Head Injuries
Margot Putukian
Head injuries occur commonly during sports participation, and can have serious consequences if not treated properly. Detecting injury, assessing severity, and making appropriate return to play (RTP) decisions are important responsibilities of the physician caring for athletes of all ages. An organized comprehensive evaluation, with special attention to exclude cervical spine injury, vascular or other focal injuries are essential for the physician caring for athletes on the sideline. Understanding the complications and long-term sequelae of head injuries and how these impact RTP decisions is important. This chapter will discuss these issues and review current literature regarding head injuries in athletes.
In general, the head injuries that occur in the athletic setting are mild in comparison to those that occur in motor vehicle accidents or other high velocity impact injuries. Despite this, the physician taking care of the athlete must always consider the possibility of a catastrophic injury. Of the catastrophic injuries that occur on the athletic field, head and spine injuries, along with cardiac fatalities, are the most common. Recognizing serious head and spine injuries and understanding their progression is therefore essential. For the head injured athlete, the most common serious injuries include vascular intracranial injuries and cervical spine injuries. Vascular catastrophes can present immediately or be delayed by several hours. Other complications of brain injury include “second impact syndrome” (SIS) (1,2), repetitive and/or cumulative injury, and postconcussion syndrome. The morbidity and mortality of these complications are significant for the athlete. Cervical spine injuries often occur in association with head injuries, and can be missed because of the attention paid to the brain injury. A comprehensive method of evaluating and following up the injuries of these athletes remains paramount in order to minimize the potential for missing these other related injuries. Whether there are age- or gender-related risks for head injury is a question that remains unanswered. What are the risks present with RTP before complete cognitive recovery or with recurrent head injury and are there prognostic factors that help determine which athletes are at greater risk for long-term complications of injury? These are issues that have begun to be addressed.
The assessment of head injury includes recognizing that an injury has occurred, managing the acute injury, determining referral status, and eventually making RTP decisions. Many head injuries go undetected, and are not reported to the medical or coaching staff. This may be in part due to the lack of availability of medical staff for certain sports or levels of participation, but in many cases it is due to the nature of the sport, where sustaining a “ding” or “bell-ringer” is felt to be part of the game. Some athletes will try to minimize their injury, knowing that if they report their symptoms, they will be kept out of play. This can obviously have significant consequences. Athletes and coaches must be educated on the importance of these injuries in terms of the athlete’s long-term health and function (3). In one study of rugby athletes, 56% of 544 athletes sustained at least one head injury associated with memory loss (amnesia) after the event. In those athletes who had amnesia lasting more than 1 hour, only 38 of 58 athletes were admitted to the hospital for treatment (4). Fortunately, over the last several years, the impact of these injuries has become more apparent, and an increased awareness by both the athletic training staff and medical personnel has allowed for a higher index of suspicion and earlier detection of these injuries.
Post-traumatic encephalopathy, or the “punch drunk syndrome”(5), has been described in boxers and is felt to be due to repetitive injuries that result in cumulative injury to the brain. This repetitive, cumulative head trauma may increase the risk for the development of Alzheimer’s disease (5,6,7). The long-term risks of repetitive head trauma is an area of sports medicine research that is gaining significant attention, and with the advent of neuropsychological and balance testing, more sensitive tools for assessing cognitive function after mild traumatic brain injury (MTBI) are available.
Epidemiology
According to the National Head Injury Foundation, sports causes 18% of all head injuries, compared to motor vehicle accidents (46%), falls (23%), and assaults (10%). In 1984, traumatic brain injuries accounted for approximately 500,000 hospital admissions, with 3% to 10% of these related to sport activities (8). One million head injuries are seen in North American emergency departments annually. Head injury causes 19% of all nonfatal injuries in football, and 4.5% of all high school sports injuries (9,10). At the elementary, junior, and high school levels, football accounts for the highest incidence of head injury among any sport (11).
Amongst young children in Australia, closed head injury was six times more likely to be a result of organized sports activities versus leisure activities (12). In the United States it is estimated that 1 million children sustain head injuries annually, 85% of them being mild, with 250,000 admissions, accounting for 10% of all emergency room visits (13).
As mentioned previously, the incidence of concussion is likely greater than what is reported, especially in younger athletes for whom medical care is less available. A recent retrospective study of 1,532 high school football players from 20 schools found that 29.9% of players reported a history of concussion, with 15.3% reporting a concussion in the current season. Of these recent injuries, only 47.3% were reported, predominantly to a certified athletic trainer. Of the unreported injuries, 66.4% of the respondents felt that their injuries were medically insignificant, 41% did not report their injuries because they did not want to be kept out of play, and the remainder did not realize their injury was a concussion (14). Concussions account for roughly 1.6% to 6.4% of all injuries at the college level, with an incidence of 0.06 to 0.55 injuries/1,000 athlete exposures (15). Over the recent years, ice hockey and football tend to account for the highest percentage of head injuries. However, men’s and women’s soccer also have relatively high incidence rates of concussion. In addition, sports that utilize head protection (ice hockey, football, men’s lacrosse) have a similar incidence to those sports without head protection (men’s and women’s soccer, field hockey). Player to player contact is the most common mechanism of injury reported in most sports tracked by the National Collegiate Athletic Association (NCAA), with the exceptions being field hockey (contact with the stick), women’s lacrosse, women’s softball, and baseball (contact with the ball). Understanding the mechanism of injury is very important in the attempts to decrease injuries by considering changes to rules or equipment.
Helmets
In several sports, wearing of helmets has been proposed as a means to decrease head injury. It is important to use injury surveillance data to make decisions with evidence-based data to support these changes. Although appealing at first glance, one must be aware of the potential that wearing a protective equipment may have. In other words, by wearing a helmet, some athletes may feel invulnerable, play more aggressively, and this may potentially change the nature of the sport. Wearing a weighted, hard plastic helmet may inadvertently increase the risk of either head injury or cervical spine injury. Therefore, it is important that one considers the true incidence of injury as well as the potential, even untoward, effects that the proposed changes may have on sports.
The use of helmets has decreased the frequency of head injury in ice hockey and football (16,17). The 50% decrease in injuries in football since 1976 (18) has been attributed to both changes in helmet fit and design, as well as rule changes that forbid spear tackling. The data has been more controversial for ice hockey because, although there has been a decrease in head injury, there has been an increase in cervical spine injuries. The use of helmets with face guards has significantly reduced the number of orofacial injuries. Pforringer (19) found that 75% of 246 injuries in ice hockey were a result of violence outside game play (high sticking, deliberate pushing, fist fighting). Therefore, enforcement of existing rules may be as important in protecting athletes from head injury as proper equipment.
In baseball and softball, helmets are used effectively to decrease the incidence of head injury. Athletes in these sports use helmets while batting and running bases. Ample evidence exists to demonstrate that head injury, involving a batted or thrown ball, has decreased (15,20). Possibly the most compelling evidence for the use of helmets in decreasing head injury is bicycling. When a fall occurs while bicycling, there is a 50% chance that a head injury will occur, and if the cyclist is traveling 20 mi/hour, there is a higher risk of fatality (20). Every year, 1,300 deaths occur as a result of cycling accidents, with most occurring due to head injury. When an appropriate helmet is used, the risk of traumatic brain injury is decreased by 88% (21). Given this data, the use of helmets by the cycling athlete is imperative.
Definitions
Head injuries occur on a spectrum, with or without focal abnormalities. Focal injuries include subdural hematoma, epidural hematoma, cerebral contusion, and intracranial hemorrhages, both subarachnoid and intracerebral. Diffuse brain injuries do not have focal lesions associated with them, but can be associated with significant deficits in cognitive function. Focal injuries often occur as a result of blunt trauma and are associated with focal neurological deficits and loss of consciousness (LOC). If LOC is brief or does not occur, these injuries can go undetected, making it more important that injury assessment is complete and thorough. Early recognition and treatment of these focal injuries is essential in optimizing successful recovery.
Subdural Hematoma
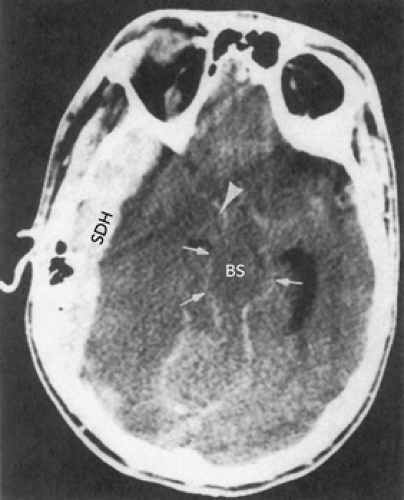
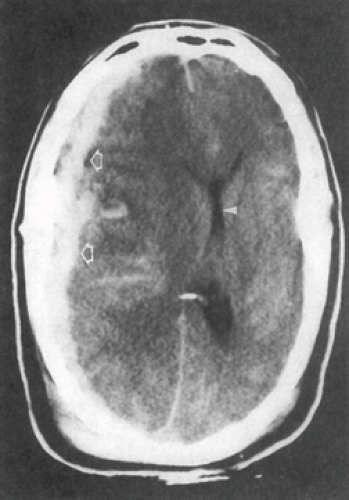
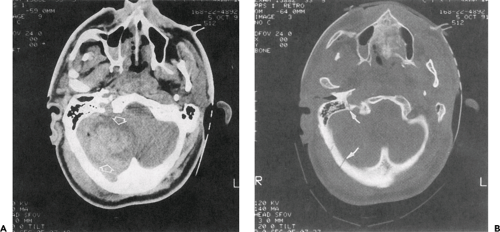
Subdural hematomas occur as a result of disruption of the venous blood vessels, causing a low-pressure accumulation of blood in an enclosed space. These “subdurals” are the most common focal injuries in the sport setting, and are often associated with LOC and slow deterioration of mental status and focal neurological deficits. If there is no associated underlying cerebral contusion or edema, the subdural is considered simple, yet the mortality rate approximates 20%. If there is underlying cerebral contusion or edema, then it is considered a complex subdural, and the mortality rate increases to 50% (see Figures 14.1 and 14.2). Depending on the age of the athlete, subdural hematomas may be more or less symptomatic. Cerebral atrophy correlates with age, and therefore there is more room for accumulation of blood in the older athlete. For a younger athlete, the same amount of bleeding will result in more and earlier onset of symptoms. Early recognition is therefore more important in the younger athlete in whom deterioration can occur quickly and become life threatening. In the older athlete the symptoms are due to a mass effect, whereas in the younger athlete the symptoms are often a result of compression of the normal brain substance (22).
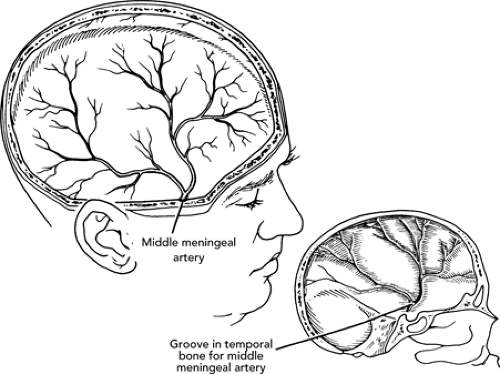
Epidural Hematoma
Epidural hematomas are not as common as subdural hematomas, and are high-pressure vascular injuries. They are due to disruption of a meningeal artery, most often the middle meningeal artery. The classic presentation of an epidural hematoma is an initial LOC followed by a lucid interval and apparent recovery. Then, after minutes to hours, headache, rapid deterioration of mental status, LOC with pupillary abnormalities (ipsilateral pupil dilates), and decerebrate posturing with weakness on the opposite side of the bleed will occur (23). Only one third of the patients will demonstrate this “classic” presentation (see Figure 14.3), underscoring the need to maintain a high index of suspicion for these emergencies.
Other Focal Injuries
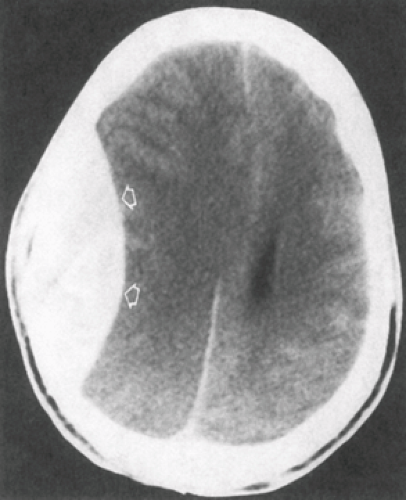
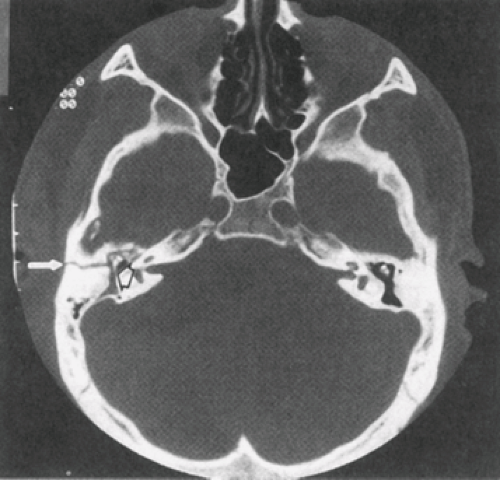
Other focal injuries include cerebral contusions, intracerebral hemorrhages, and subarachnoid hemorrhages. Common symptoms of these injuries include headache, post-traumatic amnesia (PTA), and confusion, but not LOC. Intracerebral hemorrhages occur within the substance of the brain, whereas subarachnoid hemorrhages occur on the surface of the brain. Cerebral contusions and hemorrhages can both occur in association with mass changes and hydrocephalus (see Figures 14.4 and 14.5).
Computed tomography (CT) as well as magnetic resonance imaging (MRI) and electroencephalography (EEG) are useful tools for detecting focal injuries (22,24,25,26,27,28). MRI is a sensitive tool, and MRI findings in those individuals with persistent LOC admitted to the
intensive care unit correlate with the depth and severity of injury. Lesions were present in 88% of these patients with severe clinical compromise (29). The diagnostic test of choice in the first 48 hours for evaluation of the head injured athlete is CT, given the sensitivity of this test to detect blood and fracture better than MRI. After 48 hours, MRI is favored for detecting subtle injuries (30,31,32). Both CT and MRI are equally sensitive in detecting focal injuries requiring surgical treatment (33). For those lesions requiring neurosurgical treatment, the time from detection to treatment is critical in terms of reducing morbidity and mortality.
intensive care unit correlate with the depth and severity of injury. Lesions were present in 88% of these patients with severe clinical compromise (29). The diagnostic test of choice in the first 48 hours for evaluation of the head injured athlete is CT, given the sensitivity of this test to detect blood and fracture better than MRI. After 48 hours, MRI is favored for detecting subtle injuries (30,31,32). Both CT and MRI are equally sensitive in detecting focal injuries requiring surgical treatment (33). For those lesions requiring neurosurgical treatment, the time from detection to treatment is critical in terms of reducing morbidity and mortality.
Diffuse Axonal Injury
Diffuse brain injuries are nonfocal injuries with no identifiable lesion. The spectrum of these injuries correlates with the amount of anatomical disruption. Diffuse axonal injury represents the most severe injury along the spectrum and is often associated with prolonged LOC. It is commonly associated with residual psychological personality and neurological deficits. Cerebral concussion is often considered at the other end of the spectrum and represents a nonfocal injury, although it can be associated with structural abnormalities.
Cerebral Concussion
Cerebral concussion has been defined as “a clinical syndrome characterized by immediate and transient impairment of neurological function secondary to mechanical forces” (34). The hallmarks of concussion are confusion and amnesia. LOC does not necessarily occur during concussion, and varying amounts of memory dysfunction can occur. Headache is the most common symptom of concussion, and this symptom can occur by itself without concussion, making it difficult to discern and evaluate athletes with more severe injury from those with only mild trauma and headache. Additional symptoms that are typical in cerebral concussion are given in Table 14.1. Typically, concussions involve the rapid onset of short-lived neurological impairment that resolves spontaneously. Though neuropathological changes may occur, the acute symptoms seen are generally due to a functional disturbance, not
structural injury. Resolution of injury generally occurs in a sequential course, and neuroimaging studies are generally grossly normal. Cerebral concussion, commonly referred to as MTBI, is the most common head injury seen in athletic practice or competition. MTBI can occur independently or in association with the focal injuries described earlier. MTBI can be associated with significant morbidity and mortality, especially if not treated appropriately.
structural injury. Resolution of injury generally occurs in a sequential course, and neuroimaging studies are generally grossly normal. Cerebral concussion, commonly referred to as MTBI, is the most common head injury seen in athletic practice or competition. MTBI can occur independently or in association with the focal injuries described earlier. MTBI can be associated with significant morbidity and mortality, especially if not treated appropriately.
Mechanisms and Pathophysiology
Understanding injury mechanisms can be useful in predicting the severity and recovery from head injury (35,36), as well as potentially avoiding injuries from occurring. Diffuse brain injuries are associated with anatomical changes, including disruption of axonal and myelin sheath structures throughout the white matter of the hemispheres and brain stem, petechial hemorrhages in periventricular regions, and chromatolysis and cell loss throughout the cortical gray matter and brain stem nuclei (37,38,39,40). With repetitive injury, atrophy of the cerebral hemispheres can occur (39). Research models of head injury demonstrate acceleration and impact forces similar to that seen in sports, and both of these are important in the pathophysiology of injury.
Recent reviews have discussed the correlation of specific traumatic forces with different types and severities of head injuries (41). Rotational forces and their subsequent shearing stresses are felt to be the most important factors in causing severe structural injuries (37,39,42,43). An example of a rotational force in sports is the boxer being struck by a left hook. Acceleration forces can occur when an athlete’s moving head strikes a nonmoving object, such as the ground. Impact or compressive forces occur when a stationary head is struck with a forceful blow, such as when a football player is struck in the head. These forces often occur in various combinations, with the combination of both acceleration and rotational forces associated with the most significant deleterious effects (43).
Injuries are considered “coup” injuries when the area maximally injured is the area just beneath where the head was struck, which is often the case in impact injuries. “Contra-coup” injuries occur when the maximal area of injury is on the opposite side of the skull where the impact occurred, as is often the case with acceleration injuries. These are easy to understand if one considers that the brain is floating in a fluid within the rigid confines of the skull. When an acceleration or rotational injury occurs, the brain lags slightly behind the skull at impact, and then strikes the opposite side of the skull. The attachments of the dura mater to the bony ridges of the skull create potential forces where this tethering occurs, such that when the skull is impacted, these attachments are pulled on (44).
The strength of the neck musculature is important in providing stability to the head when struck. When a force strikes the skull, the force imparted depends in part on whether the musculature is rigid. Using Newton’s second law (mass × acceleration = force), if the neck musculature is rigid, then more acceleration is necessary to impart the same force to the skull. This explains why a football player prepared for a hit is less likely to sustain an injury, and why a soccer player who forcibly strikes a ball may not be at the same risk as the player who is struck while not expecting
a blow. Therefore, neck muscle strengthening and teaching athletes the proper techniques in certain sport-specific skills may be useful in decreasing injuries.
a blow. Therefore, neck muscle strengthening and teaching athletes the proper techniques in certain sport-specific skills may be useful in decreasing injuries.
TABLE 14.1 Signs and Symptoms of Cerebral Concussion | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mild traumatic injury is associated with neurochemical and neurometabolic changes, which can put cells at risk for insult. In animal research models, the release of excitatory amino acids, such as glutamate, can cause ionic fluxes that disrupt the way cell’s utilize oxygen (45,46,47,48). When a head injury occurs, there is an increased need for glycolysis (45,46,49). At the same time, there is a decrease in cerebral blood flow (46,50), resulting in an imbalance between glucose supply and demand. It has been theorized that this imbalance creates cell dysfunction, which then puts the cell at an increased risk for a second insult (41,51).
In the limited human research that has been performed, the data appears consistent with what is seen in animal research. Cerebral glucose metabolism is increased as a result of ionic shifts (38,52), and reductions in cerebral blood flow and oxidative metabolism occur is association with changes in glutamate, potassium, and calcium. [18F]Fluorodeoxyglucose-positron emission tomography (FDG-PET) scanning studies have shown that these changes occur in severely brain injured patients (53,54). The basic and clinical science of concussion has been reviewed and is discussed in detail elsewhere (55,56).
Evaluation of the Head Injured Athlete
It is essential that the initial evaluation and management of the head injured athlete be thorough, orderly, and performed by appropriate medical personnel in an appropriate setting. The first step in evaluation is recognition that an injury has occurred. On-field evaluation must first assess the need for basic emergency services such as airway, breathing, and circulation (ABC) and assure that a cervical spine injury has not occurred. Observing the mechanism of injury can help the medical staff determine the severity of injury. Observing and recording any LOC that occurs is helpful, as well as noting the time the injury occurred. For the conscious athlete, evaluation should include assessment for any symptoms of concussion, and most importantly, any retrograde or PTA that is present. In the unconscious athlete, the medical personnel should assume that a cervical spine injury is present, and emergency care procedures should be initiated. The Glascow Coma Scale (GCS) is a useful tool in predicting long-term prognosis, although in most sport-related head injuries, the GCS is often normal (see Table 14.2). Eighty percent of patients with a GCS less than 5 will die or remain in a vegetative state, whereas if the GCS is greater than 11, more than 90% will have complete recovery (44). An increase in GCS is associated with improved prognosis, underscoring the importance for serial assessments.
Cervical spine injuries occur in 5% to 10% of severe head injuries (57). The Inter-Association Task Force for Appropriate Care of the Spine-Injured Athlete published a manuscript that reviews the prehospital care of the injured athlete with cervical spine injuries. This manuscript also reviews the importance of the Emergency Action Plan (58). These guidelines, along with those from the American College of Sports Medicine, recommend that for the football player with a helmet, the helmet should be left in place unless an airway must be secured or the facemask cannot be cut away (59).
During the initial assessment, in addition to confirming that the cervical spine is stable, it is also important to exclude associated skull fracture. Findings seen in association with skull fracture are given in Table 14.3. If skull fracture is suspected, there may be an increased risk for intracranial infection, due to the compromise of the skin and skull into the surface of the brain. There is also a 20-fold increase in the risk of intracranial bleed when skull fracture occurs in association with head injury compared
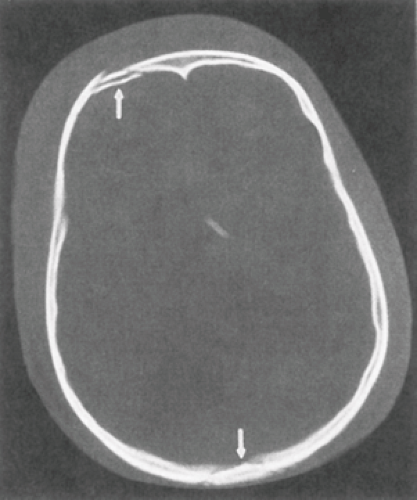
with head injury without skull fracture (60). If any concern for potential skull fracture is present, the athlete should be transported emergently to a medical facility where imaging studies can be obtained (see Figures 14.6 and 14.7) and a neurosurgical consultation can be secured if indicated.
with head injury without skull fracture (60). If any concern for potential skull fracture is present, the athlete should be transported emergently to a medical facility where imaging studies can be obtained (see Figures 14.6 and 14.7) and a neurosurgical consultation can be secured if indicated.
TABLE 14.2 Glasgow Coma Scale | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
On the field, the athlete should be asked questions that assess their orientation, memory status, and overall cognitive function. Once the athlete’s cervical spine is deemed to be stable, further assessment can occur on the sideline. Additional questions, such as what the score of the game is, what color jersey the opponent is wearing, the site of the game, and previous game results, as well as questions on events that occurred before the injury are helpful. Asking about specific plays or defensive/offensive strategies with confirmation by a teammate or coach is also a useful way to determine if the athlete’s memory is intact. If the injured athlete is seen in the office setting, or several days after the injury occurred, it may be important that an athletic trainer, teammate, coach, or family member accompanies the athlete, especially if memory dysfunction or altered levels of consciousness has occurred. Determining if LOC occurred, and for how long, is best reported by an individual who has witnessed the injury. Athletes often mistake the period in which they were confused or disoriented as “unconscious.”
TABLE 14.3 Signs of Skull Fracture | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Determination of the extent of memory loss for events before the injury (retrograde amnesia [RGA]) or after the injury (PTA) is also essential when evaluating the head injured athlete and, as will be discussed later, may be the most sensitive markers for the severity of injury. In addition, if it is clear that the athlete is struggling in answering these questions, it is often more obvious to the athlete, coach, or parent that the athlete should not be allowed to return to participation. Aspects of the examination that are difficult to measure, yet remain important, include the athletes’ ability to follow commands and how quickly and smoothly they perform aspects of the examination. For example, a useful sideline evaluation of memory and information processing
speed is to ask an athlete to give the months of the year backwards from a selected month. Although the athlete may be 100% accurate with the information they provide, observing the difficulty and speed with which they are able to perform this is useful in the overall evaluation process. Unfortunately, unless these same tests have been performed by the athlete earlier, it is often difficult to know the exact extent of their deficits.
speed is to ask an athlete to give the months of the year backwards from a selected month. Although the athlete may be 100% accurate with the information they provide, observing the difficulty and speed with which they are able to perform this is useful in the overall evaluation process. Unfortunately, unless these same tests have been performed by the athlete earlier, it is often difficult to know the exact extent of their deficits.
Other symptoms of head injury, other than RGA, PTA, and LOC, include headache, nausea, dizziness, tinnitus, balance problems, and “feeling in a fog.” Difficulties associated with gait, vision, speech, or cranial nerve deficits may also occur. Common signs and symptoms of cerebral concussion are given Table 14.1. A complete neurological examination should be performed as soon as the athlete is cleared of cervical spine injury and/or skull fracture. This should include pupillary response, cranial nerve testing, upper and lower extremity strength and sensory function, reflexes, cerebellar examination, and evaluation of complex tasks, such as gait. Deficits should be noted, and serial examinations performed along with the assessment of symptoms. The athlete should be assessed immediately and serially after head injury to ensure that deterioration does not occur.
If symptoms worsen on examination, or mental status deteriorates, the athlete should be referred for further emergent evaluation. Guidelines regarding when further evaluation in an emergency facility is warranted are presented by the NATA (National Athletic Trainers’ Association) Consensus Statement on Concussion (61), as well as the Team Physician Consensus Statement on MTBI (62). In addition, the American Academy of Pediatrics has made recommendations in 1999 for the management of minor closed head injury in children (63).
Determining when diagnostic imaging is indicated is often difficult. If there is sustained LOC, concern for skull fracture, or any evidence of focal deficits, imaging should be considered. If an athlete has an initial lucid interval, then demonstrates a decline in mental status or worsening symptoms, imaging is indicated. The American Academy of Pediatrics found no indication for routine skull radiographs for minor head injury, and also stated that CT scanning was no different in individuals with or without LOC, and was no better than observation alone, thereby questioning the routine use of CT scanning in head injured children (63). Close observation is very important for the athlete who sustains MTBI, and it is essential to ensure that the athlete is not left alone. Determining which athletes require inpatient observation is often a challenge to the team physician. CT scanning is felt to be the best initial neuroimaging test acutely, given its ability to detect fracture and blood. These imaging studies are generally normal in concussion injuries, and are obtained to exclude skull or cervical spine fracture and/or other focal abnormalities discussed previously, such as intracranial bleeding and subdural or epidural hematomas.
Management of the Concussed Athlete
Once an athlete has been diagnosed with concussion, it is important to watch him/her closely, perform serial evaluations, and determine whether he/she requires inpatient observation, observation at home, or RTP. Though there is controversy regarding several aspects of concussion treatment and management, all agree that athletes with symptoms should not be allowed to continue play. Ensuring that no athlete is symptomatic requires diligent questioning of the athlete and calls for more than merely asking him/her “are you alright?” It is often beneficial to use a symptom checklist to ensure that no additional symptoms have developed. For those athletes who are symptomatic, placing them in a quiet and dark environment, away from severe environmental conditions, is helpful. Decisions regarding whether the athlete stays on the sideline or goes into the locker room can be made based on individual cases, but the injured athlete should remain supervised by qualified medical personnel at all times to watch for decompensation. Athletes who are not kept under observation should be given written instructions; these are often also given to a teammate, roommate, and/or parent/guardian. The take-home instructions should include avoiding alcohol or other drugs, avoiding aspirin or nonsteroidal anti-inflammatory medications, and signs and symptoms to watch for that
warrant emergency referral. Athletes should also be told to avoid any significant physical or mental exertion, which may exacerbate their symptoms. Finally, athletes should be given a time for follow-up evaluation, and should not perform any weight lifting or other exertional activities (gym class, bicycling, etc.) until re-evaluation has occurred.
warrant emergency referral. Athletes should also be told to avoid any significant physical or mental exertion, which may exacerbate their symptoms. Finally, athletes should be given a time for follow-up evaluation, and should not perform any weight lifting or other exertional activities (gym class, bicycling, etc.) until re-evaluation has occurred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree