Great Toe Transfer Thumb Reconstruction
Jonathan Amer Zelken
James P. Higgins
INTRODUCTION
Absence of the thumb can be broadly classified into congenital and acquired deformities. The spectrum of congenital thumb hypoplasia is conventionally addressed with augmentation (i.e., web space deepening) in less severe forms or pollicization of the index finger in more profound deficiencies (i.e., Blauth stage IV or V hypoplasia). Free toe transfer reconstruction is not preferred in this setting because of the absence of radial-sided anatomic support structures that would be required to yield optimal results (i.e., carpometacarpal [CMC] joint, thenar musculature, extrinsic tendons, radial artery, etc.).
Free toe transfer reconstruction is most commonly employed in acquired absence of the thumb, whether traumatic (amputations, failed replantation) or extirpative (amputation performed for infection, neoplasm). Either the first or the second toe may be transferred for digit reconstruction. Due to its small size and breadth, the second toe is generally used to reconstruct digits 2 to 5, or in pediatric posttraumatic thumb reconstruction. The great toe provides a stronger and better cosmetic result (1,2). A systematic review suggests there may be improved survival, total active motion, grip strength, and key pinch strength in great and trimmed great versus second toe transfer. Furthermore, patients were more satisfied with the recipient site function and aesthetics after trimmed great toe transfer (3). Both techniques confer similar sensory outcomes (4,5).
This installment will describe the technique of great toe transfer for acquired absence of the thumb.
INDICATIONS AND CONTRAINDICATIONS
The ideal setting for great toe reconstruction is posttraumatic or postsurgical absence of the thumb at, or distal to, the level of the metacarpal neck, with a supple and stable CMC joint, functioning thenar musculature, available digital nerves for reinnervation, and a generous soft-tissue envelope. These criteria are not required for successful great toe reconstruction but provide the best opportunity for functional success.
Bone Length
The morbidity of harvest of the great toe is minimized by harvest distal to the metatarsophalangeal (MTP) joint. This allows for flexion of the MTP joint via the flexor hallucis brevis and aids propulsion. It also preserves the windlass mechanism, wherein the plantar fascia inserts into the base of the proximal phalanx and flexes the first metatarsal, allowing it to bear the majority of body weight during the stance phase of gait (6). Finally, harvest at this level maintains joint capsular integrity, the position of the volar plate, and sesamoids. The length of the great toe is sufficient to reconstruct thumb defects at the metacarpal neck or through the metacarpophalangeal (MCP) joint by
performing an MCP/MTP arthrodesis. If the thumb amputation is through the shaft of the proximal phalanx, osteosynthesis can be performed at the diaphysis of the respective proximal phalanges. If the thumb amputation is through the interphalangeal joint (IPJ), the toe transfer can be prepared by removal of the proximal phalanx and stabilized by arthrodesis through the IPJ.
performing an MCP/MTP arthrodesis. If the thumb amputation is through the shaft of the proximal phalanx, osteosynthesis can be performed at the diaphysis of the respective proximal phalanges. If the thumb amputation is through the interphalangeal joint (IPJ), the toe transfer can be prepared by removal of the proximal phalanx and stabilized by arthrodesis through the IPJ.
Thumb amputations at, or proximal to, the metacarpal shaft pose a particular challenge. The surgeon may elect to perform the great toe transfer with intercalary corticocancellous bone graft (i.e., iliac crest) to restore length not provided by the great toe (7). Alternatively, a second toe transfer may be performed with adequate length of metatarsal to achieve direct metatarsal/metacarpal osteosynthesis.
CMC Joint and Thenar Musculature
Great toe transfer reconstruction does not routinely provide significant MCPJ or IPJ range of motion (3,8). Trimmed great toe transfer has shown to result in even less IPJ motion, presumably since the capsule is invaded and the joint osteotomized by design (9). Its success is predicated on a stable and mobile CMC joint providing multiplanar motion. The ideal setting for successful reconstruction is one where the CMCJ is uninjured, supple, and powered by healthy innervated thenar musculature. If the trauma has fractured or ankylosed the CMCJ, amputated the entire metacarpal, or destroyed all of the thenar musculature, the reconstruction will be minimally functional. The surgeon and patient have to weigh the benefit of toe transfer reconstruction anticipating the thumb serving only as an immobile digit, with all prehension dependent on the mobility of the nonthumb digits. The surgeon should not consider the repair/reconstruction of the extensor and flexor pollicis longus (EPL and FPL) as a reasonable substitute for thenar musculature, as they will not provide coordinated CMC motion.
Sensory Nerves
In routine toe transfer thumb reconstruction, the toe digital nerves are coapted to the amputated stumps of the thumb digital nerves in the field of dissection just proximal to the traumatic scar. This provides tension-free atraumatic nerve coaptations near the sensory targets. In traumatic thumb avulsion injuries, however, the digital nerves may be avulsed from the median nerve in the carpal tunnel. In this setting, the surgeon and patient should plan on digital nerve sensory transfers from nearby noncritical dermatomes (typically the common and proper digital nerves to the third web space) and anticipate the donor site deficit inherent to the nerve transfer. Regardless of the multitude of technical aspects of toe transfer reconstruction, the surgeon should always mind the critical importance of sensory return in the ultimate use or neglect of the transferred toe by the patient (10,11).
In the rare setting of trauma involving thumb amputations and concomitant forearm level median and/or ulnar nerve injuries, the ability to restore sensation must be critically assessed. A complete median nerve sensory loss, for example, may be a contraindication to thumb reconstruction unless nearby donor nerves (i.e., digital nerves to the fourth web space) are available and deemed expendable for transposition to the toe transfer.
Skin Envelope
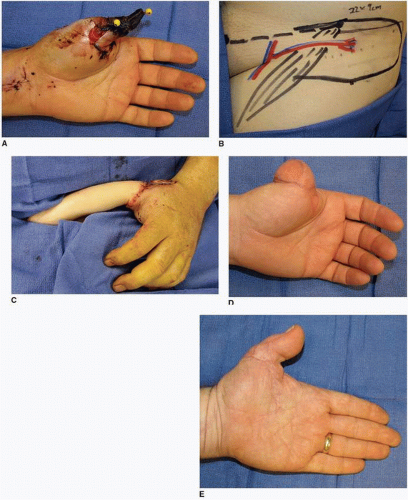
This is the least stringent of the listed requirements for toe transfer reconstruction of the thumb, but still deserves considerable preoperative attention. The great toe donor site provides very limited skin from the dorsal and plantar surfaces. If the thumb amputation site has firmly adherent scar tissue and there is no supple or excess soft tissue, the skin envelope will likely be inadequate for skin closure upon completion of the toe transfer procedure. Skin grafts may be employed if the wound bed permits (Fig. 35-1). Alternatively, staged reconstruction may be considered. The first stage involves
providing excess soft-tissue coverage of the amputation stump. This is commonly performed using a pedicle groin flap or free fasciocutaneous flaps (i.e., lateral arm, anterolateral thigh flaps). When the skin has healed and edema resolved (usually 2 or 3 months after skin flap procedure), the toe transfer can be performed with greater assurance that skin closure can be obtained over hardware, tendons, nerves, and vessels.
providing excess soft-tissue coverage of the amputation stump. This is commonly performed using a pedicle groin flap or free fasciocutaneous flaps (i.e., lateral arm, anterolateral thigh flaps). When the skin has healed and edema resolved (usually 2 or 3 months after skin flap procedure), the toe transfer can be performed with greater assurance that skin closure can be obtained over hardware, tendons, nerves, and vessels.
PREOPERATIVE PREPARATION
General
The great toe flap results in perhaps the most visibly deforming appearance after harvest than any other free flap (Fig. 35-2). It also provides the opportunity for the most dramatic elevation in overall function than any other free flap (3). A well-informed and carefully deliberated decision requires significant effort by both the patient and surgeon. It is for this reason that “acute toe transfer” surgeries are rarely performed. Some authors, however, have shown that early reconstruction may be associated with reduced convalescent time and better sensory recovery (12,13).
The experienced toe transfer surgeon should have available a portfolio of images of preoperative and postoperative results of similar cases for the prospective patient to examine. We have also found many previous toe transfer recipients to be willing resources for prospective toe transfer patients to contact and discuss function, donor site issues, and the reconstructive/recovery experience. It is also helpful to have patients evaluated by a prosthetist so they may have a complete understanding of all options available to them.
Recipient Site
Closure of the amputation stump is achieved with preservation of as much soft tissue as possible (even if it appears grossly excessive) in anticipation of possible toe transfer reconstruction. If there is insufficient soft tissue at the recipient site, it should be supplemented. The pedicled groin flap is a reliable and rapid means of augmenting the amputation site without requiring dissection of sites for future microanastomoses (i.e., the radial artery in the snuffbox) (Fig. 35-3). The groin flap donor site provides generous amounts of supple skin, and the donor site scar is easy to conceal. Alternatively, free fasciocutaneous or fascia flap transfer can be considered. In this setting, we make an effort to perform the anastomosis to the radial artery at the distal volar forearm in an end-to-side fashion. The subsequent toe transfer can then be perfused by anastomosis “downstream” in an end-to-side anastomosis in the radial artery in the snuffbox.
Donor Site
The donor foot should demonstrate palpable pulses to safely proceed with toe transfer surgery. Lack of palpable pulses suggests a significant risk of flap loss or foot ischemia after harvest. Preoperative angiography is not routinely performed at this institution. While the “dominant” blood vessel to the great toe may be plantar or dorsal in the first web space, this may be determined intraoperatively and would not alter preoperative planning to warrant routine angiographic assessment of patients with palpable pedal pulses.
The donor side is selected by comparing the appearance of the right and left great toe and the uninjured thumb. Either toe is selected if the size or morphology of the toe or nail complex is thought to be superior for creation of the new thumb compared to the opposite toe. If they are equivalent, we prefer to harvest the left great toe solely because of the need for the great toe in activating the accelerator while driving an automobile. Alternatively, if the patient has a strong side preference, this should be taken into consideration.
Whether the donor vessel drapes radially or ulnarly from the reconstructed thumb does not pose a significant challenge in insetting the toe and should not influence harvest side selection.
TECHNIQUE
This procedure is most efficiently achieved with a two-team approach, so that great toe harvest can be approaching completion by the time the hand preparation is complete. The supine patient should be positioned such that the heel of the donor foot is at the edge of the operative table. This facilitates dissection of the plantar surface of the foot. Tourniquets are used on both the upper and lower extremities.
Preparation of the hand
A sweeping incision is made from the volar to dorsal aspect of the thumb metacarpal stump, elevating radial and ulnar skin flaps. The flaps are thinned of excess subcutaneous fat if needed. This configuration will accommodate the triangular plantar and dorsal skin segments provided by the toe flap, while providing needed coverage on the radial and ulnar aspects of the toe. Dorsally, the incision is extended proximally enough to provide access to the EPL stump, the radial artery in the snuffbox, and the cephalic vein. Volarly, the incision is extended proximally enough to access the digital nerves proximal to scar tissue or neuroma. If this is proximal to the MCP flexion crease, the incision is altered in a zigzag fashion to avoid a postoperative scar flexion contracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree