High-Velocity, Low-Amplitude Technique
Jonathan D. Tait
Steven J. Karageanes
OVERVIEW
The thrust technique [also called the high-velocity, low-amplitude (HVLA) technique, or mobilization with impulse] is one of the oldest and most widely used forms of manual medicine. Although there are different types of thrust techniques, including the low-velocity, high-amplitude technique, this chapter focuses on HVLA techniques. HVLA had been the main technique taught in colleges of osteopathic medicine until recent years, where curricula now contain a variety of direct and indirect techniques as well. Several physiotherapists and other practitioners such as Maitland, McKenzie, and Mennell heavily influenced many of the HVLA techniques used and taught by early osteopathic physicians.
Many theories exist regarding the prevalence of the technique in osteopathic colleges. A. T. Still was known to use thrust sparingly in favor of myofascial release and indirect techniques (1). The faculty and students who assisted in teaching may have been largely responsible for the popularity of thrust techniques over other techniques known at the time. Teachers were able to very accurately describe the joint restriction and provide techniques for correcting the dysfunction. These techniques were much more easily learned and practiced than the myofascial and indirect techniques preferred by Still, which required much more skill in assessing the motion patterns in the tissues in order to precisely treat the dysfunction (1).
Thrust is a direct technique, meaning that the joint exhibiting somatic dysfunction is moved through its restrictive barrier of physiologic motion by an extrinsically applied thrusting force. This extrinsic force allows the joint to return to its appropriate physiologic motion, which Mennell refers to as “joint play” (2). He defines joint play as the movement allowed within a synovial joint, which is independent and cannot be introduced by voluntary muscle contraction (2). The movement is small (less than 1/8 inch) with the range dependent on the contour of the joint surfaces. He also postulates that this motion is necessary for normal, pain-free movement of the synovial articulation and, if restricted or absent, voluntary movement will, in turn, become restricted and frequently painful (2,3). In this sense, the goal of treatment is to use a small thrust—not to force the joint “back into place,” but to restore motion loss at the dysfunctional segment by gapping the joint. Joint gapping can be accomplished with or at right angles to the plane of the joint, or with distraction of the joint (3). Key points to remember regarding joint play are that it is a small, precise movement that is elicited passively, it is independent of voluntary muscle action, and it is found in all synovial joints. Effective treatment results in an immediate increase in range of motion, a decrease in muscle hypertonicity, and often a decrease in pain associated with the dysfunctional area.
CONCEPTS AND PRINCIPLES
Somatic Dysfunction
To successfully use the HVLA technique, one must accurately assess the athlete to diagnose an articulation or vertebral segment that is not exhibiting normal range of motion (4). This
requires a focused, detailed vertebral structural examination after obtaining an accurate history of the athlete’s symptoms. Muscles usually contribute to the joint restriction, and will have characteristic palpatory tissue texture changes, feeling boggy, stringy, or ropy in nature. These findings, as well as local tenderness with palpation or movement, and asymmetry of bony structures, also help the clinician localize the segmental problem (5). The somatic dysfunction usually demonstrates some or all of these characteristic tissue changes, and will also exhibit a change in the quantity and quality of joint motion.
requires a focused, detailed vertebral structural examination after obtaining an accurate history of the athlete’s symptoms. Muscles usually contribute to the joint restriction, and will have characteristic palpatory tissue texture changes, feeling boggy, stringy, or ropy in nature. These findings, as well as local tenderness with palpation or movement, and asymmetry of bony structures, also help the clinician localize the segmental problem (5). The somatic dysfunction usually demonstrates some or all of these characteristic tissue changes, and will also exhibit a change in the quantity and quality of joint motion.
Barrier Concepts
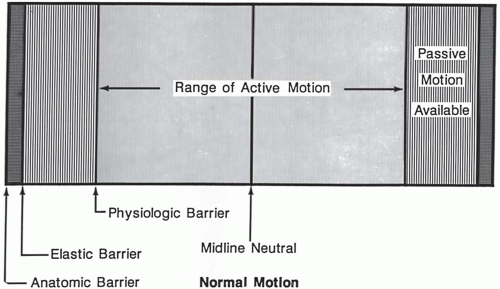
In joint mechanics, a “barrier” generally refers to a motion restriction. It is most commonly produced by either abnormal muscle contraction or capsular-ligamentous shortening, causing a “limit” to the normal range of motion. Within the total range of motion of each joint there exists a range of active motion limited by a physiologic barrier (Fig. 3.1). This physiologic barrier is created by the accumulation of soft tissue tension as the joint moves through its normal range of motion. There also exists a range of passive motion that is limited in each direction by an elastic barrier (Fig. 3.2). The elastic barrier is a physiologic limit of the joint, or the point at which all “slack” or tension has been passively taken out of the joint and surrounding muscle and ligamentous structures. The normal end-feel is due to the resilient nature and tension of these structures. The anatomic barrier of the joint represents the limit to motion beyond which tissue damage occurs. There is a very small potential
space existing between the anatomic and elastic barriers, known as the paraphysiologic space, and it is within this area that the thrust takes place, often generating a “popping” sound (3). The popping sound is not required, however, and may not always signify a successful treatment.
space existing between the anatomic and elastic barriers, known as the paraphysiologic space, and it is within this area that the thrust takes place, often generating a “popping” sound (3). The popping sound is not required, however, and may not always signify a successful treatment.
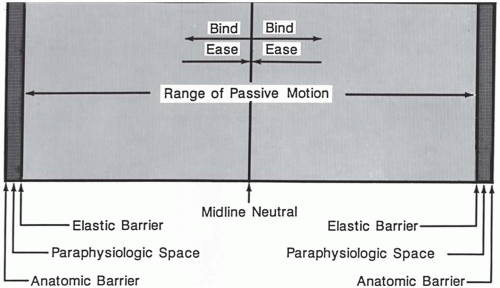 FIGURE 3.2. Passive range of motion with restrictive barriers. (From Greenman PE. Principles of manual medicine, 2nd ed. Baltimore: Williams & Wilkins, 1996, with permission.) |
One can appreciate the differences found within joint motion when a joint exhibits somatic dysfunction. Joint motion will also have a characteristic feel of bind, or a barrier to movement. This barrier, in the direction of motion loss, is known as the “restrictive barrier.” The restrictive barrier and the normal physiologic barrier on the opposite side of the joint limit the amount of active motion remaining within a joint.
Loss of motion is described with these principles in mind, as the asymmetry diagnosed on examination confirms the new position of the dysfunctional segment. The examiner must accurately identify normal and abnormal motion, as well as normal and restrictive barriers to these motions in order to diagnose the somatic dysfunction. Effective treatment will correct the segment, returning its full range of motion. It must be remembered that treatment is not just a change in the static position, but involves the dynamics of motion involving the following general principles (1):
The anatomic barrier is the end point for permitted passive motion; any motion beyond the anatomic barrier damages anatomic structures.
Normal active motion occurs between physiologic barriers.
The restrictive or pathologic barrier is the end point of permitted motion with motion loss in somatic dysfunction.
The normal midline, or neutral point, in the range of motion of a joint is frequently shifted to a new position in the presence of somatic dysfunction.
The dysfunctional segment will exhibit asymmetrical quantity of motion as well as a change in the feel, or quality, of the motion. This aspect is much more difficult for the novice practitioner, but it is a key component in the assessment of motion and positioning for treatment.
Restrictive Barriers
Restrictive barriers cause a limitation in the normal range of motion, and will have palpatory characteristics different from normal anatomic, physiologic, and elastic barriers. Skin, fascia, muscles (long and short), ligaments, and joint capsules and surfaces can all act as barriers (3). Pain can also be a cause of joint restriction. The barriers may involve a single segment or joint (short restrictor), or they may cross more than one joint or series of spinal segments (long restrictor). It is necessary to evaluate the total range of movements, the quality of movement during the range, and the end-feel of the movement to accurately diagnose the restrictive barrier.
Engaging the Barrier
The use of any direct technique requires the practitioner to engage the restrictive barrier. The term “barrier” can be misleading if it is thought of as a rigid obstacle that one is attempting to push through. Rather, as the joint reaches the barrier, restraints in the form of tight muscles and fascia serve to inhibit further motion. Engaging the barrier involves pulling against restraints rather than pushing against some anatomic structure (1). The practitioner monitors the increasing restriction caused by the tissues, positioning the joint at the limit of its motion, effectively engaging this end point, or barrier.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree