Hip Arthroscopy for Nonstructural Pathology
Sean Mc Millan
Joseph McCarthy
Elizabeth Ford
INTRODUCTION
Arthroscopy of the hip joint has become one of the fastest growing surgical procedures in the past decade. As the pursuit of addressing pathology of the hip joint via a minimally invasive technique has progressed, the understanding of the actual disease processes of the femoral-acetabular joint and its surrounding musculature has risen. Much has been written recently regarding methods to classify problems around the hip joint in an effort to streamline the diagnosis and treatment algorithm. Examples of this include labeling pathology according to location (Table 6-1) or as structural versus nonstructural (1).
Femoral acetabular impingement (FAI) of the hip has gained tremendous notoriety within recent literature (2,3). The author prefers to separate hip arthroscopy globally into a “pre and post” understanding of FAI. In early hip arthroscopy, the bony abnormalities of FAI were often not well understood. As such, routine hip arthroscopy did not address underlying bony impingement, even if present (4). Failure to address significant cam or pincer deformity may have contributed to a higher than acceptable progression of osteoarthritis and ultimately conversion to total hip arthroplasty (4,5). However, as the field has advanced, a better understanding of the structural relationship between the morphologic abnormalities of the femoral head/neck and the acetabulum has helped shed light upon the injuries seen relating to nonstructural disease. For the purposes of this chapter, we shall be focusing on issues that can be addressed via arthroscopy pertaining to nonstructural pathology of the hip joint.
Nonstructural pathology of the hip is a wide-ranging category of soft tissue, cartilage, and synovial disorders that effectively encompasses all disease processes not related to bony abnormalities. As indicated above, however, there is a vast interplay and overlap between structural and nonstructural disorders. Commonly seen nonstructural disorders include the spectrum of coxa saltans, gluteus medius tears, labral pathology, and bursitis (Table 6-2).
INDICATIONS
In many instances, soft tissue disorders of the hip can be managed in a conservative manner. It is extremely important during the patient workup to determine the duration of the pain, location of the pain, and provocative factors. In many instances, there is concomitant pathology associated with the presenting disorder that must be addressed, such as leg length discrepancies, sports hernias, muscular imbalance, and/or lumbar spine disease. A proper core-strengthening program coupled with adequate stretching can oftentimes negate the need for surgical intervention.
The most common indication for arthroscopic intervention for nonstructural hip pathology is persistent pain that has failed conservative measures. In general, the best indication for surgical intervention is recalcitrant hip pain with an identifiable etiology, particularly in patients without gross osteoarthritis. In some instances, concomitant procedures may be performed at the time of the hip arthroscopy to address the full spectrum of the hip pathology. The majority of the contraindications,
for hip arthroscopy, aside from gross osteoarthritis or infection are structural in nature. Examples of this include moderate or severe acetabular dysplasia, coxa magna, Brooker 3 or 4 heterotopic bone, and excessive acetabular version (6).
for hip arthroscopy, aside from gross osteoarthritis or infection are structural in nature. Examples of this include moderate or severe acetabular dysplasia, coxa magna, Brooker 3 or 4 heterotopic bone, and excessive acetabular version (6).
TABLE 6-1 Hip Pathology: Location Based | |
|---|---|
|
TABLE 6-2 Nonstructural Pathology of the Hip | |
|---|---|
|
PREOPERATIVE PLANNING
As with any orthopedic procedure, the hallmark of successful surgical intervention begins with matching proper patient selection with the proper procedure. The key to this success lies in the preoperative planning process. Once the patient history has directed the physician toward a specific pain generator location, a decision tree can begin that allows a broad spectrum of pathology to be narrowed to a small field. This in turn allows for an increase in successful outcomes.
A concentrated physical examination of the hip and the surrounding structures can help identify pathology such as lumbar disc disease, sports hernias, tight musculature, or mechanical symptoms. The authors recommend using reproducible provocative testing to ensure proper identification. Examples of these include flexion-adduction-internal-rotation testing (FADDIR) for impingement, McCarthy’s test for labral tearing, OBER’s test for illiotibial band (ITB) dysfunction, and a version of the flexion-abduction-external-rotation test (FABER) for internal snapping hip (7).
Once the examination is completed, appropriate radiographs can be ordered. It is imperative to have true, nonrotated, radiographs. This is particularly useful when investigating for bony abnormalities. Standard hip series radiographs for the authors include an AP pelvis, a false-profile view of the hip, and a Dunn view lateral. Additional radiographs of the lumbar spine are ordered if there is suspicion of concomitant pathology (8,9).
Noncontrast MRI has a limited ability to identify intra-articular pathology, and thus, the authors prefer the use of a gadolinium-enhanced MRI arthrogram. The arthrogram allows for better visualization of labral tears, loose bodies, ligamentum injuries, and identification of cartilage lesions. It should be pointed out, however, that the severity of cartilage pathology remains the most difficult lesion to accurately identify preoperatively. As such, careful examination of the plain radiographs for joint space preservation, in conjunction with the MRI arthrogram, is critical during preoperative evaluation. The absence of radiographic osteoarthritis has been shown to have a favorable effect on outcome after hip arthroscopy (10). The addition of an intra-articular anesthetic during the arthrogram has demonstrated some benefit in localizing joint pathology versus extra-articular sources (11). The lead author routinely requests either lidocaine or Depo-Medrol be added to the arthrogram injection; however, it should be noted that there is some debate regarding the risk of postoperative infection after intra-articular steroid injections.
Other adjunct imaging includes CT scanning with 3D reconstruction and ultrasound evaluation. CT scanning has been helpful in identifying structural abnormalities of the femoral head and acetabulum (12). Controversy remains over its benefit versus risk when considering the patient population and radiation risk. Dynamic ultrasound evaluation of the iliopsoas and the ITB has grown in popularity. Past limitations of this imaging modality were primarily linked to the technical expertise of the examiner; however, as the growth of the diagnostic ultrasonography for orthopedic use has exploded, these interpretive limitations appear to be disappearing (13,14).
SETUP AND POSITIONING
Hip arthroscopy is routinely performed in either the supine or the lateral position (15,16,17). The authors primarily utilize the lateral position; however, the supine position is also utilized depending on facility and equipment availability. Various commercial tables are available for either position, or, if necessary, a standard fracture table will suffice. A soft boot is applied to the operative foot and a well-padded perineal post is placed against the inner thigh of the operative leg to avoid perineal injury. Manual hand traction of 25 to 50 pounds is applied and maintained during the intra-articular portion of the procedure. Traction time should not exceed 90 minutes in order to limit risk of sciatic nerve injury. General or spinal anesthesia may be utilized for the procedure, with the goals of muscle paralysis and a low mean arterial blood pressure.
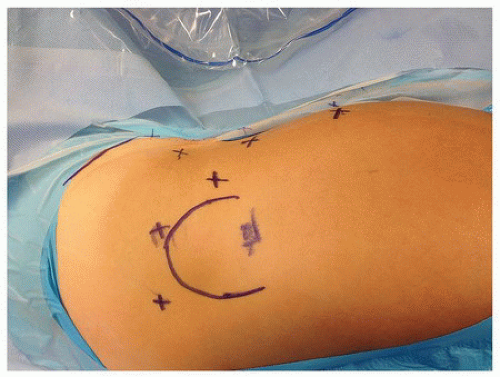
The operating room is set up in order to maximize mobility of the operative leg for evaluation of the static structures during osteoplasty. The author stands on the side of the operative leg with the C-arm brought across the patient’s body, beneath the table. The majority of the central compartment work is performed using a 70-degree arthroscope utilizing a combination of the anterolateral portal (ALP), mid-anterior portal (MAP), and anterior portal (AP) (Fig. 6-1). Work in the peripheral compartment can be performed utilizing either a 30- or a 70-degree arthroscope. In addition to the standard portals listed above, accessory portals may be employed as well. These portals are discussed below when appropriate.
CENTRAL COMPARTMENT PATHOLOGY
Once the patient has been positioned, fluoroscopy is taken in the AP and lateral position to ensure there is no malrotation of the pelvis. Confirmation of this increases the likelihood of success during osteoplasty procedures. After prepping and draping, a spinal needle is used to identify an ALP under fluoroscopy just off the anterior-superior edge of the greater trochanter (18). Access to the joint is performed carefully using a dilation technique to avoid damage to the articular cartilage and the labrum. The author prefers to utilize a 5.5-mm metal cannula for visualization; however, a 4.5-mm cannula, in conjunction with a posterior portal (PP) outflow, is employed in cases of severe acetabular overcoverage. An MAP is then created referenced off the ALP. This portal is approximately 3 finger’s breadths away on a 45-degree angle from the ALP. If needed, the direct AP is created at the intersection of the anterior superior iliac spine (ASIS) and the top of the greater trochanter. A capsulotomy can be created connecting these portals via use of a capsular blade, an oscillating shaver, or an electrocautery device. The author prefers a capsular blade to minimize loss of tissue for potential repair at the conclusion of the procedure. In order to avoid soft tissue interference during labral repair, it is suggested to switch portals after the initial capsulotomy to ensure that the capsulotomy is complete.
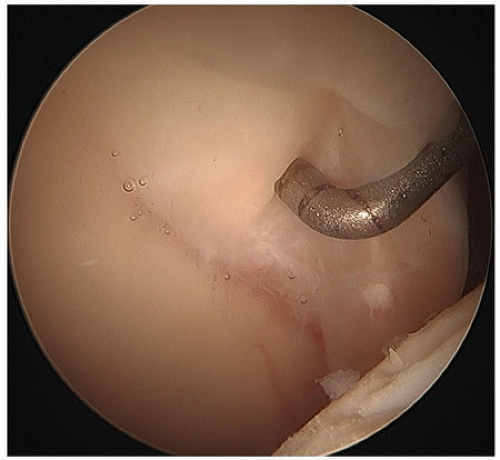
Routine central compartment evaluation is done systematically to avoid missing pathology. The author initially inserts the probe and evaluates the articular cartilage of the femoral head and acetabulum, identifying and documenting potential lesions that may progress, if untreated, to fulminate arthritis. The articular cartilage of the acetabulum is traced up to the chondral-labral junction and probed. Oftentimes, the consequence of femoral cam impingement is the delamination of the chondral labral junction. Upon probing this border, the surgeon will note a “wave sign” (Fig. 6-2; Video 6-1). Treatment of this lesion is discussed below.
Next the acetabular labrum is probed and inspected for instability and/or erythema from the far anterior “5 o’clock” position, up around back to the “9 o’clock” position. If needed, the scope can be repositioned into the AP or PPs, respectively, to obtain appropriate visualization. Proper preoperative planning should make identification of the labral tear location easy as the structural abnormalities of the femoral head and/or acetabulum often correlate with the labral defect. Following this, the deep fovea region of the acetabulum is evaluated. Often, there is disruption of the ligamentum with a large amount of erythematous synovitis noted. Finally, the scope is relocated into the PP (if utilized) and the direct AP to evaluate for foveal loose bodies or chondral defects.
LABRAL PATHOLOGY (SEE VIDEO 6-2)
Within the past decade, there has been a philosophical shift in how labral tears are managed (19,20,21,22




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree