Chapter 5 Head and Neck
1. Understand the structural components of the cervical region.
2. Be knowledgeable about the effects position has on the head and neck.
3. Explain the types of headaches.
4. Explain temporomandibular joint (TMJ) dysfunctions.
5. Understand the effects the muscles have on TMJ.
6. Explain the types of torticollis.
7. Explain the causes of whiplash.
The area of the head and neck is one of the most complex and overworked regions in the body. At some point in their lives most people will complain about a pain in their neck. Because of its structure and function, it is easy to understand why neck pain is so prevalent. Imagine a semisolid base holding a rod arced at 30-40 degrees, which supports a 10-pound bowling ball. This is the structure of the neck. The base of the neck is the torso, which consists of the thoracic vertebrae, rib cage, and sternum. The arced rod consists of the seven cervical vertebrae and their intervertebral discs. The bowling ball represents the head, which weighs an average of 8-10 pounds (Figure 5-1).
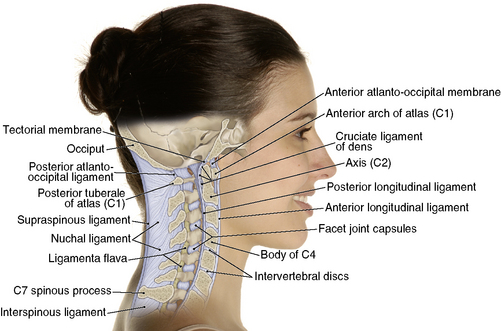
Figure 5-1 Structure of the neck.
(From Muscolino JE: The muscle and bone palpation manual with trigger points, referral patterns, and stretching, St Louis, 2009, Mosby.)
The cervical area has sacrificed structure to provide mobility, including extension, flexion, lateral flexion, rotations, and many combinations of these movements. This area is rich in nerves, ligaments, and musculature. The complex musculature of the neck is necessary for stabilization of the head, to maintain its balance, and to control these movements (Figure 5-2).
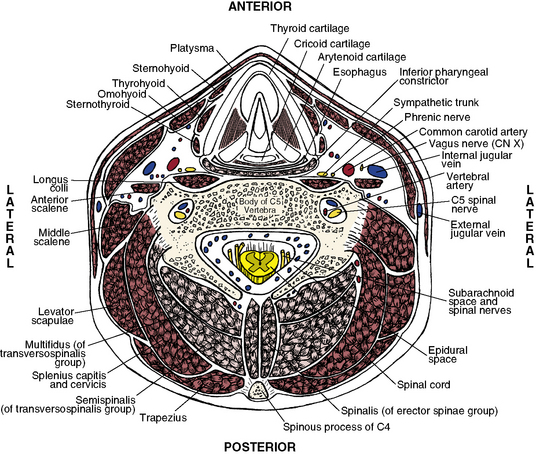
Figure 5-2 Cross-section of the neck.
(From Muscolino JE: The muscular system manual: the skeletal muscles of the human body, ed 3, St Louis, 2010, Mosby.)
The cervical spine is a complex area that also requires extreme caution because of its vascularization and nerves. The obvious concern while working with any region of the spine is the central nervous system. The spinal cord runs through the vertebral foramen and can be pinched or damaged with forceful movements. Although damage to the spinal cord is rare with therapeutic massage, the peripheral nerves, such as the cervical plexus (C1-C4) and brachial plexus (C5-C8) as they exit the spine, are susceptible to damage in massage therapy. Innervations from the cervical plexus feed the face and neck with the stimulus needed for movement and function. The brachial plexus feeds the arms and hands with their needed stimuli (Figure 5-3).
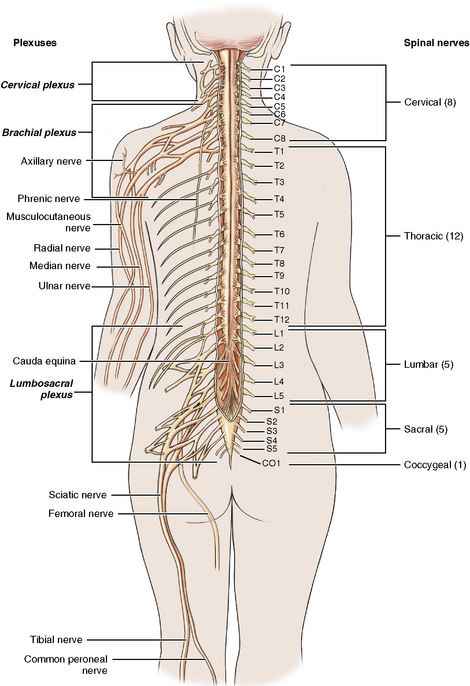
Figure 5-3 Cervical and brachial plexus.
(From Herlihy B: The human body in health and illness, ed 4, St Louis, 2011, Saunders.)
The vascular design in the cervical region raises additional concerns. Cervical vertebrae 1 through 6 contain a transverse foramen, which provides a protected pathway to the brain for the vertebral artery and vein. Because of the motion, especially rotation of the neck, this is a high-risk area. Rotating the neck to access tissues or applying a stretch can apply pressure to these vessels, which can result in fainting, nausea, and vertigo. This potential to pinch or compress the vertebral artery happens at approximately 45-50 degrees of rotation. On the anterior aspect of the neck the carotid artery and jugular vein hide under the sternocleidomastoid (SCM). The carotid pulse is palpated here as these vessels are superficial in the body. If at any time you are working on the anterior aspects of the neck and feel a pulse, you should change the positioning of your hands (Figure 5-4).
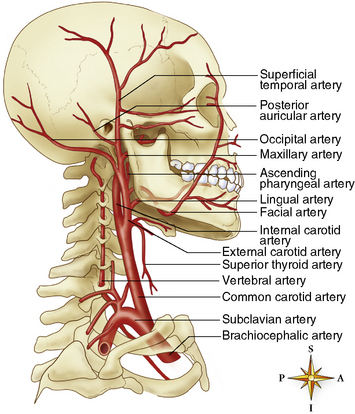
Figure 5-4 Vessels of the neck.
(From Patton KT, Thibodeau GA: Anatomy & physiology, ed 8, St Louis, 2013, Mosby.)
Migraines and headaches
Tension headaches
Tension headaches originate from a mechanical stress or exertion. This could be tightening of the musculature caused by body alignment, poor ergonomics, or stress, among many other things. In most cases, the musculature is overworking to maintain proper alignment of the skull. Although many therapists begin working the trapezius muscles, the root of the muscular tension is typically in the suboccipital muscles. This group of intricate muscles plays an important role in maintaining the balance of the head. They help to stabilize the atlas (C1), axis (C2), and the base of the occiput. As tension builds in the superficial muscles of the body, the suboccipital muscles contract to maintain proper head alignment. Because of the tension on the suboccipital muscles, intervertebral compression may occur in this area, resulting in headaches (Figure 5-5).
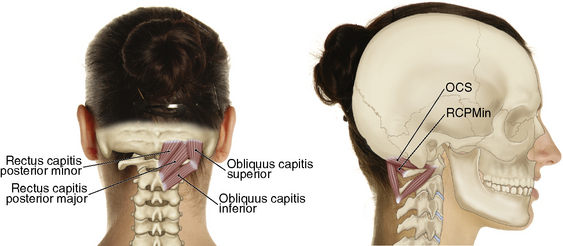
Figure 5-5 Suboccipitals.
(Muscolino JE: The muscle and bone palpation manual with trigger points, referral patterns, and stretching, St Louis, 2009, Mosby.)
Other muscles that play a role in tension headaches are the trapezius, levator scapulae, scalenes, splenius, SCM, and some muscles of the jaw. Each muscle has a pain referral pattern that can help identify the muscles affected. A clear and detailed discussion during the client-intake process helps identify these muscles (Table 5-1).
| Muscle | Referral Pattern |
|---|---|
| Frontalis | Local discomfort occurs above the eye. |
| Levator scapulae | Refers pain to the base of the neck, top of the shoulder, and vertebral border of the scapula. |
| Occipitalis | Local discomfort occurs at the back of the head. |
| Scalene group | Commonly refers pain to the top of the shoulder and down the lateral arm into the first three digits. |
| Splenius capitis | Refers pain to the top of the head. |
| Splenius cervicis | Refers pain to the back of the neck and temporal area. |
| Sternocleidomastoid | Sternal head refers pain to cheek, temporal area, and behind the ear. Clavicular head refers pain behind the ear and above the eyes. |
| Suboccipitals | Refers discomfort in a headband-like area around the eye and above the ears. |
| Trapezius | Upper fibers refer discomfort to the eye, ear, and lateral neck. |
Migraines
Clients often say that there is no experience that comes close to the pain and discomfort of a true migraine. Migraines are vascular-based headaches affecting the vessels surrounding the brain. People often experience nausea and vomiting, chills and sweating, extreme fatigue, and visual disturbances. These are often debilitating, causing the person to miss work and stay in bed. Some people experience extreme sensitivity to light and sound. Migraines are often triggered by sensitivity to foods, alcohol, and other drugs, stress, weather changes, sleeping patterns, and posture. They affect women more than men because of hormonal influences (Box 5-1).
Working with headaches
The focus of the session should be on reducing the trigger points, tight muscles, skeletal imbalances, and increasing ROM of the neck. Work through the layers; start with warming the tissues and the superficial fascia of the area. Address any trigger points or hypertonic tissues found in the upper trapezius muscles. Address the restrictions found in the levator scapulae and SCM using compressive, stripping, and lengthening techniques. As you progress deeper to the splenius and suboccipital muscles, myofascial stretching and compression are effective approaches. Finish the region with joint movements and stretching to help with the neuromuscular reeducation (Sequence 5-1).









