Hip Arthroscopy and the Management of Nonarthritic Hip Pain
Bryan T. Kelly MD
Pete Draovitch PT, AT
Keelan R. Enseki MS, PT
RobRoy L. Martin PhD, PT
Richard Erhardt PhD
Marc J. Philippon MD
History of the Technique
Within the discipline of sports medicine, the hip has received considerably less attention than other joints, largely due to the difficulty that practitioners have traditionally had in assessing intra-articular pathology around the hip. Traditionally, young people with hip pain were given a diagnosis of “early arthritis,” with very little consideration for soft tissue anatomy and injury in and around the joint. Arthroscopic examination of the hip is significantly more challenging than similar surgery around the shoulder and knee, primarily due to the anatomical constraints (Fig. 60-1). The femoral head is deeply recessed in the bony acetabulum and is convex in shape. The thick fibrocapsular and muscular envelopes around the hip joint increase the amount of force required for distention of the hip during arthroscopy; the relative proximity of the sciatic nerve, lateral femoral cutaneous nerve, and femoral neurovascular structures make portal placement more challenging.1,2
Nonetheless, over the past several years hip arthroscopy has begun to gain considerable interest within the orthopedic community. The advent of better diagnostic tools, especially magnetic resonance imaging (MRI), has helped in the detection of intra-articular hip pathology in a more predictable fashion. Technical advances in appropriate portal placement, needle positioning, distraction techniques, and patient set up have all improved the accessibility of the hip joint. New techniques and instrumentation have facilitated the visualization and treatment of these intra-articular lesions by hip arthroscopy. Most notably, the recent adaptation of arthroscopy equipment to create flexible scopes and instruments specifically designed for the hip has led to improved safety, visualization, and accessibility of this joint3 (Fig. 60-2A,B). These improvements in technology have led to a more detailed understanding of the specific intra-articular soft tissue lesions that lead to nonarthritic hip pain. This chapter discusses the current clinical and radiographic methods to detect early hip joint disease and the current indications and surgical techniques of hip arthroscopy.
Indications and Contraindications
Athletes subject their bodies to extreme forces; their lower extremity joint may experience joint reactive forces in excess of five times body weight during activities such as running and jumping.4 The mechanisms of injuries can be from repetitive motion or direct trauma. Subtle radiographic evidence of hip dysplasia or decreased head-neck junction offset may place the athlete at underlying risk for intra-articular injury.5,6,7,8,9 A source of intra-articular pathology should be investigated in patients with unremitting hip pain lasting greater than 4 weeks. The senior author (MJP) has performed over 2,500 hip arthroscopies and has had significant experience with the arthroscopic treatment of elite and amateur athletes from a wide variety of sporting endeavors including: golf, football, ice hockey, baseball, basketball, tennis, skateboarding, gymnastics, weightlifting, ballet, soccer, tae kwon do, Olympic yachting, and figure skating.4,10,11,12
Hip arthroscopy offers a less invasive alternative for hip procedures that would otherwise require surgical dislocation of the hip. In addition, this procedure allows surgeons to address intra-articular derangements that were previously undiagnosed and untreated. In our experience, hip arthroscopy has been very effective for the treatment of numerous athletic injuries including labral tears, capsular laxity with iliofemoral ligament deficiency, femoral-acetabular
impingement and decreased femoral head neck junction offset, lateral impact injury and chondral injuries, injuries to the ligamentum teres, extra-articular conditions (internal and external snapping hip), and loose bodies. Other less common indications for hip arthroscopy include management of osteonecrosis of the femoral head (Avascular Necrosis [AVN]), synovial chondromatosis and other synovial abnormalities, crystalline hip arthropathy (gout and pseudogout), infection, management of posttraumatic intra-articular debris, and in extremely rare cases, management of mild to moderate hip osteoarthritis. In addition, patients with long-standing, unresolved hip joint pain and positive physical findings may benefit from arthroscopic evaluation.3,5,7,8,9,13,14,15,16,17,18,19,20,21,22,23,24 Hip arthroscopy is contraindicated in patients with hip fusions, advanced arthritis, open wounds or cellulitis, obesity, stress fractures in the femoral neck, severe dysplasia, and stable AVN.
impingement and decreased femoral head neck junction offset, lateral impact injury and chondral injuries, injuries to the ligamentum teres, extra-articular conditions (internal and external snapping hip), and loose bodies. Other less common indications for hip arthroscopy include management of osteonecrosis of the femoral head (Avascular Necrosis [AVN]), synovial chondromatosis and other synovial abnormalities, crystalline hip arthropathy (gout and pseudogout), infection, management of posttraumatic intra-articular debris, and in extremely rare cases, management of mild to moderate hip osteoarthritis. In addition, patients with long-standing, unresolved hip joint pain and positive physical findings may benefit from arthroscopic evaluation.3,5,7,8,9,13,14,15,16,17,18,19,20,21,22,23,24 Hip arthroscopy is contraindicated in patients with hip fusions, advanced arthritis, open wounds or cellulitis, obesity, stress fractures in the femoral neck, severe dysplasia, and stable AVN.
Appropriate patient selection is of paramount importance to a successful outcome after hip arthroscopy. Injuries to the hip in athletes are often categorized as muscle strains or soft tissue contusions. However, hip pain, particularly in the young adult, may arise from a number of soft-tissue
structures in and around the hip joint. It is important to be able to differentiate extra-articular from intra-articular pathology. Based upon our clinical experience and review of patient outcomes we have come up with a detailed algorithm for categorizing nonarthritic hip pain (Fig. 60-3). Injuries to the hip are classified based upon the primary soft-tissue problem: labrum, chondral, capsule, extra-articular, or systemic. Within each primary problem, underlying causes or abnormalities are identified. This comprehensive assessment algorithm provides a rational approach to patient evaluation and improves clinical decision making and treatment plans.
structures in and around the hip joint. It is important to be able to differentiate extra-articular from intra-articular pathology. Based upon our clinical experience and review of patient outcomes we have come up with a detailed algorithm for categorizing nonarthritic hip pain (Fig. 60-3). Injuries to the hip are classified based upon the primary soft-tissue problem: labrum, chondral, capsule, extra-articular, or systemic. Within each primary problem, underlying causes or abnormalities are identified. This comprehensive assessment algorithm provides a rational approach to patient evaluation and improves clinical decision making and treatment plans.
Labral Injury
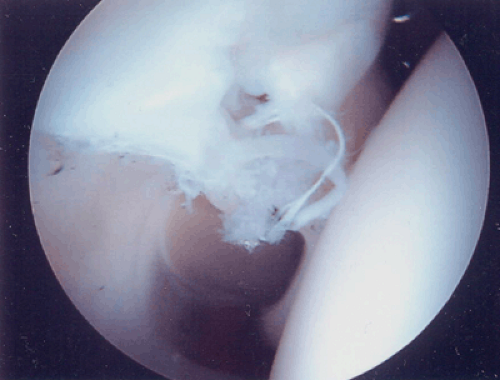
In our experience, injuries to the labrum are the most common source of hip pain identified at the time of arthroscopy. In the review of 300 recent cases, labral tears were present in 90% of them (Fig. 60-4). Dynamic forces acting across the injured hip will result in hip pain, decreased athletic performance, and limitations in activities of daily living. The diagnosis of a labral tear remains largely clinical and is analogous to those patients who present with meniscal pathology. These patients often present with mechanical symptoms (catching and painful clicking) as well as restricted range of motion. Sometimes their presentation is more subtle, with symptoms of dull, activity-induced, positional pain that fails to improve with rest.20,25 Classic symptoms of hip clicking
may be misdiagnosed as a labral tear when the etiology is in fact from a different source (snapping iliotibial band tendon or a hypermobile psoas tendon). Patients who have persistent hip pain for greater than 4 weeks, clinical signs, and radiographic findings consistent with a labral tear are candidates for hip arthroscopy. No radiographic study, however, including high-contrast gadolinium-enhanced arthrography MRI scanning, is entirely sensitive or specific in the detection of labral tears.26 Thus, a high clinical suspicion of positive physical findings is essential for proper treatment.
may be misdiagnosed as a labral tear when the etiology is in fact from a different source (snapping iliotibial band tendon or a hypermobile psoas tendon). Patients who have persistent hip pain for greater than 4 weeks, clinical signs, and radiographic findings consistent with a labral tear are candidates for hip arthroscopy. No radiographic study, however, including high-contrast gadolinium-enhanced arthrography MRI scanning, is entirely sensitive or specific in the detection of labral tears.26 Thus, a high clinical suspicion of positive physical findings is essential for proper treatment.
In order to effectively treat patients with labral tears, the underlying cause of the labral injury must be identified. Based upon our clinical experience and comprehensive review of 300 recent cases, we have identified at least five causes of labral tears: (a) trauma, (b) laxity/hypermobility, (c) bony impingement, (d) dysplasia, (e) degeneration. Capsular laxity or hypermobility of the hip is the most common underlying cause for labral injury in our experience, resulting in 34% of the cases.3,27 Femoral-acetabular impingement is the second most common cause for labral injury and was the underlying cause in 33% of the reviewed cases. Bony impingement can result from decreased femoral head neck junction offset (CAM effect), overhang of the anterior superior acetabular rim (pincer lesion), a retroverted acetabulum, or a combination of these bony deformities.5,7,8,9,28 Specific traumatic events such as twisting, falling, or other lower extremity loads may precede the onset of symptoms. However, isolated traumatic labral tears were less common overall (14%), although they were the most common type of tears seen in high level athletes.
It has been shown that labral tears are associated with acetabular dysplasia.29,30 In our practice, this subgroup of patients represented 5% of the labral tears seen at the time of arthroscopy. Although Byrd and Jones29 report that the results of hip arthroscopy in the presence of dysplasia compare favorably with the results reported for the general population, we believe that extreme dysplasia (center edge angle <17 degrees) is a contraindication to the procedure. The final factor commonly associated with the presence of a labral tear is global hip joint degeneration. Degenerative labral tears were present in 11% of the patients in our series. Isolated treatment of labral tears without addressing the underlying causative factor will likely result in poor outcomes. These associated causative factors must be identified preoperatively and treated appropriately at the time of surgery.
Chondral Injury
Although chondral injury is an appropriate indication for hip arthroscopy, these lesions can be an elusive source of hip pain.31,32 Traditionally, chondral damage around the hip has been associated with either progressive joint deterioration (osteoarthritis or rheumatoid arthritis) or trauma. However, acute isolated traumatic articular surface injuries can occur from impact loading across the hip joint. There appears to be a particular propensity for this injury pattern in young physically fit adult males who suffer impact loading over the greater trochanter in association with sport or activity. The so-called lateral impact injury occurs following a blow to the greater trochanter, which, due to its subcutaneous location, has minimal ability to absorb large forces. The high bone density of this region allows impact on this area to transfer energy and load to the joint surface, resulting in chondral lesions of the femoral head or acetabulum without associated osseous injury. Arthroscopic findings in this clinical scenario will commonly support this lateral impact mechanism.32
In most cases of chondral injuries in the hip joint, symptom onset is immediate; however, in some cases the injury will appear innocuous with variable associated dysfunction. Persistent symptoms such as intermittent catching or pain elicited by provocative maneuvers should prompt a more extensive diagnostic workup. Although gadolinium-enhanced MR arthrography is currently the most promising imaging modality, it still has some limitations in reliably demonstrating chondral injuries perhaps due to the static nature of the imaging study and the lack of hip joint distraction during the test. Potter et al.33 have demonstrated the utility of cartilage sensitive MRI for the detection of these lesions, which can be performed successfully without the use of gadolinium.
Primary chondral sources of intra-articular hip pain may also be due to loose bodies or synovial chondromatosis. Removal of these cartilaginous loose bodies can be successfully performed arthroscopically with very satisfying results. Focal AVN may be treated effectively with hip arthroscopy if the lesion is identified prior to collapse. In these cases, arthroscopically assisted core drilling and bone grafting can be performed to revascularize the necrotic region. Arthroscopic evaluation of the core tract allows for a direct assessment of the presence of bleeding bone.
Capsule Pathology
Hip instability can be a difficult disorder to diagnose and can be of traumatic or atraumatic origin. Professional athletes may develop overuse injuries of the hip from abnormal stresses on normal anatomy resulting in hip pain with associated subtle rotational hip instability.3,4,12 Injuries or soft-tissue abnormalities such as labral tears or iliofemoral ligament insufficiency can disturb the complex buffer mechanism in the hip and result in increased tension in the joint capsule and its ligament and decreased ability to absorb stress or overstress.
Instability of the hip joint is much less common than in the shoulder, but can be a source of great disability. The hip joint relies much less on its adjacent soft tissue for stability because of the intrinsic osseous stability. It is apparent that any deviation from “normal” bony anatomy will lead to more dependence on the capsular tissue and labrum for stability. The labrum helps to contain the femoral head in extremes of range of motion, especially flexion. The labrum and capsule also act as load-bearing structures during flexion, causing a hip with a deficient labrum to be subject to instability if capsular laxity is present.3,27 Takechi et al.34 have demonstrated that the labrum may enhance stability by providing negative intra-articular pressure in the hip joint. Ferguson et al.35,36 have further identified a stabilizing role of the labrum using a poroelastic finite element model to demonstrate that the
labrum provides some structural resistance to lateral and vertical motion of the femoral head within the acetabulum and helps to form a suction seal around the femoral head (Fig. 60-5). Since the labrum appears to enhance joint stability and preserve joint congruity, there is a significant concern about the potential for rotational instability or hypermobility of a hip associated with a deficiency of labral tissue. This instability may result in redundant capsular tissue and create a potential abnormal load distribution due to a transient incongruous joint resulting from subtle subluxation.3
labrum provides some structural resistance to lateral and vertical motion of the femoral head within the acetabulum and helps to form a suction seal around the femoral head (Fig. 60-5). Since the labrum appears to enhance joint stability and preserve joint congruity, there is a significant concern about the potential for rotational instability or hypermobility of a hip associated with a deficiency of labral tissue. This instability may result in redundant capsular tissue and create a potential abnormal load distribution due to a transient incongruous joint resulting from subtle subluxation.3
 Fig. 60-5. View of the normal suction seal of the labrum on the femoral head with the traction released. |
Even less common than hypermobility of the hip is global capsular tightness. These patients present with a capsular pattern of decreased motion and closely resemble the clinical findings associated with adhesive capsulitis of the shoulder. They typically have significant synovitis associated with their decreased motion. Nonoperative management should be the mainstay of treatment for these patients, focusing on physical therapy to regain motion and anti-inflammatory medications to decrease the inflammation. Fluoroscopically guided corticosteroid injections directly into the hip joint may help decrease the local inflammation. If patients are unresponsive to nonoperative treatment, they may be considered for arthroscopic capsular release; however, we have mixed results in these cases.
Extra-articular Sources of Pain
Extra-articular sources of hip pain are perhaps more common than intra-articular sources. A thorough evaluation is necessary to identify any associated extra-articular problems prior to the time of arthroscopy. Sources of extra-articular hip pain include: internal snapping hip (iliopsoas over the iliopectineal eminence); external snapping hip (iliotibial band over the greater trochanter); trochanteric and ischial bursitis; chronic tendonitis involving the hip flexors, adductors, and abductors; gluteus medius tears; osteitis pubis and sports hernia; piriformis syndrome; SI joint dysfunction; pelvic obliquity; leg length inequality; and referred pain from sources including the back, genitourinary, and endometriosis.
Systemic Sources of Pain
Systemic sources of hip pain include complex regional pain syndrome or reflex sympathetic dystrophy, rheumatoid arthritis, polyarticular arthritides, diabetes, and hormonal factors. Identifying a systemic cause of the hip pain should lead the treating surgeon away from surgical intervention, unless a discreet mechanical factor is identified.
Clinical Exam
Prior to a formal history and physical examination, all patients complete pre-evaluation subjective questionnaires to report the location and nature of the symptoms, as well as the intensity of the symptoms over the prior 24 hours (Appendices 1, 2, and 3). A comprehensive patient history should be performed to assess the qualitative nature of the discomfort (pain, clicking, catching, instability, stiffness, weakness, or decreased performance), the specific location of the discomfort, the timing of the onset of symptoms, the precipitating cause of the symptoms, and assessment of any referred or systemic causes of hip pain (Appendix 4).37,38,39 An intra-articular etiology causing intractable hip pain in the adult can present in a variety of ways. Patients may have pain in the anterior groin, anterior thigh, buttock, greater trochanter, or medial knee. Other symptoms include persistent clicking, catching, locking, giving way, or restricted range of motion. Symptoms may be preceded by a traumatic event, either a fall or twisting injury; however, insidious onset of hip pain may also be reported. Symptoms are typically exacerbated with activity and improved with rest.
A comprehensive physical examination form may be used to record all findings (Appendix 4). The initial portion of the exam should assess the patient’s gait and posture and is best performed when the patient is unaware that they are being watched. Antalgic gait patterns result in shortening of the stance phase, as well as shortening of the length of the step on the affected side secondary to pain. During a Trendelenburg gait, functionally or physiologically weakened gluteus medius forces shift the upper body to the involved side so as to move the center of gravity over the painful hip and decrease the moment the arm forces across the hip joint.40 Evaluation of posture and limb position should look for pelvic obliquity, limb length inequality, muscle contractures, and scoliosis and includes both static and dynamic evaluations.39 Iliac crest heights are determined in both the standing and sitting positions for the purpose of differentiating pelvic obliquity from leg length inequality. Several lumbar movements are performed after a base line of symptoms is established to determine if the lumbar motions elicit any of the symptoms. If suspicion is present for lumbar involvement, lower extremity deep tendon
reflexes and manual muscle testing should be performed in the seated and supine position. Straight leg testing and femoral nerve stretch testing should be performed to rule out a radicular source of pain.
reflexes and manual muscle testing should be performed in the seated and supine position. Straight leg testing and femoral nerve stretch testing should be performed to rule out a radicular source of pain.
Examination of the hip joint itself begins with palpation of specific regions of the hip to localize sites of tenderness, to delineate the integrity of the muscular structures about the hip, and to identify any areas of gross atrophy. If the source of the pain is truly intra-articular, palpable pain can rarely be elicited. Active and passive range of motion of both hips should be evaluated in the seated and supine positions. Any asymmetry in adduction, abduction, flexion, extension, external rotation, and internal rotation should be noted as well as any reproduction of symptoms in these positions.
Several tests can be exercised to identify specific hip pathology. The Thomas test will help to identify the presence of a hip flexion contracture by eliminating the effects of excessive lumbar lordosis on the perceived extension of the hip.40 Typically, passive range of motion should match or exceed active range of motion; however, provocative maneuvers performed during passive range of motion evaluation may result in limited motion secondary to pain and are highly suggestive of intra-articular pathology. Painful hip flexion, adduction, and internal rotation can indicate acetabular rim problems or labral tears, especially if clicking or groin pain is present. The Faber test involves flexion, abduction, and external rotation of the hip and suggests sacroiliac pathology or iliopsoas spasm. The Ober test is used to evaluate tightness in the iliotibial band and may elicit symptoms in the presence of trochanteric bursitis. The test is positive when the leg remains in the abducted position after the hip is passively extended and abducted with the knee extended. The piriformis test is performed by flexing the hip to 60 degrees, stabilizing the hip, and exerting a downward pressure on the knee. If the piriformis is tight, pain is elicited; and if the sciatic nerve is compressed (piriformis syndrome), the patient experiences radicularlike symptoms.39,40 Mechanical symptoms attributable to intra-articular pathology can also be elicited by loading the hip joint with both a resisted leg raise in the supine position as well as forced internal rotation while applying an axial load. Both of these maneuvers can load the hip joint anterolaterally, which is the most common location for labral tears.
The complete physical examination should include motor strength testing of both hips in order to detect subtle differences from side to side. Finally, a neurovascular examination should be performed to rule out referred pain secondary to radicular symptoms or vascular etiology. In most patients, hip pain goes away over time if the patient complies with conservative treatment. If a patient’s hip pain persists, is reproducible on physical examination, and does not respond to appropriate conservative measures (including rest, ambulatory support, nonsteroidal anti-inflammatory drugs, and physical therapy), hip arthroscopy may be of substantial value.41,42 A subset of patients may have persistent symptoms despite negative or uncertain radiographic studies. Arthroscopy can lead to definitive diagnoses such as focal degenerative arthritis, chondromalacia, chondral flap tears, nonossified loose bodies, synovitis, labral lesions, and synovial chondromatosis in as many as 40% of these cases.21,43
All patients undergo a standard series of plain x-rays including standing anteroposterior (AP) pelvis, cross-table lateral of the involved hip, and a 90-degree flexion lateral. The main purpose of plain x-rays is to rule out significant joint space narrowing, the presence of acetabular dysplasia, and the presence of femoral-acetabular impingement. Radiographic indices should include the center-edge angle and the Sharp angle. If acetabular dysplasia is suspected, a false-profile view may be obtained to look for loss of anterior coverage.44
MRI has become the examination of choice for the evaluation of unexplained hip pain. Its unique ability to provide detailed images of soft tissue and marrow-based abnormalities in multiple planes of view makes it superior to other modalities employed in intra-articular hip imaging. Gadolinium-enhanced MR arthrography of the hip may be performed when evaluation of the capsulolabral structures or articular surfaces is most important. Intra-articular injection of 10 to 15 cc of gadolinium solution, followed by routine MRI may increase the sensitivity and specificity of detecting intra-articular hip pathology.38,44 Czerny et al.45 compared conventional MRI with MR arthrography in the diagnosis of labral tears. They reported a sensitivity and accuracy of 80% and 65% for conventional MRI compared to 95% and 88% with MR arthrography. Results such as these suggest that MR arthrography may have a significant advantage over conventional MRI for the evaluation of capsulolabral structures in the hip. More recent cartilage imaging methods, described by Potter et al.,33 may obviate the need for intra-articular gadolinium in the MRI detection of chondral lesions of the hip.
Surgical Techniques
Hip arthroscopy may be performed in either the supine or lateral position depending upon surgeon preference. In either case, distraction of the femoral head from the acetabulum must be performed to fully visualize the articular surfaces. Either general or spinal anesthesia may be used; however, it is necessary to maintain complete skeletal muscle relaxation at all times to minimize the amount of traction force required for distraction. A thorough understanding of the anatomic relationships around the hip joint with special attention to neurovascular structures and tissue planes is of paramount importance. Specialized instruments including flexible probes, extra long cannulas, and extra long specialized instruments such as shavers, burs, drills, and loose body retrievers; all have improved accessibility of the joint and increase the versatility of procedures available to the surgeon (Fig. 60-2A,B). Initial insertion of long spinal needles
(6-inch 16 gauge) allows release of the negative pressure vacuum phenomenon created with joint distraction and also allows for injection of sterile saline for joint distention.
(6-inch 16 gauge) allows release of the negative pressure vacuum phenomenon created with joint distraction and also allows for injection of sterile saline for joint distention.
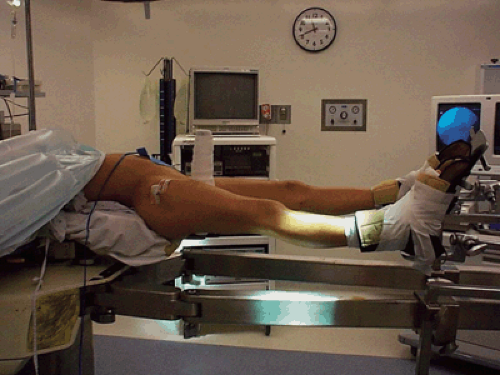 Fig. 60-6. The modified supine position: the hip is in 10 degrees flexion, 15 degrees internal rotation, 10 degrees lateral tilt, and neutral abduction. |
We perform hip arthroscopy in the modified supine position in which the hip is placed in a position of 10 degrees flexion, 15 degrees internal rotation, 10 degrees lateral tilt, and neutral abduction (Fig. 60-6). A minimum of 8 to 10 mm of distraction is recommended to avoid any iatrogenic injury to the chondral surfaces or labrum. Adequate traction typically requires between 25 and 50 lb of force (Fig. 60-7).31 Gentle countertraction is also applied to the contralateral limb. All of the intra-articular structures in the hip joint can be seen through the combined use of 70- and 30-degree arthroscopes as well as by the interchange of portals.20
 Fig. 60-7. Fluoroscopic view of the hip after adequate traction has been applied. A minimum of 8 to 10 mm is necessary to avoid iatrogenic injury to the cartilage surfaces or the labrum. |
Portal Placement
Accurate portal placement is essential for optimal visualization of all intra-articular structures and safe access to the hip joint. Typically, three basic portals are used: anterolateral, anterior, and posterolateral (Fig. 60-8A,B). The vast majority of procedures performed within the joint can be accomplished with just two portals: the anterolateral and the anterior. Two accessory portals (proximal lateral and distal lateral) are useful for releases of the iliotibial band (ITB) and osteochondroplasty for decreased head-neck junction offset respectively.
Anterolateral Portal
The anterolateral portal has also been described as the anterior paratrochanteric portal as it is referenced off the greater trochanter. This portal is traditionally described as being approximately 1 to 2 cm superior and 1 to 2 cm anterior to the anterosuperior “corner” of the greater trochanter depending upon the patient’s weight and size. In our experience, we have found the portal to be more useful if placed directly off the anterosuperior portion of the greater trochanter. This portal allows for optimal visualization of the iliofemoral ligament, femoral head, anterior superior labrum, ligamentum teres, transverse ligament, and most of the acetabulum. Typically a 70-degree scope is used through this portal for greatest visualization.
Anterior Portal
The anterior portal is typically the second portal to be established and allows for visualization of the posterior-superior capsule, posterior superior labrum, the posterior recess, the femoral head, and the ligamentum teres. This portal is also the optimal location for viewing the head-neck junction, the anterior femoral neck, the zona orbicularis, and the distal insertion of the capsular ligaments on the intertrochanteric line. Again, use of the 70-degree arthroscope will allow for optimal visualization. The portal is established by identifying the intersection of the vertical line drawn from the anterior superior iliac spine distally and the horizontal line drawn from the superior surface of the femoral greater trochanter medially. This portal presents the greatest risk to the lateral femoral cutaneous nerve, which lies within several millimeters of the cannula. In addition, the lateral femoral circumflex artery and femoral neurovascular bundles must be protected.1 Care must be taken not to place this portal too anterior or deep, as this places the femoral neurovascular bundle at risk.46 The localization of the femoral pulse distal to the inguinal ligament helps prevent inadvertent injury to these structures.
Posterolateral Portal
The posterolateral portal is also described as the posterior paratrochanteric portal as it is also referenced off the greater trochanter. The entry site is 2 to 3 cm posterior to the tip of the greater trochanter at the same level as the anterolateral portal. Direct visualization of entry into the joint is possible with the scope in the anterolateral portal. The anterolateral and posterolateral portals should be established parallel to one another. The greatest risk with this portal is injury to the sciatic nerve, which lies within approximately 3 cm.46,47 Advancing the trocar with the femur in a neutral or slightly internally rotated position can protect the nerve, as this maneuver rotates the nerve away from the posterior margin of the greater trochanter. This portal is used for visualization of the posterior aspect of the femoral head, the posterior labrum, posterior capsule, and the inferior edge of the ischiofemoral ligament.1
Proximal Lateral Accessory
The proximal lateral accessory portal is used for ITB releases. It is placed approximately 2 cm distal and in line with the anterolateral portal. The 30-degree arthroscope is placed in the anterolateral portal, and the accessory portal is established as a working portal for additional instruments required for the release. The ITB can be clearly visualized through the anterolateral portal, and the release can be performed under direct visualization through the accessory portal.
Distal Lateral Accessory
The distal lateral accessory portal is used for an osteochondroplasty performed in patients with decreased femoral head-neck junction offset. It is placed at the midpoint between the anterior and anterolateral portals and approximately 4 cm distal. The portal typically enters the capsule at around the level of the zona orbicularis and allows for direct access to the anterior neck. This portal can be established under direct visualization with the 70-degree arthroscope placed in the anterior portal (Fig. 60-9).
Once traction is applied, the anterolateral portal is established under fluoroscopic guidance using the landmarks described above. Immediate visualization of the anterior
triangle is established through this portal (Fig. 60-10). The anterior triangle represents the intra-articular portion of the lateral limb of the iliofemoral ligament. The anterior portal is established under direct visualization, as the spinal needle is directed between the lateral and medial limbs of the Y-ligament (Fig. 60-11).
triangle is established through this portal (Fig. 60-10). The anterior triangle represents the intra-articular portion of the lateral limb of the iliofemoral ligament. The anterior portal is established under direct visualization, as the spinal needle is directed between the lateral and medial limbs of the Y-ligament (Fig. 60-11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree