27
Hand Fractures
The hand is used in nearly every vocational and avocational human activity. It is often called the third eye of the body. As such, it is at times subjected to a wide variety of deforming forces, many of them significant. A fracture results when the integrity of a bone is compromised from an external force.1 Metacarpal and phalangeal fractures are some of the most common fractures that occur in the human body, second only to forearm fractures. Hand fractures account for up to 10% to 20% of all fractures in adults and children.2,3 Without proper management by a physician and/or therapist, these injuries can become functionally disabling, adversely affecting the patient’s work, family, independence, and well-being.
General Timelines and Healing
Immediately following a fracture, the body enters a three-phase, bone healing process. The first stage is the inflammatory phase. The second stage is the repair phase. The third phase is the remodeling phase. In the inflammatory phase, the body sets in motion the cellular and vascular activity necessary for hematoma formation and primary stabilization. During the repair phase, the body removes the hematoma and damaged cells and lays down callus bone, further stabilizing the fracture site. In the third phase, the callus is gradually replaced with true bone tissue over the following months and years. Given the right healing environment, the once fractured bone will return to pre-fracture strength. A stable fracture will heal itself via this ordered process of inflammation, repair, and remodeling, which is also known as secondary healing.2
A fractured bone requires stability at the fracture site in order to heal properly. If there is instability, delayed healing or non-union may result. Some fractures do not require significant medical intervention for normal healing to occur. These fractures are described as non-displaced (that is, the fractured fragments remain properly aligned). Displaced (poorly aligned) fractures require physician manipulation in order to restore proper anatomical alignment, which is also known as reduction.4,1
After reduction, the physician determines whether or not the fracture is stable. Unstable fractures displace spontaneously or with motion and may require some form of internal or external fixation. This allows the bone to heal without any malrotation, angulation, or malunion. External fixation can be achieved via external orthoses or casts. Internal fixation is achieved via internal placement of screws, plates, and or pins across an anatomically aligned fracture. An external cast or custom orthosis may be used to protect the fracture, even after internal fixation. There are instances when a severely comminuted (fragmented) fracture requires traction to realign the bony fragments. An external fixator accomplishes this task by attaching a low-profile scaffold system to the proximal and distal portions of the fracture. The physician adjusts the tension to appropriately align the fragments. Advances in internal fixation methods over the past several years have led to less frequent use of external fixators (Fig. 27-1).

Severe third metacarpal fracture from gunshot wound stabilized with external fixator.
Improved internal fixation technology and surgical techniques allow physicians to secure bone fragments through open surgery using metal plates and screws, called open reduction internal fixation (ORIF). The healing process, in these cases, bypasses the secondary process of callus conversion to bone. This is called primary healing. By securing fracture fragments with plates and screws the physician eliminates interfragmentary gaps and provides the adequate stability required for bone healing, effectively substituting for external callus.2
ORIF also has some disadvantages. In order to access the bone, the surgeon must dissect through soft tissue, and as a result scar and potential adhesions will develop. Potential infection is also a disadvantage to internal fixation. Additionally, one cannot underestimate how surgical management affects the intimate nature of the soft tissue in the hand. Plates and screws may interfere with soft tissue mobility, such as tendon gliding. This is especially a problem when the places and screws are placed dorsally.1–3
Secondary fracture healing typically requires approximately 7 to 8 weeks. This often depends on location and type of fracture and, therefore, may require a longer duration of healing. Controlled AROM of joints just proximal and distal to the fracture may typically begin around 5 to 6 weeks, and sometimes earlier depending on the patient’s health and speed of healing. Light activities of daily living (ADLs) may begin during this time. Approximately 2 weeks after AROM is initiated, and when edema is not a problem, passive range of motion (PROM) may begin, which may include static progressive or dynamic splinting as needed. Resistive exercises may typically begin 8 to 10 weeks after initial reduction and stabilization, but bone healing and absolute stability must be first confirmed by physician prescription.1
There has been a recent shift in fracture treatment protocol in the literature with evidence suggesting that early AROM of proximal and distal joints of an extra-articular fracture may assist to prevent stiffness, improve strength and stability of the fracture, and improve alignment of the fracture.2,5
Early AROM may sometimes begin before actual radiographic evidence of healing, most often between 3 and 6 weeks. In this situation, the physician must prescribe, the therapist must educate, and the patient must be completely compliant. The therapist may also need to fabricate a fracture brace to provide sufficient stability and protection to the fracture externally in order to avoid displacement during this controlled motion. If the therapist believes that the patient will have poor compliance, then early AROM should not be attempted. In general, fracture bracing and subsequent early AROM is intended for simple, minimally displaced, extra-articular fractures of long bones.6 Judy Colditz provides an excellent review of fracture bracing in Chapter 127 of Rehabilitation of the Hand and Upper Extremity, edition 6.6
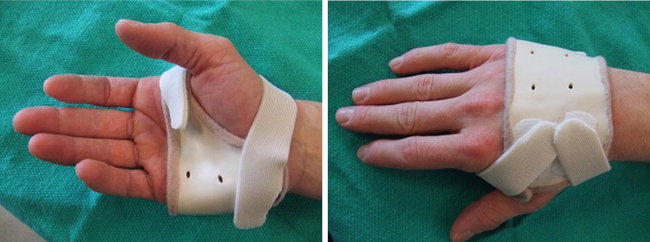
The purpose of fracture bracing is to provide sufficient stabilization and alignment to fracture fragments while regional joints are engaging in AROM. The fracture brace provides circumferential support of the long bone and is fabricated to be adjustable in order to accommodate for fluctuations in edema, while allowing for full range of motion (ROM) of the proximal and distal joints6 (Fig. 27-2). Again, fracture bracing is recommended for extra-articular, stable fractures. More specific details regarding fracture bracing will be discussed in the respective metacarpal and phalangeal sections.
While a philosophical shift has taken place over the past 5 to 10 years, early, controlled AROM is still “generally not recommended during the first 3 weeks of healing.”5 Some clinicians may consider it unsafe, while others may consider it unnecessary, citing that without the intra-articular nature of the fracture, early motion will not provide a functional benefit.5 Indeed, several authors conclude that clinically, early AROM and fracture bracing makes sense, although the literature still does not support or refute it. They agree that further research needs to be done.2,5,7 It is the experience of this author that early AROM of both stable and unstable, extra-articular fractures should be on a case-by-case basis. It is of utmost importance that the patient be 100% compliant with the protocol—if compliance is questionable, do not proceed. Furthermore, if there is concern that the patient’s joints will increase in stiffness faster than average, then early mobilization should be considered.
As mentioned earlier, the soft tissues in the hand are intimately associated with the bones. The forces required to fracture a bone often and inevitably result in surrounding soft tissue injury.1,4,5 Soft tissue injuries associated with metacarpal and phalangeal fracture may include peripheral or digital nerve injury, joint capsule and/or ligament injury, and tendon and/or tendon sheath injury, in addition to the sometimes adverse effects of scar formation or reduced tendon gliding. Secondary joint lag, contracture, and decreased muscle strength, endurance, and flexibility may also develop as a result of the soft tissue injury following a fracture in the hand.1,2 The more complicated the injury and/or subsequent surgery, the more important it is to begin therapy early in order to avoid as many complications of immobilization as possible. Indeed, that is typically the purpose of the extensive surgery; to provide significant rigid fixation in order to begin early motion. The therapist needs to recognize complications early and must communicate his or her findings to both the patient and the physician. He or she must also use this information to appropriately modify the plan of care to improve outcomes.
This topic will continue to be discussed and debated over the next several years. For more information see Feehan’s work.2,5
Early Mobilization
Early mobilization is obviously not appropriate for every hand fracture treated by physicians and therapists. When a patient comes to therapy with a fracture, the therapist needs to be able to identify who is a good candidate to begin early mobilization and who isn’t. Typically, early mobilization is considered appropriate for extra-articular hand fractures in one of two situations: 1) a stable, closed, non- or minimally-displaced fracture, and 2) when a fracture has been immobilized with rigid fixation, either externally or internally. Fractures that don’t fall into these two categories are generally not recommended for early mobilization due to the increased chance of displacement and subsequent malunion or nonunion.5 Feehan points out, however, that there may be a place for early mobilization in potentially unstable fractures that are not clear surgical candidates.
Feehan2 describes several clinical factors that are important to consider before beginning early mobilization:
1. Fracture location: In which bone and where in that bone is the fracture located? The therapist and physician need to know the potential deforming forces that surround the particular fracture (for example, intrinsic and/or extrinsic muscle force vectors).
2. Fracture pattern and amount of displacement: Multiple fracture lines and greater than minimal displacement will require a period of immobilization due to decreased structural stability.
3. Type of fracture reduction and type of hardware used: Was it reduced via open or closed techniques? Is it rigid, coaptive, or stable fixation?
4. Nature of the surrounding soft tissue injury: For example, if a ligament is torn in addition to the fracture, the therapist’s treatment plan will need to take this into consideration.
5. Patient’s daily functional demands: This information will assist the therapist in predicting the types of daily functional stresses that will be put on the injury. For example, an office worker will have different functional demands than a firefighter.
6. Timing or stage of healing: This will assist the therapist in determining how much additional internal strength has been added by the healing bone.
Early mobilization should be gentle, generally pain-free, supervised, and engaging. The motion of the joint proximal and/or distal to the fracture should be moved through an arc that does not risk reproducing displacement of the fracture.5 Feehan states that there are many different ways to perform early mobilization. One may delay early mobilization for a few weeks. Fracture bracing may also be used in order to stabilize a fracture while proximal and distal joints are actively ranged. If AROM is not an option, then one may consider gentle PROM with the fracture supported. Feehan states, “The advantage of making this clinical determination (to begin early mobilization or not) early in the fracture healing process is that it is possible to move from categorizing a fracture as either clinically stable or clinically unstable and to think instead in terms of what clinical factors or variables would need to be controlled to maintain fracture structural integrity and still allow for some form of early joint motion.”5
Evidence-Based Treatment
The landscape of health care is changing. Third-party payers from Medicare, to Labor and Industries, to private insurers are moving toward requiring outcome-based measures to document improvement and necessity for therapy before they issue payment. An objective measurement tool should be used to document need for services. There are several upper extremity based, reliable, and valid outcome measures available for therapist use, including but not limited to the Disabilities of the Arm, Shoulder, and Hand (DASH), QuickDASH, Jebson Taylor Hand Function Test (JTHFT), Minnesota Rate of Manipulation Test, Motor Assessment Scale (MAS), Functional Independence Measure (FIM), Hand Function Survey (HFS), Michigan Hand Questionnaire (MHQ), Upper Extremity Functional Scale (UEFS), and Arthritis Hand Function Test (AHFT). The most popular assessment seems to be the DASH and the QuickDASH. It is important for each hand therapist and/or clinic to review potential outcomes measures, weigh the pros and cons of each, choose one or two to implement, and then be consistent with its use in the clinic. Future payment may likely depend on it.8
Metacarpal Fractures
“Metacarpal fractures are common and account for 18% of all fractures in the hand and forearm.”9 This percentage increases from 30% to 50% when isolated to only the hand.10,11 Most metacarpal fractures (up to 85%) occur in men, and the most commonly fractured metacarpals are the fourth and fifth, typically from punching-type injuries.9 The clinician must know and understand the anatomy of the metacarpals and the soft tissues surrounding them, thereby understanding the deforming forces that act on these fractures.
Metacarpal Anatomy
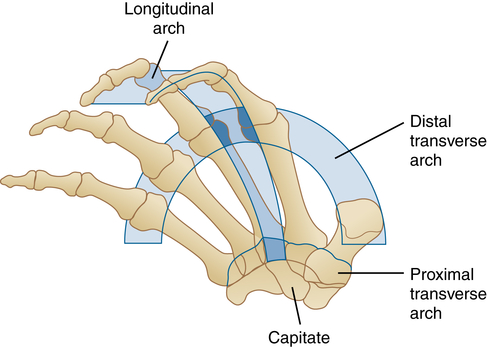
The metacarpal is described as a miniature long bone, composed of a cortical bone shaft (or diaphysis), and proximal and distal ends composed of cancellous bone. The diaphysis is covered by periosteum (the outer lining that envelopes the bone). The proximal and distal ends are called the epiphyses. These ends are covered by articular cartilage (hyaline cartilage that covers the articular surfaces), which is necessary for smooth, pain-free AROM. Metacarpal bones are concave in nature with the concavity being volar.11 This concavity allows for space for the long flexors and lumbrical muscles to be “tucked away,” as well as to slide over.10 The rich blood supply to the metacarpals permits fractures of these bones to heal well. Generally, the cancellous bone heals more efficiently than cortical bone.1,10 The head of the metacarpal is located at the distal end, with the neck, being just proximal. The most proximal end is called the base. The base is connected to the neck and head via the shaft. The five metacarpals vary in length and girth. The longest metacarpal is the index finger, followed by the middle, ring, and small fingers. The thumb metacarpal is the shortest10 (Fig. 27-3). With the decrease in length, there is also diminution of stability, thereby making the thumb metacarpal the most mobile. The increased mobility on the most radial and ulnar side of the hand allows for a natural curvature of the hand that provides the ability to successfully perform both gross and fine motor hand functions, from grasping a steering wheel to holding and counting change. The arch created by the rigid index and middle metacarpals is the longitudinal arch. The rigid nature of these metacarpals is due to the interlocking quality of the metacarpals on their respective carpometacarpal (CMC) joints. There are two transverse arches in the hand, a proximal transverse arch and a distal transverse arch (Fig. 27-4). The proximal transverse arch is created by the interlocking carpal bones. Deep ligaments to the metacarpal heads support the distal transverse arch. Extrinsic and intrinsic muscles also lend support to this functional, skeletal arch system.
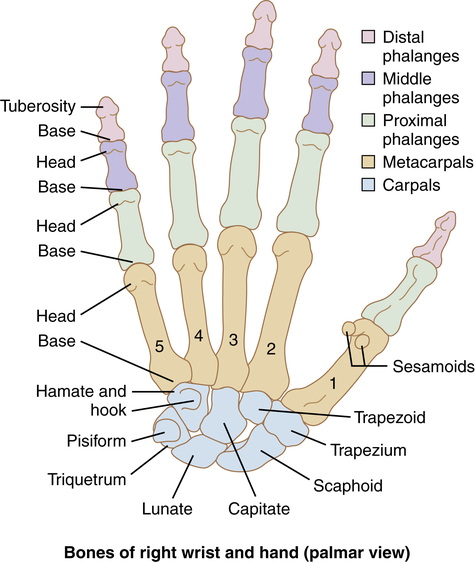
Volar view of the bones of the hand and wrist. (From Pratt NE: Anatomy and kinesiology of the hand. In Skirven TM, Osterman AL, Fedorczyk JM, et al, editors: Rehabilitation of the hand and upper extremity, ed 6, Philadelphia, 2011, Mosby Elsevier.)
Diagnosis and Pathology
Fractures of the metacarpals most often occur in the first and fifth metacarpals. This happens for a couple of reasons. First, they are the border digits and are the most exposed. Second, they are the most mobile.1,11 Soong, et al. reports that the fourth metacarpal is also frequently fractured because it has the most narrow shaft diameter. Diagnosis is definitively made with x-ray. The angulation, displacement, and malrotation of the fracture are factors in determining the need for surgery.
Fractures of the metacarpal may occur anywhere along the bone, base, shaft, neck, or head. Each of these areas will be discussed in more detail in the “Timelines and Healing” section. Base fractures are the least common because of their stability. They usually occur as a result of a heavy direct blow or crush injury. Shaft fractures typically occur due to torsion, direct impact, or longitudinal compression. Depending on the number of fragments and/or line of the fracture, it may be classified as transverse, comminuted, or oblique. Malrotation and/or bone shortening often result from an oblique fracture. Dorsal angulation results from a transverse fracture due to the volar vector forces of the interossei and long flexor muscles.1,2
There are several specific metacarpal fractures that have identifiable names. The first is a boxer’s fracture (though a skilled boxer rarely sustains this type of fracture).9 A boxer’s fracture is one in which the metacarpal neck is compromised. Amount of displacement and comminution varies depending on the force that caused the injury. The force tends to be a compressive force that travels proximally from the metacarpal head toward the base, typically occurring when the head of the fifth (and sometimes fourth) metacarpal comes in contact with something solid with the digits in full composite flexion.1,10
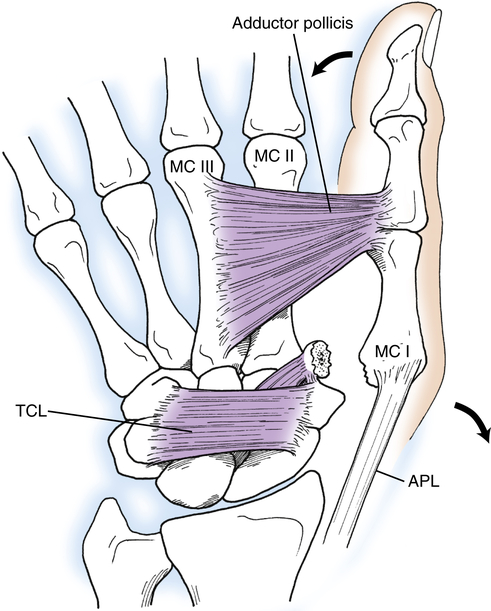
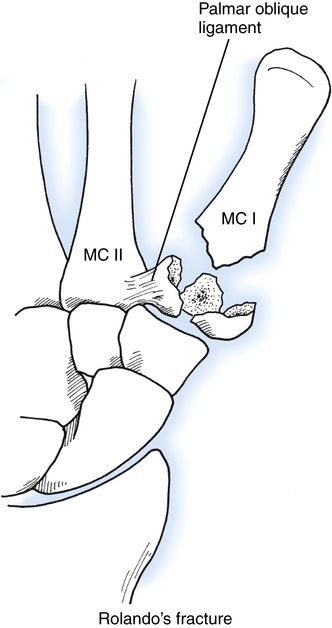
The second well-known metacarpal fracture occurs at the thumb metacarpal base and is known as a Bennett’s Fracture. A Bennett’s fracture is intra-articular at the first CMC joint (Fig. 27-5). This fracture occurs when there is forced first CMC abduction and an axial blow along the metacarpal shaft when the metacarpal is slightly flexed. A stabilizing ligament, the palmar, oblique ligament, or beak ligament, causes an avulsion fracture of the ulnar aspect of the first metacarpal base. Often, these avulsion fractures result in dislocation of the trapeziometacarpal joint. Furthermore, due to the competing forces of the adductor pollicus and abductor pollicus longus tendons, the type of axial blow listed earlier results in dislocation and subluxation of the first CMC joint. Rolando’s fracture is a fracture of the metacarpal base that presents with a “T” or a “Y” fracture pattern that splits the articular surface of the base of the first metacarpal1,10,12 (Fig. 27-6).
Timelines and Healing
Metacarpal fractures tend to be quite stable secondary to their multiple muscle and ligament attachments. Metacarpal fractures tend to heal in 3 to 7 weeks with variables of age, nutrition, genetics, stability, and amount of displacement affecting this timeline.1 If the fracture is not recognized or treated appropriately, the aforementioned normal stabilizing soft tissue forces may cause debilitating deformities. It is important for therapists to recognize this. For example, the volar displacement of the fifth metacarpal head in the boxer’s fracture results in a disruption of the normal arch of the hand, which adversely affects hand function and weakens grip strength.
Base Fractures
As mentioned earlier, base fractures are not common, especially of the second and third metacarpals. If a metacarpal base fracture occurs, it may demonstrate a small amount of rotation. This is significant in that this small rotation will be magnified many times at the distal end of the digit.10
Shaft Fractures
Fractures of the metacarpal shafts are typically stable enough that they may tolerate early mobilization well, which is discussed in more detail at the end of this section. The apex dorsal angulation of the fracture can be aesthetically displeasing and may result in impingement or rupture of the extensor digitorum communis (EDC) if left untreated.10 Any angulation in the index and middle fingers needs to be corrected. As a general rule, angulations greater than 20° in the ring finger and 30° in the small finger need to be corrected. Multiple metacarpal fractures as well as unstable fractures will need to be stabilized by ORIF utilizing plates, lag screws, or Kirschner wires (inserted in either a closed or open manner).10
Neck Fractures
A neck fracture is the most common metacarpal fracture seen in the hand clinic. Orthotic fabrication and fitting is required with both conservative and post-surgical treatment. Of course, there is more freedom of movement following ORIF. Surgery is generally required when the dorsal angulation is greater than 15° for the ring and small finger.10 Decreased metacarpophalangeal (MP) AROM and failure of the small finger to initiate grip result from angulated small and ring finger neck fractures greater than 15°. Some surgeons may avoid surgery with small finger metacarpal neck fractures less than 30° and ring finger neck fractures less than 20°.13 Displaced, untreated, and/or improperly treated metacarpal neck fractures will often result in a pseudo-claw deformity in addition to decreased ROM at the MP joint. Tenderness in the palm also develops during grip due to the volarly-displaced metacarpal head. These fractures are usually splinted or casted in the intrinsic plus position of MP joint flexion of 70° to 90° with the interphalangeal (IP) joints free to flex and extend. The affected digit will often require buddy taping to the adjacent digit to avoid any malrotation of the metacarpal head.
Head Fractures
Head fractures are uncommon, but serious in nature, because they tend to be intra-articular. If less than 20% of the metacarpal head is involved (and non-displaced), then treatment tends to be conservative. The therapist will fit the patient with an ulnar or radial (depending on which metacarpal head is fractured) wrist, hand, finger, gutter orthosis with the wrist in 0° to 20° of extension, the metacarpal flexed as close to 90° as possible, and the IP joints in 0° of extension. The therapist includes the adjacent digit for increased stability and comfort. ORIF is generally indicated if more than 20% of the articular surface is involved.10 If ORIF is performed, it is important to begin motion and scar management techniques as soon as possible after surgery. Without immediate motion and scar management, tendon and capsular adhesions may develop from the longitudinal surgical incision, thereby preventing full AROM of the MP joint.1
Thumb Metacarpophalangeal Fracture-Dislocation (Bennett Fracture)
In most cases, surgical intervention is required due to the intra-articular nature of these injuries. The stout beak ligament mentioned previously is rarely torn; so when forces are strong enough to tear it, the ligament maintains its hold on the first metacarpal base and avulses a piece of bone from the ulnar aspect of the base (see Fig. 27-5). The bony fragments are often greater than 25% of the joint surface or simply irreducible, which are the criteria for internal fixation.12,13 Stability is compromised significantly with these fractures. Following surgical repair (usually via Kirschner wires), the surgeon immobilizes the fracture for approximately 4 to 6 weeks in a forearm-based thumb spica cast. IP joint AROM may be allowed after 2 to 3 weeks depending on surgeon preference. The surgeon removes the pins after the 4 to 6 week immobilization period. Because the fracture is intra-articular, it should have continued protection in a hand- or forearm-based thumb spica orthosis for another 3 to 6 weeks. If rigid internal fixation has been utilized, IP joint movement may be allowed after 1 week. Resistive exercises are avoided until there is radiographic evidence of stable fracture healing, which is typically after 3 months.12
Thumb Metacarpal Shaft Fractures
Due to the high mobility of this particular metacarpal, shaft fractures are rare. Forces strong enough to fracture this bone are often dissipated to the more stable base, where the fracture will occur. Indications for reduction are similar to small finger metacarpal shaft fractures (that is, dorsal angulation greater than 30°). Post fracture treatment (post reduction or ORIF) includes 3 to 4 weeks of immobilization in a thumb spica cast/orthosis with the IP joint included. If the fracture requires more time to heal, IP joint mobilization may be considered after the initial 3 to 4 week time period.10–13
Thumb Metacarpal Head Fractures
The most common fracture of the metacarpal head comes from radial directed forces that can tear the ulnar collateral ligament (UCL), which provides lateral stability on the ulnar side of the thumb. Rupture of this ligament often results in an avulsion fracture. This particular fracture is coined skier’s thumb. Non-displaced injuries are treated with immobilization in a forearm-based thumb spica cast or custom orthosis with the IP joint included. The IP joint portion may be removed to encourage motion after 4 weeks, as long as there is evidence of fracture healing. Displaced fractures need to be stabilized via Kirschner wires or ORIF. This improves joint congruence.10
Early Motion for Metacarpal Fractures
The deforming forces, malunion pattern, and common soft tissue complications were discussed previously and need to be considered carefully before deciding to begin early mobilization. The orthotic design for the resting position should hold the MPs in at least 70° of flexion at rest. As the fracture heals, this may be serially reduced to allow for more motion at proximal and distal joints. A fracture brace could also be fabricated in order to provide stabilization to the fracture site, while allowing functional, uninhibited motion of the proximal and distal joints (Fig. 27-7; see also Fig. 27-2). One must be careful with exclusive use of a fracture brace due to skin breakdown from the counterforce pressure points.13
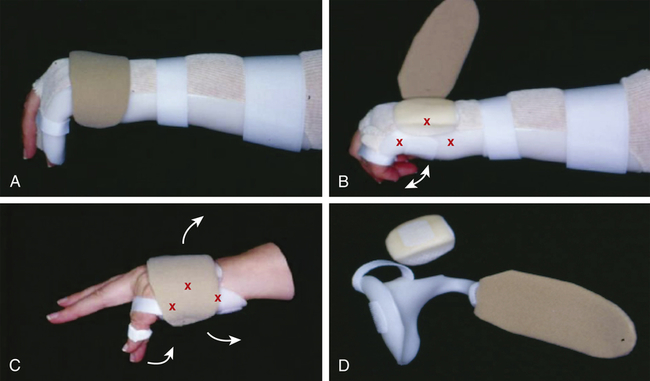
A, A volar-based orthosis that holds the wrist, hand, and fourth and fifth fingers in a position of function with and adjustable dorsal circumferential strap across the metacarpal region. B, The dorsal strap is removed to expose a three-point counter pressure, semi-rigid insert that adds additional fracture support. The orthosis has been serially reduced to allow proximal interphalangeal (PIP) and distal interphalangeal (DIP) motion. C, Further serial reduction to free the wrist with a buddy strap distally to control rotation of the finger during motion. D, The component parts of the same orthosis shown in C. (From Feehan LM: Extra-articular hand fractures part II: therapist’s management. In Skirven TM, Osterman AL, Fedorczyk JM, et al, editors: Rehabilitation of the hand and upper extremity, ed 6, Philadelphia, 2011, Mosby Elsevier.)
Treatment: Non-Operative and Operative
In general, therapeutic management of metacarpal fractures is similar, regardless of the location of the fracture. Initial immobilization is necessary and is achieved by fabricating a radial or ulnar gutter orthosis or cast (depending on which metacarpal was fractured). The orthosis or cast may also be volar-based (see Fig. 27-7). The MP joints are held in a position of 70° to 90° in order to minimize MP joint contractures. The IP joints are held in 0° of extension. The wrist is held in approximately 20° of extension. The surgeon may allow for the IP joints to be free if there is low concern for displacement, such as after rigid fixation or a stable shaft fracture. If IP joints are free, the therapist must take care to allow for unimpeded proximal interphalangeal (PIP) joint flexion by making sure the orthosis sits proximal to the PIP joint. If the thumb metacarpal is fractured, a basic thumb spica orthosis/cast is fabricated with care to maintain the web space. The thumb IP joint is typically included in the orthosis initially and is allowed more controlled motion after sufficient healing has occurred. The therapist must mold the orthoses with care to maintain the longitudinal and transverse arches of the hand.1,10,12
Once the patient has been immobilized, he/she needs to be educated on AROM exercises of all uninvolved joints. Edema occurs often following metacarpal injuries and surgeries. The therapist should educate the patient on proper elevation (for example, elevation above the heart, but without full elbow flexion) and icing techniques. Icing techniques should be utilized in the acute post-injury or post-operative phase. Manual edema mobilization (MEM) is more effective in the sub-acute and chronic phases. AROM of uninvolved joints is also very effective in edema reduction. If percutaneous pinning has been used and the surgeon left the pins exposed, the client must be instructed in pin care (see Chapter 25 for specific pin care instructions).
Closed Reduction
Once the physician has determined sufficient stability at the fracture site, controlled AROM of the wrist and MP joints may begin. This is typically 3 to 5 weeks post injury. As discussed previously, if the fracture is extra-articular and stable, early mobilization should be considered. If the fracture falls into the “gray” area (that is, is not stable) but the patient is not a clear surgical candidate, early mobilization might also begin within 1 to 2 weeks following the fracture. If the therapist, physician, and patient choose this route, 100% compliance must be assured. Typically, between 6 to 7 weeks, gentle PROM may be added to the treatment, both in the clinic and at home. Resistive exercises may be added only after adequate healing has been determined by the physician, typically between 6 and 8 weeks. Resumption of normal activities without restriction is usually around 10 to 12 weeks.2,10,12,13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



