Hemivertebra Excision
Daniel J. Hedequist
Michael P. Glotzbecker
DEFINITION
A hemivertebra is a congenital anomaly of the spine that forms during the 8th to 12th weeks of embryologic development. It is characterized by the formation of half of a vertebral body, a corresponding pedicle, and a corresponding hemilamina.
Hemivertebra are classified as a congenital failure of formation.
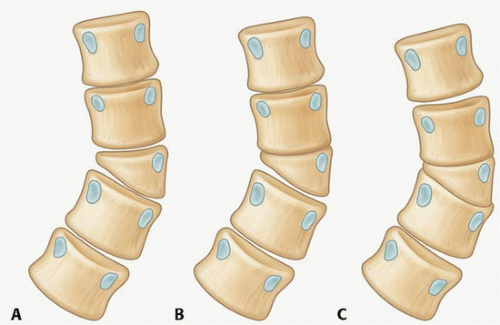
A hemivertebra may be classified as fully segmented (ie, separated from the bodies above and below by discs), partially segmented (ie, separated from one adjacent body by a disc and fused to the other adjacent body), or unsegmented (ie, fused to the body above and below; FIG 1).1
Progressive curvatures of the spine caused by a hemivertebra result from unbalanced growth. Full-segmented hemivertebra have a much higher rate of progression because the presence of an intact disc space above and below signifies the presence of growth plates and potential asymmetric spinal growth.
ANATOMY
The hemivertebra has a partial vertebral body, a pedicle, and a hemilamina.
Anatomically, it may be joined to the level above or below at either the body, the hemilamina, or both. If the hemivertebra is not fused to either adjacent segment, the potential for asymmetric spinal growth is high.
A local kyphotic or lordotic deformity may occur with hemivertebra if the associated failure of formation is greater anteriorly or posteriorly.
PATHOGENESIS
Progressive spinal curvatures due to hemivertebra are a result of disordered growth.
The hemivertebra is a wedge on the convex side of a curve. In the presence of healthy growth plates above and below (ie, a fully segmented hemivertebra), convex growth is faster than contralateral concave growth, causing a progressive scoliosis.
In cases of hemivertebra, if the vertebral body lies in the posterolateral quadrant, a progressive kyphosis may arise in association with the scoliosis.
The disordered growth eventually may cause curvature to such a degree that normally segmented areas of the spine become involved in the curve, causing deformity and spinal imbalance.
NATURAL HISTORY
The natural history of a hemivertebra depends on its location and the potential for growth and curve progression.
Hemivertebrae that are fully segmented progress at approximately 2 degrees a year and can exceed over 45 degrees at maturity.3 These require treatment to prevent deformity and also to prevent adjacent spinal curvature.
Partially segmented hemivertebrae have much less growth potential (<1 degree per year), rarely exceeding 40 degrees at maturity. They usually do not require treatment. Unsegmented hemivertebrae generally require no treatment.
Hemivertebra at the lumbosacral junction almost always require treatment because the lumbar spine takes off obliquely from the sacrum, causing a long compensatory curve in normally segmented regions of the lumbar spine, with resultant cosmetic deformity and spinal imbalance.
PATIENT HISTORY AND PHYSICAL FINDINGS
Embryologic development of the spine occurs between the 8th and 12th weeks of gestation; hence, other organ systems developing at the same time also may have a congenital anomaly.
A complete musculoskeletal examination looking for diagnoses such as clubfoot, developmental dysplasia of the hip, and limb anomalies is warranted.
A complete neurologic examination should be performed because as many as 40% of patients with congenital scoliosis have a corresponding spinal dysraphism. This examination includes sensory, motor, and reflex testing.
Occult signs of spinal dysraphism include cutaneous manifestations such as midline spinal hemangiomas, penetrating sacral dimples, or midline hairy patches. Foot anomalies such as vertical talus or asymmetric cavus feet can signify spinal dysraphism.
Cardiac auscultation should be done because 20% of patients with congenital scoliosis have congenital heart anomalies.
Observe shoulder position, trunk position, and waist symmetry. Truncal imbalance is an indicator of curvature.
Observe the flexibility of the patient’s spine.
Rotation of the spine during the Adams forward bend test is indicative of deformity and points to its location.
IMAGING AND OTHER DIAGNOSTIC STUDIES
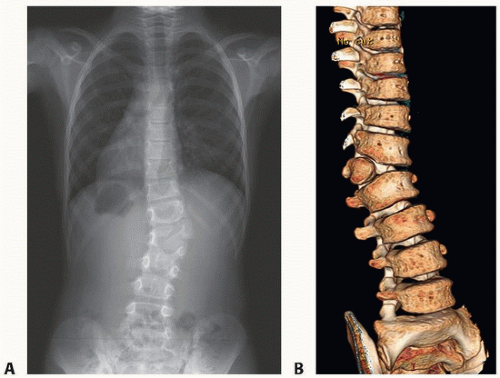
Standing 36-inch posteroanterior (PA) and lateral radiographs are mandatory to define the deformity and assess the Cobb measurement. Apparent progression may be seen from supine radiographs to standing radiographs (FIG 2A).
Bending radiographs, in which the patient is directed to bend in a concave and then in a convex direction, are useful to assess the flexibility of curves above and below the hemivertebra.
Magnetic resonance imaging (MRI) scanning of the brainstem and spinal cord is mandatory before any surgical intervention, given the high association (30% to 40%) of congenital scoliosis with spinal dysraphism.1
Computed tomography (CT) scans with three-dimensional (3-D) reconstructions should be obtained to delineate the anatomy of the anterior and posterior elements as an aid in planning the operation and to avoid intraoperative problems such as unexpected posterior element deficiencies or fusions (FIG 2B).2
A pediatric protocol should be used for CT scans to avoid the significant radiation exposure that results when adult protocols are used for children.
Preoperative evaluation of the genitourinary system with a screening ultrasound and evaluation of the cardiac system with an echocardiogram are necessary if these have not been performed, given the rate of anomalies associated with congenital scoliosis.
DIFFERENTIAL DIAGNOSIS
Failure of vertebral formation
Failure of vertebral segmentation
Sequela of infection causing partial vertebral body destruction
Tumor
NONOPERATIVE MANAGEMENT
Nonoperative management is reserved for nonprogressive curves caused by hemivertebra.
Hemivertebra associated with little or no curve progression (unsegmented or partially segmented) may be followed during growth with radiographs every 6 to 12 months, depending on the degree of deformity and age of the patient.
Bracing has no role in the management of a hemivertebra.
SURGICAL MANAGEMENT
The classic indication for a hemivertebra resection is a patient with a progressive curve secondary to a fully segmented hemivertebra in the thoracolumbar, lumbar, or lumbosacral regions with a resultant deformity.
We have found that excision is best performed between the ages of 18 months and 4 years.
Patients younger than this may be more difficult to instrument, and waiting until this age rarely has caused irrevocable deformity.
Excision in older patients is feasible; we have found, however, that if diagnosed early, there is no reason to wait past the age of 4 years given the progression of curvature and its effect on normally segmented regions of the spine.
Instrumentation at these ages is technically feasible.
Preoperative Planning
Review of the preoperative MRI of the spine
If spinal dysraphism is present, referral to a neurosurgeon is mandatory.
If the patient requires neurosurgical intervention for dysraphism, that procedure should precede the hemivertebra excision, either at the same setting or in a staged setting, at the discretion of the spine surgeon and neurosurgeon.
Review of the 3-D CT scans
A complete understanding of the anatomy of the hemivertebra is crucial to avoid intraoperative confusion, especially because associated posterior element fusions or absences can make identifying levels difficult.
Studying the pedicle anatomy (ie, length and diameter) of the levels above and below is efficacious given the smaller size of these patients.
Neurologic monitoring is important and should be done using somatosensory evoked potentials and motor evoked potentials.
Communication between the monitoring and anesthesia teams should be facilitated to prevent any change in neurologic function brought on by anesthetics, hypotension, or low blood volume.
Positioning
We perform hemivertebra excisions with the patient in the prone position.
This is done on a radiolucent operating frame with chest and pelvic support, which leaves the abdomen free.
We also have found it useful to slightly “airplane” the table or bolster the patient so that the convex side is slightly higher than the concave side. This helps with visualization anteriorly, control of bleeding, and retraction of the dura and its contents (FIG 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree