally, when using a prosthesis with an anatomic design, the location of the posterior rotator cuff (infraspinatus) defines humeral version (which varies from 7 degrees of anteversion to 48 degrees of retroversion) and, consequently, version of the humeral head cut.3 After identification of the insertion of the infraspinatus, the humeral head is removed at the anatomic neck of the humerus with an oscillating saw (Fig. 11-9). We believe it acceptable to leave the bare area of the humeral head because this allows a margin of error for protection of the posterior rotator cuff during humeral head resection. Proper head resection at the anatomic neck correctly replicates humeral version. Figure 11-10 depicts the relationship between humeral version and insertion of the rotator cuff.
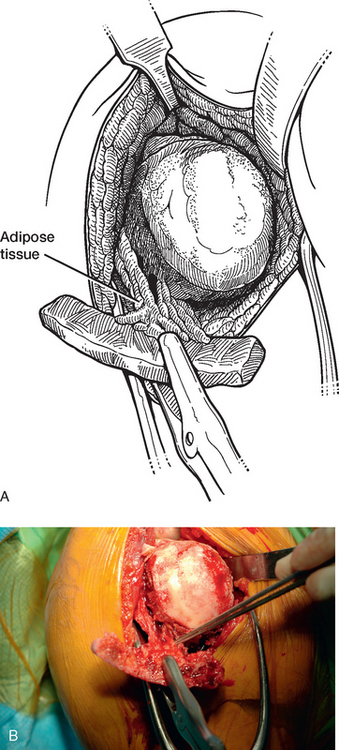
Figure 11-7 A and B, Layer of adipose tissue interposed between the osteophytes and the native humerus.
We use an adaptable anatomic prosthetic system (Aequalis Prosthetic System, Tornier, Inc., Stafford, TX) with the goal of reproducing the normal anatomy of each patient. This system permits specification of humeral stem diameter, humeral head diameter, anatomic neck inclination, and humeral head offset. With this system the humeral canal is identified and entered with an awl; the entry point is typically on the anterior and lateral aspect of the cut surface because of the normal posterior and medial offset of the humeral head with respect to the humeral diaphysis (Fig. 11-11). Progressive diaphyseal reaming is performed with manual instrumentation to reach the inner humeral cortex. The preoperative anteroposterior radiograph is helpful to estimate intramedullary canal diameter (Fig. 11-12). It is not critical that the diaphyseal fit be excessively “tight.” We prefer to use a smaller diaphyseal reamer rather than risk humeral fracture. The neck inclination guide is used to select the appropriate inclination of the prosthesis, which varies between 125 and 140 degrees in 5-degree increments (Fig. 11-13). If the neck inclination angle is not divisible by 5, we select the smaller angle; that is, we would select a 130-degree component if the actual measurement were 133 degrees. The proximal humerus seems to be able to better adapt to a smaller neck inclination angle than to one that is too large, hence our reason for selecting the prosthesis with the smaller inclination angle. Progressive metaphyseal broaching is performed to match the size of the largest reamer used (Fig. 11-14) while taking care to keep the broaches perpendicular to the cut surface of the humerus for maintenance of correct humeral version. The humeral inclination angle is marked on the broach to help the surgeon determine the appropriate depth to advance it (Fig. 11-15). Once reaming and broaching are complete, a trial stem is inserted (Fig. 11-16). The trial stem is assembled before insertion by combining a metaphyseal-diaphyseal portion that matches the largest size broach used and a humeral neck portion that matches the neck inclination angle selected (Fig. 11-17). A trial prosthetic humeral head is selected to match the size of the resected humeral head (Fig. 11-18). Most humeral heads are slightly elliptical; if this is the case, the smaller diameter is selected. Additionally, if the resected humeral head is between the sizes available in the prosthetic system, the smaller size is initially selected to avoid “overstuffing” the glenohumeral joint. The trial head is then placed on the trial stem. The Aequalis system incorporates variable medial and posterior head offset to allow the surgeon to position the head at one of eight indexed positions. The position that provides the best coverage of the cut humeral surface is selected (Fig. 11-19). Care is taken to avoid overhang of the prosthetic head anteriorly, superiorly, and posteriorly to prevent impingement of the rotator cuff. Inferior overhang, though not ideal, is acceptable. If a large amount of overhang is observed at any index, the selected head is probably too large. In areas in which the prosthetic head does not quite cover the cut humeral surface, a rongeur can be used to trim the cut surface and create a better fit. The entire humeral trial component is then removed. If a glenoid component is to be inserted, the cut humeral surface is covered with a humeral cut protector to prevent deformation of the humeral cut surface during glenoid preparation and implantation (Fig. 11-20). Care is taken to note the humeral head offset index before disassembling the trial humeral component so that the final humeral implant may be properly assembled. Except in cases in which we have selected the smallest humeral stem, we use a cut protector (assembled similar to the trial humeral implant except that the neck portion is replaced with a flat surface matching the selected inclination angle) with a metaphyseal-diaphyseal portion 1 size smaller than what has been selected for the trial stem to allow easier removal later in the procedure (Fig. 11-21). In cases in which the smallest humeral stem has been selected, the same size cut protector is used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree