Hemi-Hamate Autograft Reconstruction of Unstable Dorsal Proximal Interphalangeal Joint Fracture-Dislocations
Thomas R. Kiefhaber
Rafael M. M. Williams
Meredith N. Osterman
DEFINITION
Proximal interphalangeal (PIP) joint fracture-dislocations occur with the following fracture patterns11:
Palmar lip fracture-dislocations: fracture of the middle phalanx palmar lip with dorsal subluxation of the middle phalanx on the head of the proximal phalanx
Dorsal lip fracture-dislocations: fracture of the dorsal lip of the middle phalanx with palmar subluxation of the middle phalanx
Pilon fractures: Pilon fractures include a loss of continuity of both the dorsal and palmar cortical margins of the middle phalangeal articular surface. The base of the middle phalanx usually is highly comminuted, and the articular fragments may be significantly impacted.
PIP fractures are further classified as “stable” or “unstable.”
Stable fractures maintain concentric joint reduction throughout the range of motion (ROM).
Unstable fractures sublux or dislocate during parts of the motion arc.
Dorsal lip fracture treatment is complicated by the need to reestablish continuity of the extensor tendon insertion onto the middle phalanx.
Pilon fractures are best treated with some form of traction and early motion.
Unstable palmar lip fractures are amenable to treatment with hemi-hamate autograft and are the focus of this chapter.
ANATOMY
The PIP joint is a complex hinge articulation that provides more than 95 degrees of flexion while maintaining stable, concentric reduction of the joint surfaces.
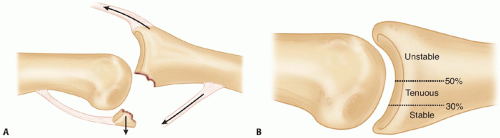
Several forces encourage dorsal migration of the middle phalanx: The extensor tendon lifts the middle phalanx and the mid-middle phalanx superficialis insertion levers the middle phalanx dorsally7 (FIG 1A).
The only restraints on middle phalangeal dorsal translation are the palmar plate and the cup-shaped geometry of the middle phalanx articular surface. The middle phalangeal palmar lip wraps around the proximal phalanx head and acts as a hook, preventing dorsal translation.
Palmar lip fractures disrupt both of the restraints to dorsal subluxation. The palmar plate is no longer attached, and the middle phalangeal palmar lip is disrupted. The slope of the remaining middle phalangeal articular surface encourages the middle phalanx to travel up and over the proximal phalangeal head.
A direct relation exists between the amount of palmar articular surface disrupted and stability (FIG 1B).
Hastings and Hamlet8 has shown that when 42% of the palmar articular surface is damaged, the joint always exhibits dorsal instability.
In the clinical setting, fractures with as little as 30% articular surface involvement can be unstable.
Hemi-hamate arthroplasty restores stability by rebuilding the cup-shaped geometry of the middle phalangeal base and restoring the palmar plate attachment.
PATHOGENESIS
The middle phalangeal palmar lip fracture that is associated with unstable dorsal PIP fracture-dislocations is created by either avulsion of the fracture fragment or an impaction shear mechanism.
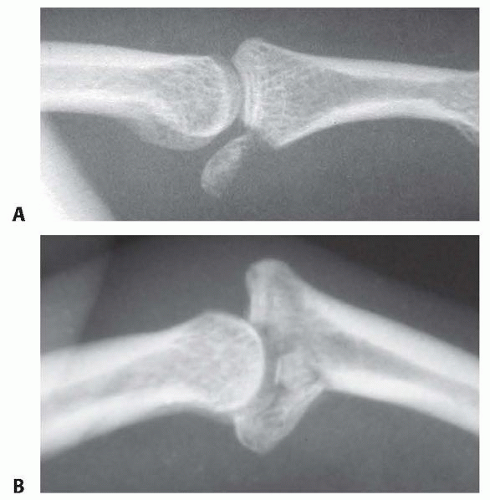
Avulsion fractures result from PIP joint hyperextension and traction through the palmar plate attachment (FIG 2A).
The fracture fragment is not comminuted and represents less than 30% of the articular surface.
These injuries usually are stable and rarely require surgical intervention. If the joint is unstable, osteosynthesis with lag screws often is possible because of the lack of comminution and the substantial size of the fragment.
Impaction shear PIP fracture-dislocations result from a longitudinally applied load to the tip of the finger with the PIP joint slightly flexed, such as in a mishandled ball catch. The force drives the middle phalanx into and over the proximal phalanx head, resulting in a middle phalangeal palmar lip fracture that is highly comminuted (FIG 2B).
Up to 80% of the joint surface can be involved, and the articular fragments are often deeply impacted into the soft metaphyseal bone.
Disruption of the terminal extensor tendon (mallet finger) often occurs in association with unstable dorsal PIP fracture-dislocations.
NATURAL HISTORY
The long-term prognosis for PIP fracture-dislocations is theoretically affected by the quality of the joint surface restoration and the maintenance of concentric reduction of the middle phalanx on the proximal phalangeal head.
The PIP joint seems to tolerate less than perfect restoration of a smooth joint surface. As long as motion is initiated quickly, small gaps and step-offs seem to be tolerated. Long term, some remodeling occurs, and most patients do not need to be treated for symptomatic posttraumatic degenerative arthritis.
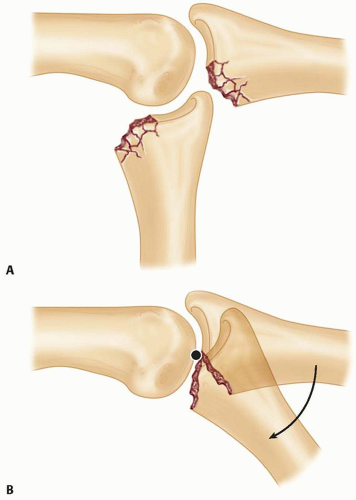
Joint reduction that is less than perfect is not well tolerated. When the middle phalanx rides dorsally on the proximal phalangeal head, PIP flexion occurs by “hinging” at the fracture margin.11 The joint pivots on the palmar edge of the fracture, and the proximal phalanx falls into the fracture defect at the palmar base of the middle phalanx. The proximal phalangeal articular cartilage suffers accelerated wear, whereas the remaining undamaged middle phalangeal articular surface remains unused throughout the motion arc (FIG 3).
Treatment of unstable PIP palmar lip fractures is directed toward reestablishing joint stability so that flexion occurs by “gliding” of the remaining middle phalangeal articular cartilage on the head of the proximal phalanx.
PATIENT HISTORY AND PHYSICAL FINDINGS
Assess alignment in the coronal plane. Lateral deviation suggests asymmetric compression of articular fragments.
Assess alignment in the sagittal plane. Lack of colinearity of the middle and proximal phalanx suggests persistent joint subluxation or dislocation.
Associated mallet injuries must be treated concurrently with a distal interphalangeal (DIP) joint extension splint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs in the posteroanterior (PA) and lateral planes provide the mainstay of radiographic evaluation of PIP fracture-dislocations.
Inspect the lateral radiograph to determine the percentage of joint surface fractured and the quality of the reduction.
If the joint is not concentrically reduced with less than 30 degrees of flexion, the joint is classified as unstable and must be treated appropriately (see FIG 1B).
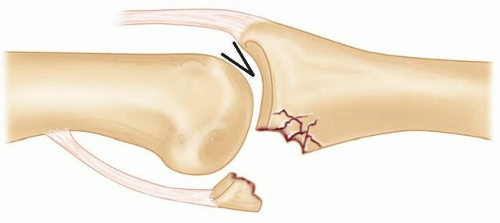
On every lateral radiograph taken throughout the treatment course, carefully scrutinize the quality of the reduction. The remaining articular cartilage on the middle phalanx base must be in full contact with the proximal phalanx head. Any dorsal gap between the two surfaces—a “V” sign—indicates persistent instability and must be corrected (FIG 4).
The percentage of the middle phalanx articular surface consumed by the fracture can be used to predict joint reduction stability7,8,11 (see FIG 1B):
Less than 30%: The reduction usually is stable. The middle phalanx almost always remains concentrically reduced on the head of the proximal phalanx throughout a full ROM.
Thirty percent to 50%: The reduction is tenuous. The middle phalanx may or may not subluxate dorsally when the PIP joint is extended. If any subluxation is noted on the lateral radiograph with the PIP joint fully extended, flex the joint to 30 degrees and repeat the lateral radiograph.
If concentric reduction is achieved and the palmar fragments are sitting where they will reconstitute a palmar lip, some form of extension block treatment may be employed.
If the joint will not stay reduced with less than 30 degrees of flexion, the joint is unstable and must be treated accordingly.
Over 50%: The PIP joint is unstable, and surgical intervention usually is required to rebuild the cup-shaped geometry of the middle phalanx base and to reattach the palmar plate.
Inspect the PA view to determine asymmetric compression of middle phalanx articular fragments leading to varus or valgus angulation.
Computed tomography (CT) or magnetic resonance imaging (MRI) evaluation rarely is necessary.
DIFFERENTIAL DIAGNOSIS
In patients with a history of recent trauma and radiographic confirmation of a large PIP palmar lip fracture associated with dorsal subluxation, the diagnosis of an unstable PIP dorsal fracture-dislocation is obvious.
Dorsal dislocation and disruption of the middle phalanx palmar lip also may be seen in chronic PIP fracture-dislocations and occasionally in association with various forms of arthritis.
NONOPERATIVE MANAGEMENT
Unstable PIP fracture-dislocations rarely can be managed nonoperatively. When over 50% of the middle phalanx articular surface is consumed by fracture, all restraints to dorsal subluxation are lost. The cup-shaped geometry of the middle phalanx base must be restored and the palmar plate reattached. Both goals can be accomplished with osteosynthesis of a single large fragment,4,5,10 palmar plate arthroplasty,3 or a hemi-hamate osteochondral autograft.6,17,18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree