Homodigital Island Flap
Bradon J. Wilhelmi
Damon Cooney
Single-stage reconstruction of the finger pulp has become possible with a better understanding of hand anatomy and the advent of new surgical techniques. Single-stage reconstruction eliminates the risk of a stiff finger resulting from immobilization and the necessity of a second operation that is required with traditional regional flap reconstruction. The options for one-stage reconstruction of pulp defects include heterodigital and homodigital neurovascular island flaps. The heterodigital neurovascular island flap has the disadvantage of late or no development of sensory reorientation and paresthesia in the donor finger. Harvesting the flap from the injured finger, as is the case in a homodigital island flap, avoids unnecessary surgery to an adjacent uninjured finger as well as potentially enhancing rehabilitation by minimizing additional hand trauma. Many homodigital neurovascular flaps based on one or two volar digital pedicles have been described which can provide the fingertip with sensate coverage. The palmar advancement flap based on bilateral neurovascular pedicles has been used for reconstruction of the thumb and fingers. The interphalangeal (IP) joint is usually needed to be kept in flexion to obtain adequate advancement of the flap, which increases the complication risk for flexion contracture of the distal joint with these advancement flaps. Also, the use of the advancement flap increases the risk for dorsal skin necrosis if the dorsal branches from the proper digital artery are severed for distal advancement of the flap. The volar V-Y flap is still a suitable flap for small fingertip defects less than 1 cm when there is sufficient skin distal to the distal interphalangeal (DIP) crease to base the flap.
Indications/Contraindications
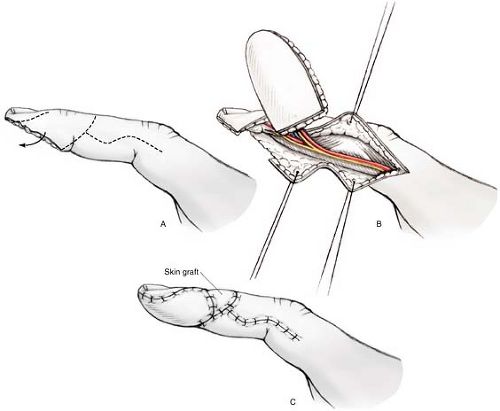
The homodigital neurovascular flap has been described with elevation of the dorsal finger skin to repair pulp deficits which cannot be closed with the volar V-Y advancement flap. Anatomic studies have demonstrated that a dorsal arterial branch from the proper digital artery exists over the middle phalanx which runs obliquely, dorsally, and distally over the distal interphalangeal crease. The dorsal branch at the middle phalanx collateralizes with the dorsal blood supply of the finger from another dorsal branch from the proper digital artery at the level of the distal phalanx, forming a dorsal arterial arcade over the DIP joint. Also, a dorsal nerve branch can be found leaving the proper digital nerve to innervate the dorsal finger skin proximal to the nail fold. The dorsal homodigital neurovascular island flap can be based on one or both of these arteries and this dorsal nerve. When the flap is harvested on the distal-most branches, it can be called the distal dorsal homodigital artery (DDHDA) flap. This DDHDA flap can be used to close defects of 2 × 2.5 cm just proximal to the tip and hyponychium (Fig. 22-1). Larger defects in this region can be reconstructed by a flap based on the dorsal branch at the middle phalanx, called the middle dorsal homodigital neurovascular island flap, or MDHDA flap. This MDHDA flap can be used to close defect 2 × 4 cm in size (Fig. 22-2). Alternatively, when the loss is very distal and an antegrade homodigital neurovascular island flap will not reach the defect, a reverse homodigital island flap (RHDA flap) can be used. The RHDA flap is harvested from the lateral base of the finger and based on proximal dorsal branches of the proper digital artery (Fig. 22-3). Dorsal branches of the proper digital nerve can be used to innervate this skin paddle, coapting this nerve to the transected nerve at the tip. These homodigital flaps are contraindicated when there is significant injury involving the pedicle or the skin on which the flap is based over the dorsum of the finger. Moreover, these homodigital flaps should not be used when
a skin bridge cannot be preserved for venous drainage to the distal finger. If the harvest of the flap would result in the exposure of already injured extensor tendon, devoid of paratenon, then the flap should be avoided. Crush and electrical injuries to the dorsal finger are also relative contraindications for the homodigital flap.
a skin bridge cannot be preserved for venous drainage to the distal finger. If the harvest of the flap would result in the exposure of already injured extensor tendon, devoid of paratenon, then the flap should be avoided. Crush and electrical injuries to the dorsal finger are also relative contraindications for the homodigital flap.
Preoperative Planning
The reconstruction of fingertip defects with homodigital island flaps should be performed in the operating room. The flap should be harvested with the use of a tourniquet to facilitate identification of anatomic structures. A microscope should be available should the digital artery be injured and require repair, or if the nerve has to be coapted. Amputated remnants should be saved. These amputated parts can be used as a source for a skin graft for the tip defect if the flap cannot be used or even as the donor defect of the flap. The risks of the procedure should be explained to the patient and family. Patients need to understand that if the flap fails, they may require an amputation, as well as other risks such as loss of extension, cold intolerance, swelling, and loss of some sensation.
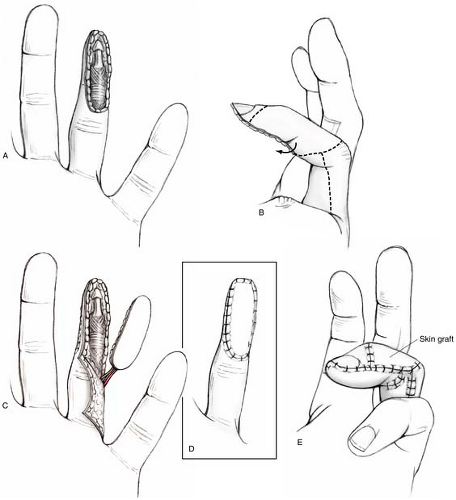 FIGURE 22-2 A,B:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|