CHAPTER 40 Glenohumeral stiffness and arthritis after instability surgery—causes and treatment
 Glenohumeral stiffness and arthritis can be a significant problem after instability surgery and usually affects younger patients.
Glenohumeral stiffness and arthritis can be a significant problem after instability surgery and usually affects younger patients.Clinical history, physical examination, and radiographic evaluation
Physical examination
Palpation of certain key areas of the shoulder should be done. The neck also should be evaluated because shoulder pain may either be caused by cervical disease or may refer pain to the neck. Limited shoulder motion also can cause ipsilateral neck pain, tightness, and spasm as a result of strain in the compensatory periscapular muscles.
Radiographic findings
Samilson et al1 originally described the radiographic appearance of arthritic glenohumeral joints after dislocation. Dislocation arthropathy is based on changes seen on the AP radiograph and classified into three groups based on the combined measurement of inferior osteophytes on both humerus and glenoid. Grade I (mild) arthritis measures less than 3 mm (Fig. 40-1, A), and grade II (moderate) arthritis measures between 3 and 7 mm with evidence of glenohumeral joint irregularity (Fig. 40-1, B). Grade III (severe) arthritis is greater than 7 mm with joint space narrowing and sclerosis (Fig. 40-1, C).
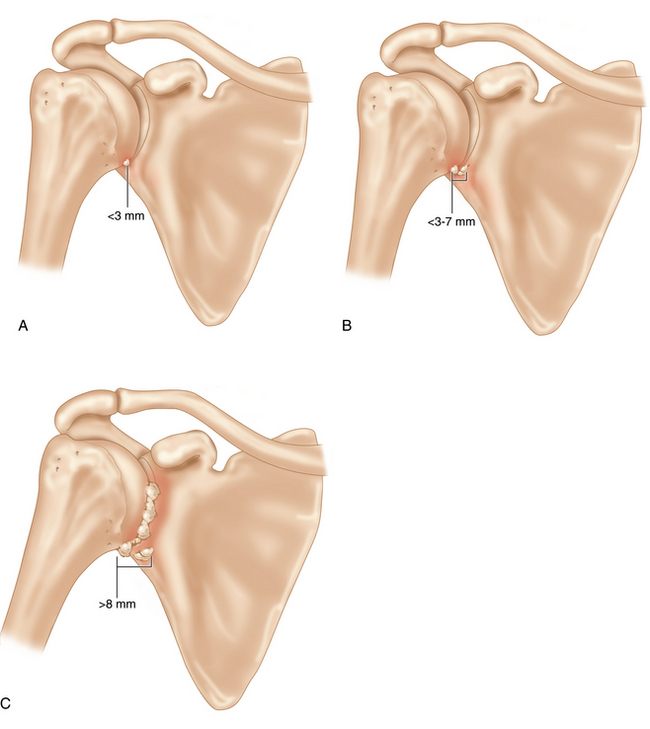
FIGURE 40-1 Samilson et al classification1 for dislocation arthropathy. The classification is based on the combined size of humeral and glenoid osteophytes as seen on an anteroposterior (AP) radiograph. Grade 1 (mild, A) is <3 mm in combined measurement, grade 2 (moderate B) is 3 to 7 mm, and grade 3 (severe, C) is >8 mm.
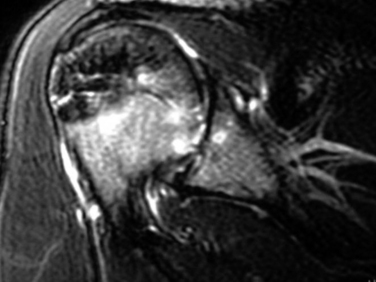
Advanced imaging is an important adjunct in the radiographic evaluation of the postsurgical arthritic and/or stiff shoulder. Magnetic resonance imaging (MRI) can be helpful in evaluating articular cartilage, labrum, rotator cuff, and other soft tissue pathology. Computed tomography (CT) scanning is extremely useful for identifying joint incongruities, loose bodies, and bone abnormalities. Although more invasive by nature, the addition of intra-articular contrast to either MRI or CT imaging potentially adds invaluable information when investigating etiologies for postsurgical stiff shoulders.
Stiffness without glenohumeral arthritis
Chondrolysis
Chondrolysis is a rare but catastrophic complication of arthroscopic shoulder instability surgery (Fig. 40-2). Multiple cases in the literature have been reported, but open surgical stabilization has not been associated with chondrolysis. Hence, there has been much speculation regarding the etiology of chondrolysis as a postarthroscopic phenomenon.
Most commonly, chondrolysis has been associated with radiofrequency devices. Thermal capsulorrhaphy has had some use in the past to treat capsular laxity. Good et al2 reported that eight patients developed chondrolysis after thermal energy was used. All eight had either thermal capsulorrhaphy or thermal capsular shrinkage in conjunction with labral repair for instability.
Stiffness with glenohumeral arthritis
Arthritis after instability episodes
Hovelius et al3 retrospectively evaluated long-term results after the open surgical Bristow-Latarjet procedure. Thirteen percent of patients who had a history of recurrent dislocation developed Samilson grade 2 or 3 arthritis, while only 6% without a history of recurrent dislocation demonstrated Samilson grade 2 or 3 arthritis.
Arthritis after instability surgery
Multiple studies have demonstrated differing incidences of arthritis following instability surgery, especially with open surgical techniques. Neer et al4 reported that 7% of total shoulder arthroplasties were performed on patients with prior instability surgeries, and the average age was significantly younger in those patients. Rosenberg et al5 evaluated patients at 15 years following open Bankart repair, and 12% showed evidence of moderate to severe osteoarthritis. Other studies have demonstrated that anywhere from 12% to 17% of patients developed Samilson grade 2 to 3 arthritis after Bankart repair. In other soft tissue operations, a number of studies with follow-up from 9 to 26 years have demonstrated 11% to 30% incidence of moderate to severe arthritis after Putti-Platt capsulorrhaphy.
Procedures that address bone defects also have been associated with the variable development of arthritis. Bristow-Latarjet coracoid transfer procedures have demonstrated successful clinical outcomes. Banas et al6 reported that, at an average of 8.6-year follow-up, only 3% developed mild to moderate arthritis. In a long-term cohort, Hovelius et al3 found 14% with Samilson grade 2 to 3 changes at a mean 15-year follow-up. Similarly, Brox et al7 reported on 52 patients who underwent autograft iliac crest glenoid reconstruction with average follow-up of 14 years. Of those 4% had recurrence of instability and 53% of operated shoulders developed mild to moderate arthrosis.
There have been reports of complications from implants used for instability surgery. Zuckerman et al8 reported on 37 patients who developed complications after instability repair with screws or staples. Fourteen patients (41%) were noted to have significant injury to the articular cartilage at the time of reoperation. Obviously poor placement of metal, screws, pins, wires, and staples or even bioabsorbable material can damage the articular surface and lead to arthritic changes. However, even well-placed implants can cause a reaction leading to degeneration of the joint. Glenohumeral arthritis has been associated with increased use of certain bioabsorbable anchors. Freehill et al9 reported that 19% of patients developed delayed onset of synovitis including pain and progressive stiffness after use of poly-L-lactic acid tack at an average of 8 months after surgery.