Chapter 35 Ischaemic heart disease
Myocardial infarction
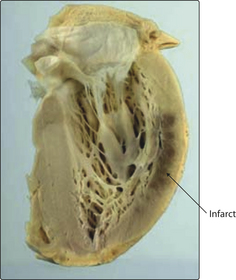
Coronary arteries are end-arteries. The ventricular wall is supplied by perforating branches arising from the epicardial coronary arteries. The subendocardial zone is furthest from the blood supply and it is here that critical ischaemia tends to occur first. As the infarct enlarges, it extends further towards the epicardial surface (Figs 3.35.1 and 3.35.2). The exception is a very narrow band of myocardium immediately adjacent to the endocardium that receives enough oxygen to survive from the blood within the ventricle. The area of infarcted muscle depends on the territory supplied by the obstructed artery. No two hearts are exactly the same, but typical regional infarcts tend to occur in the territories shown in Fig. 3.35.3.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree