David B. Weiss, Seth R. Yarboro, James A. Browne
Hip and Pelvis
Regional Anatomy and Surgical Intervals
Regional Anatomy
Osteology
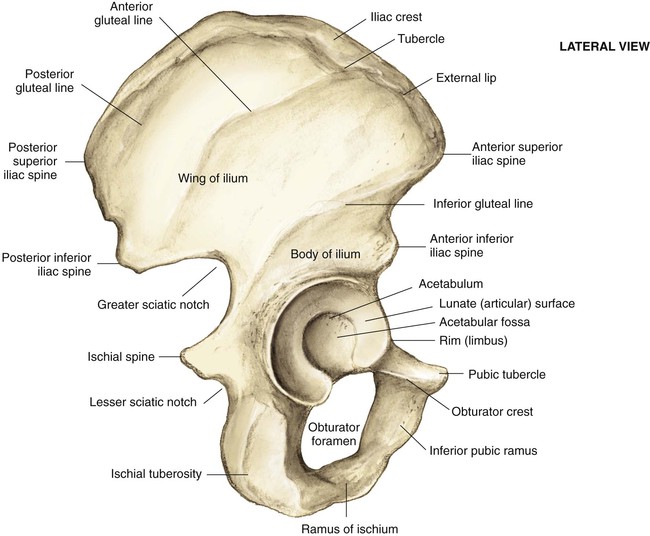
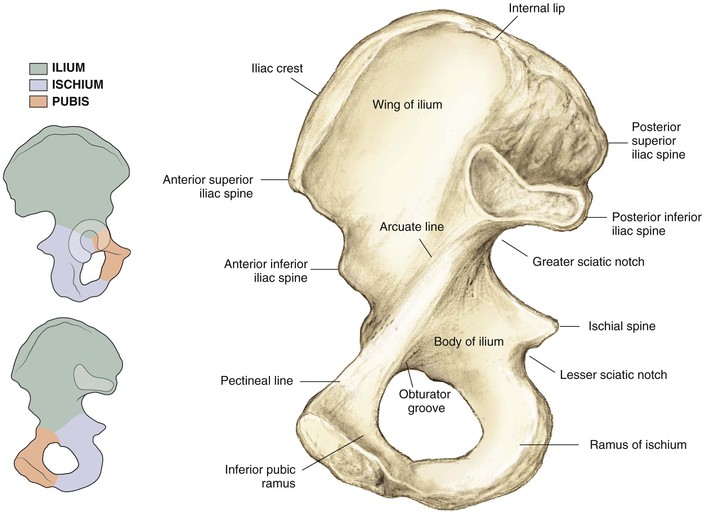
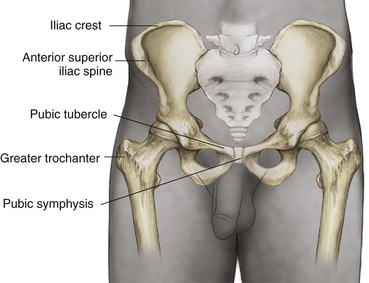
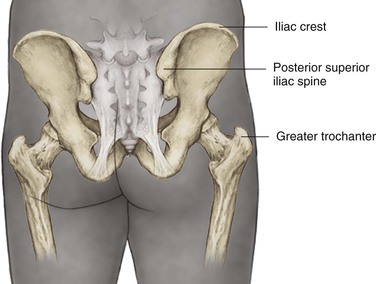
Pelvis (Figs. 6-1 and 6-2)
Iliac crest (palpable throughout its entire length)
• Landmark for several skin incisions
• Iliac tubercle (outer surface of iliac crest about 5 cm posterior to the anterior superior iliac spine [ASIS])
• Site for external fixator pin
• ASIS and posterior superior iliac spine (PSIS)
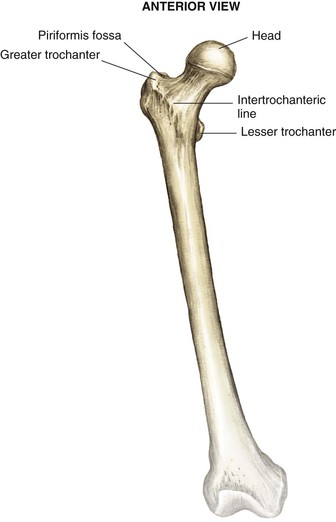
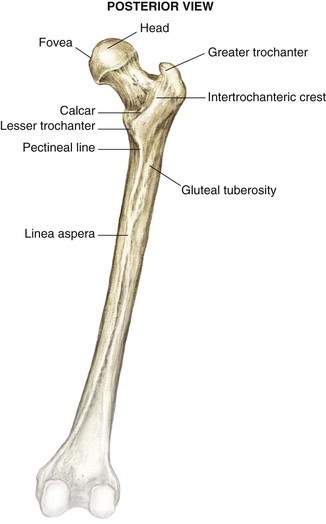
Proximal Femur (Figs. 6-3 and 6-4)
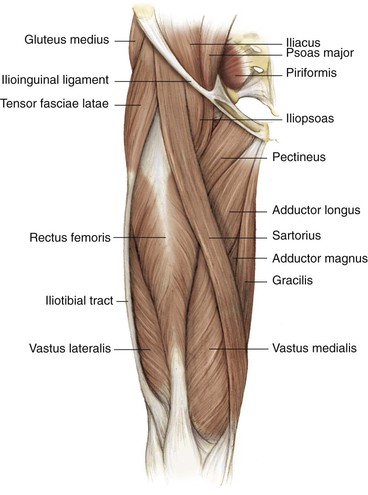
• Greater trochanter (abductor attachment for increased moment arm and mechanical advantage)
• Attachment point for abductor muscles
• Intertrochanteric line (ridge connecting the greater and lesser trochanter)
• Lesser trochanter (insertions of the iliacus and the psoas muscles)
• Posterior to the midaxis of the femoral neck, in line with the medullary canal
• The starting point for some femoral nails
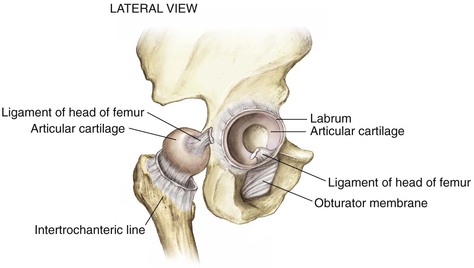
• Fovea (ligament of the femoral head attachment)
• Fractures below this area are out of the weight-bearing surface
Arthrology
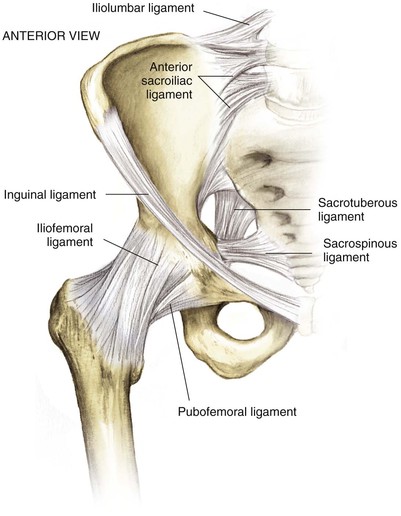
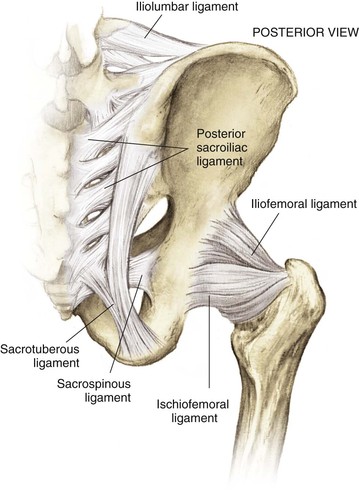
Hip Joint (Figs. 6-5 to 6-7)
Sacroiliac Joint
Small translations of the joint
Largely stabilized by ligaments
• Pelvis and sacroiliac ligament joint stabilizers
• Sacrospinous (connects the lateral part of the sacrum and the coccyx to the spine of the ischium)
• Iliolumbar ligaments (transverse process of the lower lumbar vertebrae to the ilium)
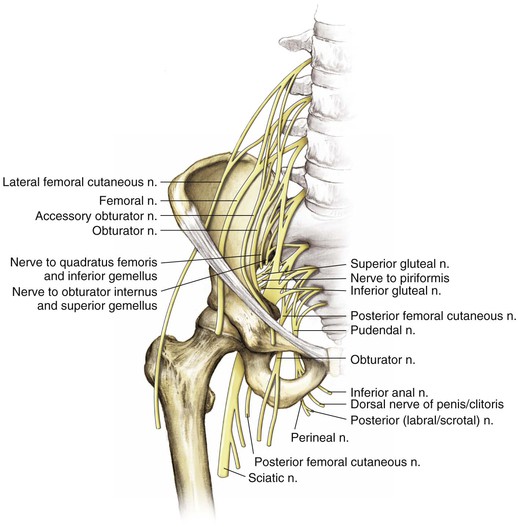
Nerves
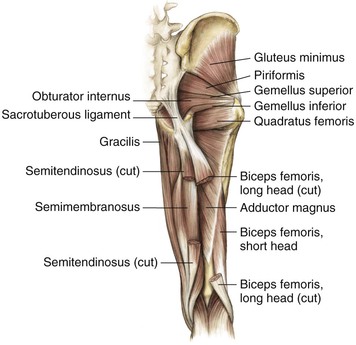
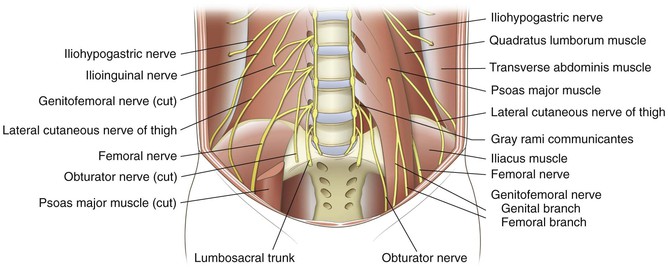
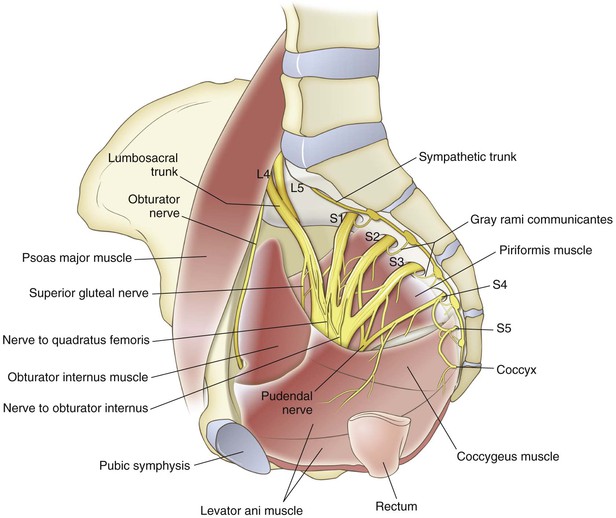
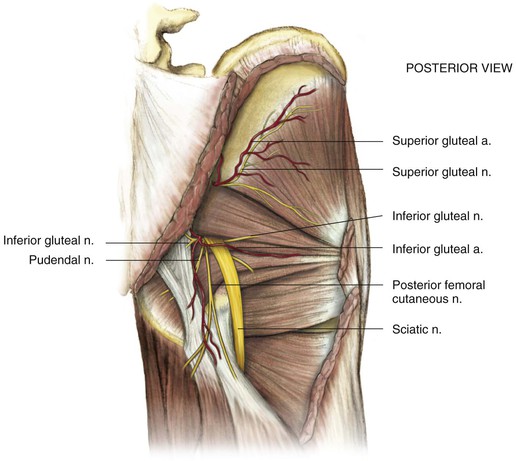
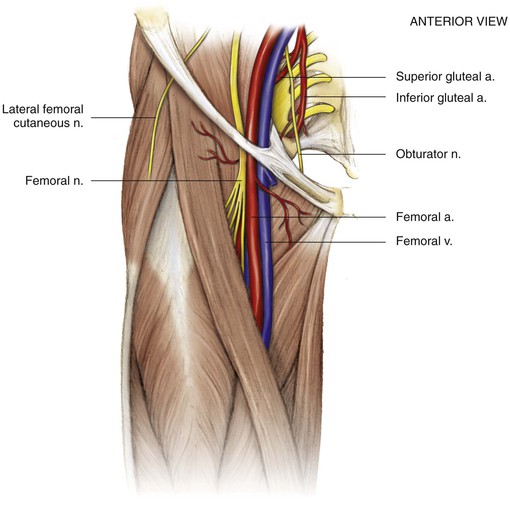
Extension of Nerves from the Lumbosacral Plexus (Fig. 6-14)
• Sciatic nerve (L4 and L5 and S1, S2, and S3)
• Has tibial and peroneal divisions that are indistinguishable around the hip but later divide
• Superior gluteal nerve (innervates the gluteus medius, gluteus minimus, and tensor fasciae latae muscles)
• A risk of injury exists with extensive superior and medial dissection above the GSN
• Inferior gluteal nerve (innervates the gluteus maximus)
• Exits the GSN inferior to the sciatic nerve and enters the gluteus maximus
• Is at risk with extensive medial dissection around the posterior column near the GSN
• Lateral femoral cutaneous nerve
• Exits the pelvis just medial to the ASIS (with wide variation up to 3 cm to either side)
• Provides pure sensory innervation to anterolateral thigh
• Femoral nerve (largest branch L2, L3, and L4)
• Exits the pelvis over the anterior wall of the hip and lateral to the femoral artery and vein
• Is at risk with anterior retractor placement during anterior and posterior approaches to the hip and during middle window dissection and retraction for ilioinguinal approaches
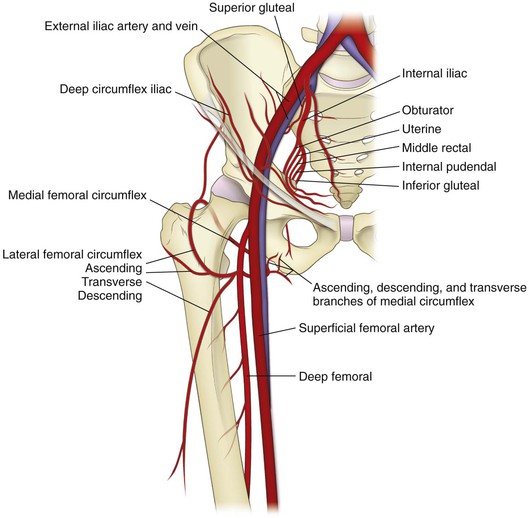
Vascularity (Fig. 6-15)
Internal Iliac Artery
Primarily supplies the pelvic floor musculature
• Exits the greater sciatic notch and supplies the gluteus medius and minimus
• Can be damaged during posterior approaches to the hip/acetabulum
• Travels along the true pelvis and quadrilateral plate
• Corona mortis must be ligated during ilioinguinal or Stoppa approaches to the pelvis
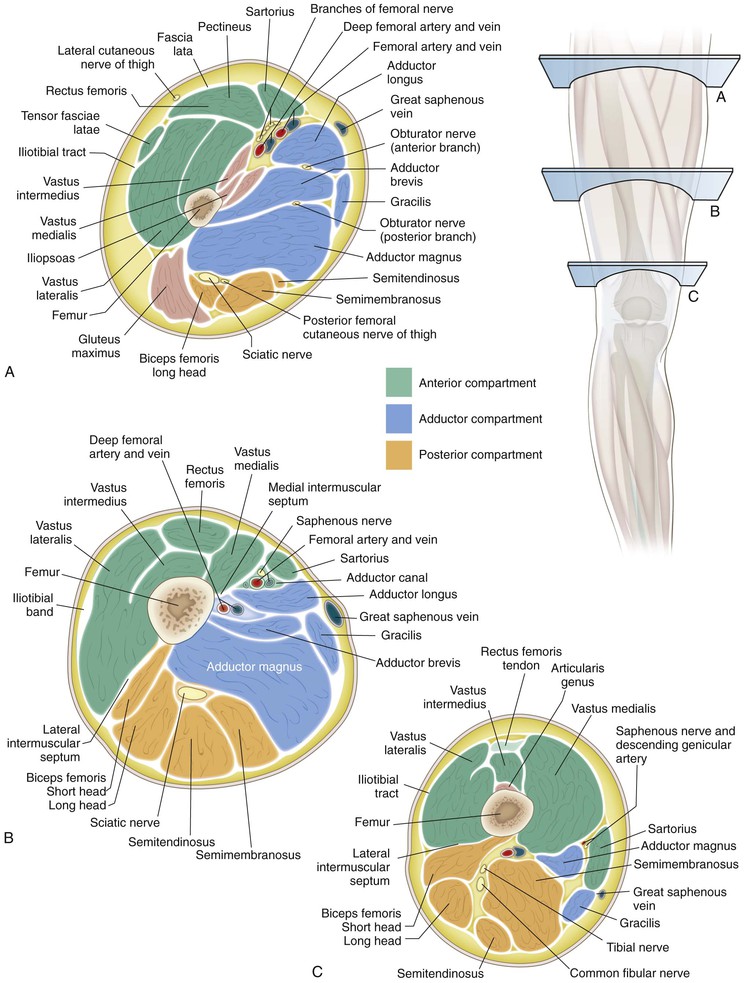
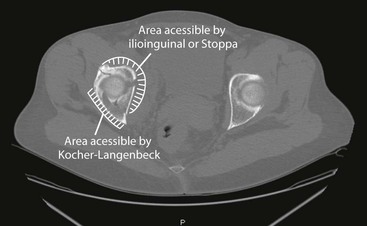
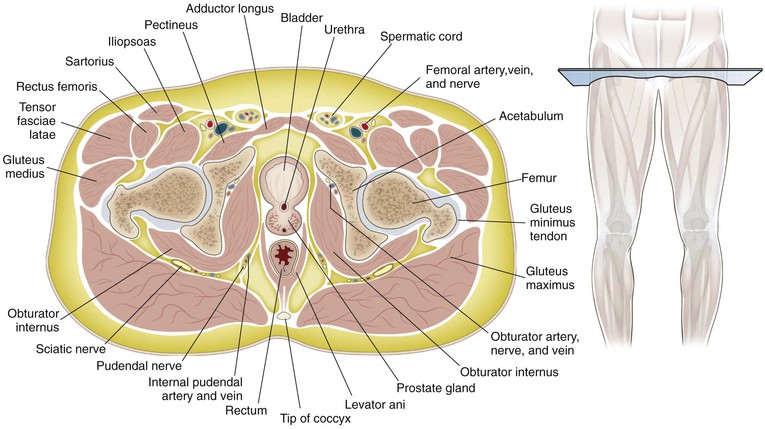
Cross-Sectional Anatomy (Figs. 6-16 to 6-19)
Hazards (Figs. 6-20 and 6-21)
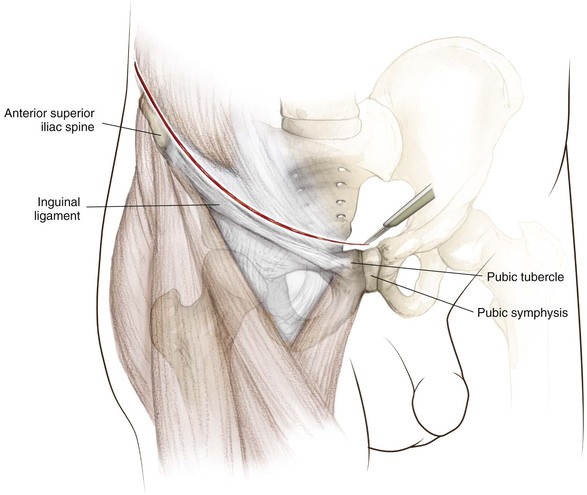
Femoral Triangle
Bordered by the inguinal ligament, sartorius, and the adductor longus, the structures from lateral to medial consist of the femoral nerve, artery, vein, and lymphatics (see Fig. 6-20)
Surgical Approaches to the Pelvis
Posterior Approach to the Sacroiliac Joint
Indications
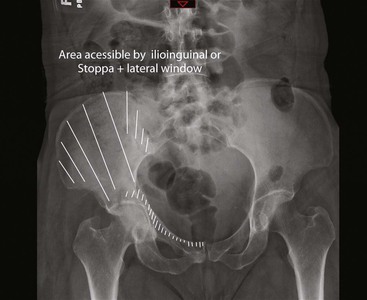
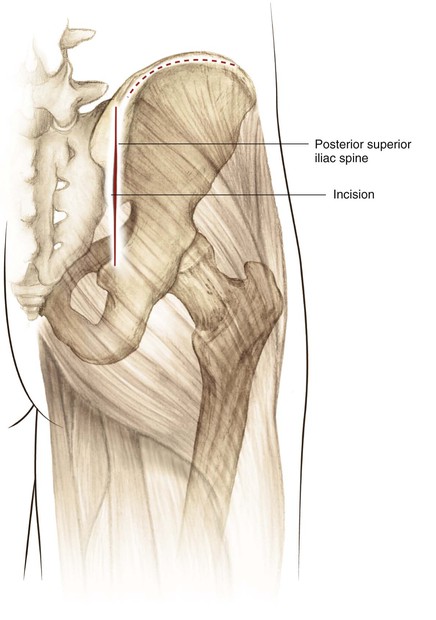
Incision (Fig. 6-27)
The incision is 8 to 12 cm centered 2 to 3 cm below and slightly lateral to the PSIS (Fig. 6-28)
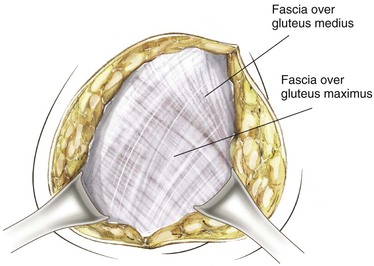
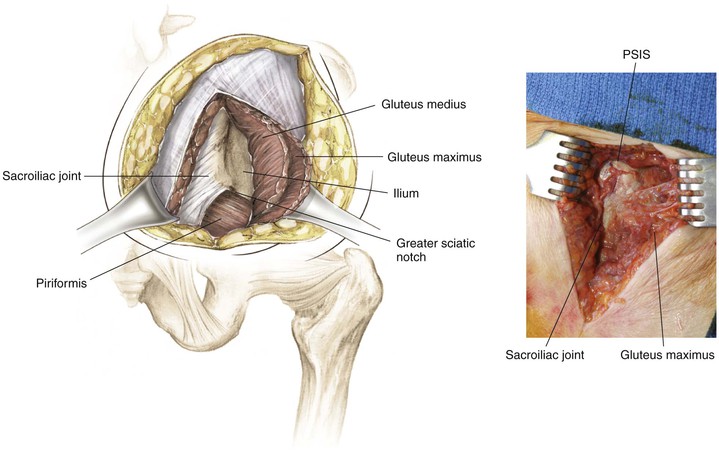
• Incise the fascia of the maximus over the crest of the ilium
• This maneuver uncovers the gluteus medius and the piriformis emerging from the greater sciatic notch (the superior gluteal nerve and artery are emerging as well; Fig. 6-29)
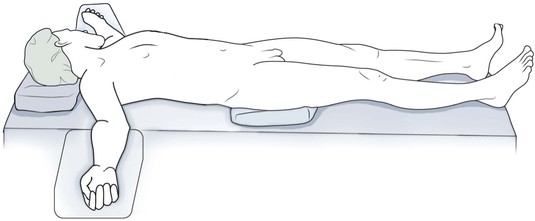
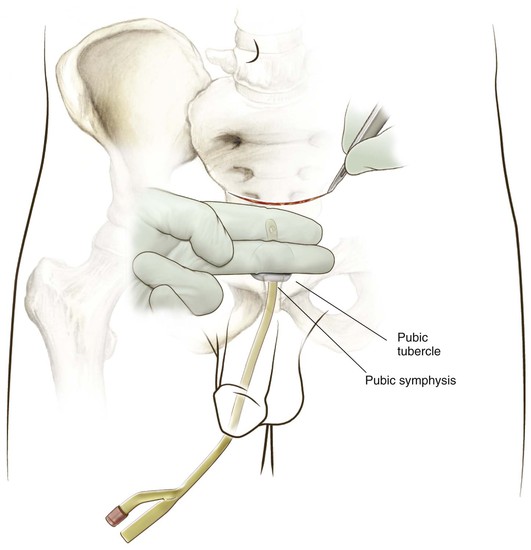
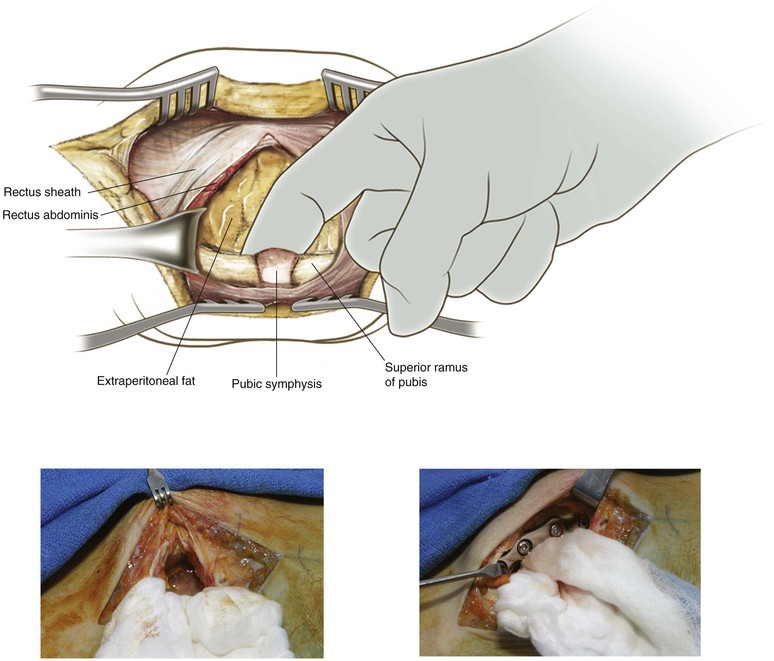
Anterior Approach to the Pubic Symphysis (Video 6-1)
Indication
Superficial Dissection
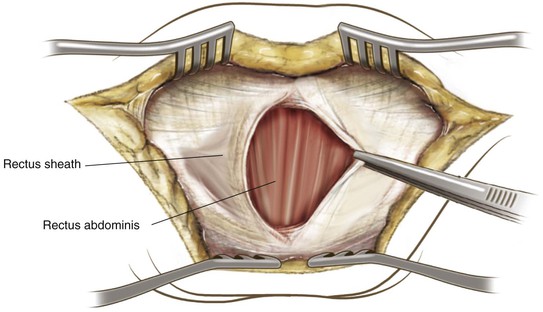
Deep Dissection Midline
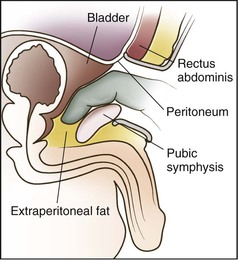
Retract the rectus abdominis laterally and superiorly
A layer of extraperitoneal fat may be present between the rectus abdominis and the bladder
Dissection of the posterior aspect of the superior rami and pubic symphysis can be accomplished digitally (preperitoneal space of Retzius; Figs. 6-33 and 6-34)
Ilioinguinal Approach to the Pelvis (Video 6-2)
Background
Surgical Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree