(15% to 30% involvement of the femoral head), and severe (greater than 30% involvement of the femoral head). Though there is no consensus, treatment options and algorithms are largely based on whether the femoral head is in a precollapse or postcollapse stage at the time of presentation. Other factors to consider when deciding whether to perform a head-preserving procedure versus an arthroplasty include patient age and activity level, acetabular involvement, lesion size and location (14), and associated patient risk factors (15). In those with precollapse and early postcollapse lesions, treatment strategies are aimed at preserving a congruent femoral head and delaying and/or avoiding collapse and subsequent arthroplasty. Femoral head-preserving procedures include core decompression, nonvascularized bone grafting, and vascularized bone grafting. On rare occasions, proximal femoral osteotomies may be considered to rotate an uninvolved portion of the femoral head into the weight-bearing portion of the articular surface. This technique will be described in Chapter 9, Periacetabular Osteotomy and Proximal Femoral Osteotomy.
TABLE 8-1 Direct and Indirect Risk Factors for Osteonecrosis of the Hip | |
|---|---|
|
TABLE 8-2 Commonly Used Staging Systems for Osteonecrosis of the Hip | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
compared to medial-based lesions and those involving less than 30% of the femoral head. Thus, the low likelihood of success within this subset of large-sized lesion patients may be considered by some to be a contraindication to performing a femoral head-preserving procedure. The quality of the articular cartilage on the acetabulum must also be considered when attempting head-preserving procedures as those with substantial degenerative changes on the acetabular side may be best treated with a total hip arthroplasty. If marked involvement of the weight-bearing portion of the femoral head is involved, many authors may opt for a total hip arthroplasty. Similarly, femoral head depression of greater than 2 mm has been considered an indication for arthroplasty surgery.
Precollapse lesions (Ficat and Arlet stages I and II)
Small- to medium-sized lesions (30% head involvement or less or Kerboul angle less than 200 degrees)
Postcollapse lesions in patients who are unable to tolerate a more extensive femoral head-preserving procedure
Postcollapse lesions (Ficat and Arlet stages III and IV)
Femoral head depression greater than 2 mm
Large-sized lesions involving greater than 30% femoral head
Acetabular involvement
Patients who are unable to comply with postoperative weight-bearing restrictions
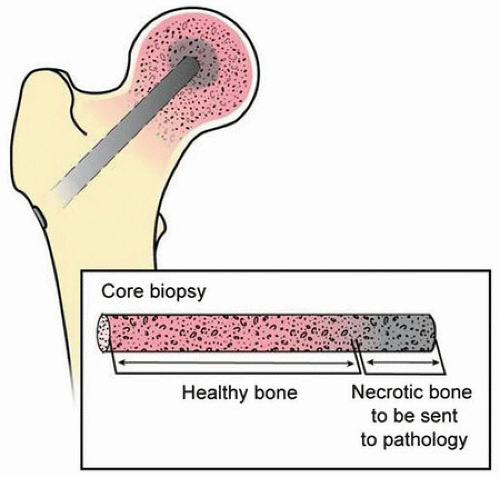
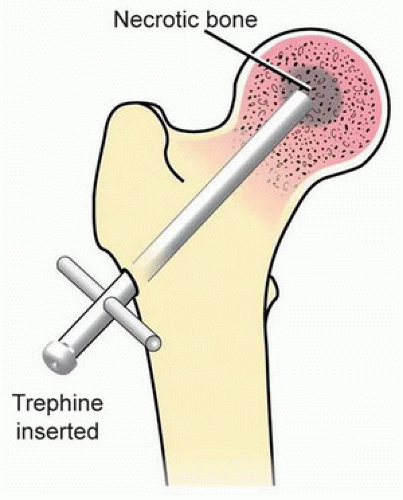 FIGURE 8-1 Illustration of 8- to 10-mm trephine inserted into the necrotic osteonecrosis lesion of the femoral head. |
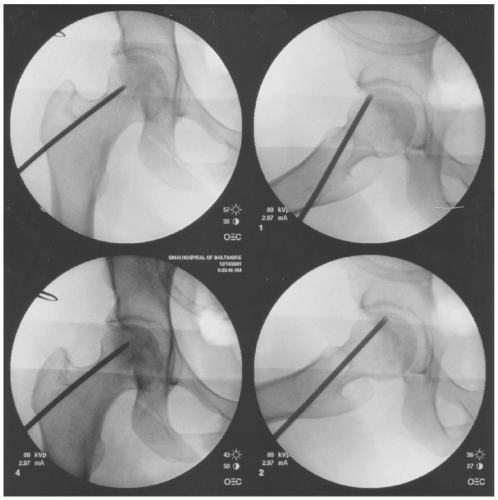
gauze around the skin-pin junction during all drilling maneuvers. The position and trajectory of the pin is now assessed in the AP and frog-leg lateral planes by removing the drill from the pin and having an assistant maneuver the leg into the appropriate position. If the trajectory is acceptable, the leg is brought back into the starting position and the pin advanced through the femoral neck towards the lesion. If unacceptable, the pin is backed out and redirected ensuring that the same starting hole is used to avoid creating another stress riser. The pin is then advanced to the appropriate depth in the subchondral bone taking care not to penetrate through the articular surface into the joint. While drilling through the lesion, it is common for areas of sclerosis to be encountered. The surgeon must avoid the urge to use larger amounts of force when attempting to drill through these lesions as the risk of plunging through the femoral head into the hip joint is increased. Larger-sized lesions may be treated with 2 to 3 passes of the Steinman pin using the same technique and starting hole (Fig. 8-3). Once adequate decompression is obtained, the pin is backed out while holding a saline-soaked 4 × 4 gauze around the pin-skin junction. Direct pressure is held at the skin entry site until adequate
hemostasis is achieved. A simple suture using absorbable monofilament may be required although a Band-Aid is usually sufficient.
Care must be taken to create a starting point above the level of the lesser trochanter in order to avoid creating a stress riser and potential for future subtrochanteric femur fracture.
There is a risk of skin-edge necrosis when drilling the Steinman pin in a percutaneous fashion. This risk can be minimized by keeping a saline-soaked 4 × 4 gauze sponge at the skin-pin junction during all drilling maneuvers.
When adjusting the trajectory of the pin, the same entry hole should be used as creation of a new pilot hole adjacent to the original hole can create a new stress riser.
Exercise caution when drilling through osteonecrotic lesions as areas of hard bone are commonly encountered. The surgeon must resist the urge to push harder and risk plunging through the femoral head into the hip joint.
Subtrochanteric stress riser leading to proximal femur fracture from multiple entry holes or entry point made at or below the level of the lesser trochanter.
Pin penetration of femoral head into hip joint with overzealous drilling.
Skin-edge thermal necrosis.
Iatrogenic weakening of the femoral head and neck may be created if using large-diameter tre-phines/cannulas or by the creation of multiple pin tracts.
TABLE 8-3 Outcomes of Traditional Core Decompression | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||