Genitourinary System
Kevin B. Gebke M.D
Perspective
The genitourinary (GU) system comprises of the internal and external organs that make up the urinary system (kidney, ureter, urinary bladder, and urethra) and the genital organs. Both systems are located in the lower abdomen and pelvic area. Injuries to the kidney, ureter, and bladder are common in athletics. The most common symptom reported in GU system injuries is hematuria.
Anatomy
For the most part, the organs of both the genital and urinary systems are well protected. The kidneys are located in the retroperitoneal upper lumbar area of the abdomen, with the upper third of the right kidney and the upper half of the left kidney located underneath the 12th rib. The psoas, paravertebral, and latissimus dorsi muscles protect the remaining parts of the kidneys. The kidneys themselves rest in a bed of pericapsular fat.
The ureters run their course along the posterior peritoneal wall and are primarily protected by the vertebrae and muscles of the posterior abdominal wall. The ureters are vulnerable only where they course over the pelvic rim and into the bladder. The bladder lies within the pelvis except when it is full and rises above the pelvic rim. The bladder is thinnest and most vulnerable when full. The entire female reproductive system is situated within the pelvis, as are the prostate and internal portion of the male urethra. The external male genitalia (penis, scrotum, and testes) are obviously the most vulnerable portions of the male GU system. During sports, these organs are protected and held close to the body by an athletic supporter.
Kidney Injuries
Injury to the kidney can result from direct trauma, repetitive jarring, decreased renal blood flow, and medication side effects.
Traumatic Injuries
The kidney can be injured by a direct blow to the exposed flank area or abdomen, such as when a football player reaches up to catch a pass and is tackled. The kidney also is subject to a contrecoup type of injury after a high-speed collision. The following kidney injuries are common in sports: contusion, intra- and extracapsular injury, capsular tear or rupture, renal parenchymal tear or rupture, and tear of the renal pedicle.
Injury to the kidney is typically accompanied by pain, tenderness, ecchymosis and/or hematuria. In rare instances, renal colic can occur from blockage of the renal pelvis by blood clots. Hypovolemic shock may be a result of extensive bleeding. There is a weak correlation between the degree of hematuria and the degree of kidney injury. Occasionally, there will be no blood in the urine if the renal collecting system is spared. An indication of significant bleeding is the loss of renal outline and psoas muscle shadow on plain kidney, ureter, and bladder (KUB) films of the abdomen (Figure 16.1). Associated rib fractures, renal capsular and renal cortex tears, or bleeding may be detected on plain x-rays or intravenous pyelogram (IVP).
If an athlete has flank pain following an injury but the urinalysis is normal, successive urine studies should be done to ensure that the urine remains clear. If the team physician doubts the presence of a kidney injury and the urinalysis and plain films of the abdomen are negative, further diagnostic tests are unnecessary and observation is all that is required to manage this situation. If an injury
to a kidney is strongly suspected, an IVP or computed tomography (CT) with intravenous contrast should be obtained. CT has emerged as the preferred diagnostic test; Definitive diagnosis can be established and associated abdominal and retroperitoneal injuries are easily identified.
to a kidney is strongly suspected, an IVP or computed tomography (CT) with intravenous contrast should be obtained. CT has emerged as the preferred diagnostic test; Definitive diagnosis can be established and associated abdominal and retroperitoneal injuries are easily identified.
 Figure 16.1 Kidney, ureter, and bladder (KUB) demonstrating normal psoas muscle shadow and renal outline. |
The incidence of renal trauma in sports is unknown. Kidneys that are large, malformed, or have tumors are more prone to injury. There are five classes of injury as follows:
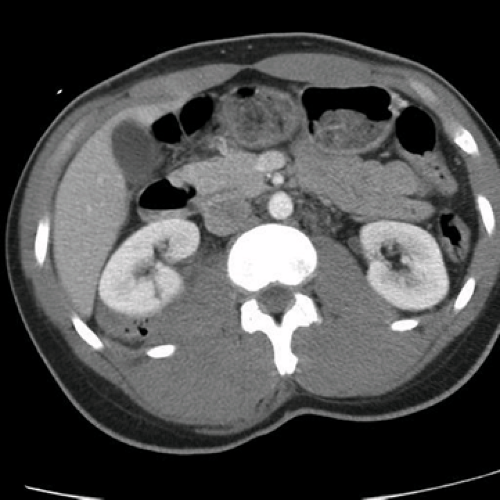
Class I—contusion. These represent most (>85%) sports-related injuries to the kidney (1). There is usually a history of trauma but signs of trauma may or may not be present. Hematuria is usually present and the IVP is negative. CT (Figure 16.2) will identify the renal contusion (1), but most class I injuries do not require such extensive evaluation. Treatment of most contusions initially involves observation, hydration, bed rest, and repeat urinalysis. Most athletes return to sports after approximately 2 to 3 weeks of rest.
Class II—cortical laceration. Cortical laceration is usually related to trauma and has findings similar to a contusion. On a plain radiograph, the psoas shadow may be lost and an IVP will show extravasations of dye. CT may be useful to identify the degree of injury. Again, observation, hydration, bed rest, and a repeat urinalysis are indicated. As with class I injuries, most athletes return to play within 2 to 3 weeks.
Class III—caliceal laceration. Caliceal laceration involves intrarenal hemorrhage and disruption of the caliceal collecting system. CT establishes diagnosis, and repeat scanning is recommended to establish stabilization of the injury and healing (Figure 16.3). IVP, if utilized, will show an intact capsule with intrarenal extravasation of dye and loss of definition of the calices. Treatment involves observation and surgery for more serious cases.
Class IV—complete renal fracture. This is a rare sports injury and the patient usually presents in shock. CT or IVP can establish diagnosis if the athlete is stable. Immediate surgery is indicated.
Class V—vascular pedicle injury. This injury is also rare in sports and the patient presents in hypovolemic shock. Hematuria may or may not be present and the kidneys are usually not visualized on IVP. Visualization of the renal pedicle is possible with CT. A selective renal arteriogram shows renal vascular damage. Treatment always involves surgery, usually emergently.
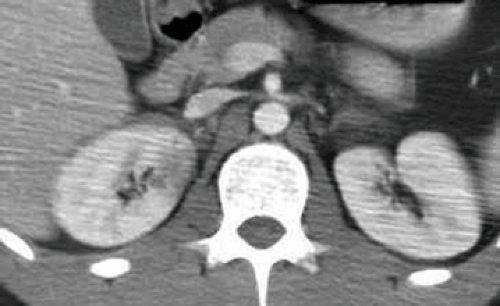 Figure 16.2 Computed tomography (CT) of the abdomen demonstrating a right renal contusion (without laceration). |
Most kidney trauma results in intracapsular or contusion injuries and heals without sequelae or complications. The athlete should be at complete bed rest until the urine is completely free of hematuria. Any athlete who develops hematuria after a blow to the flank or abdomen should be monitored closely. Extracapsular kidney injuries respond well to bed rest and close follow-up by the team physician in 50% of cases. The other 50% of cases may have continued bleeding (2). If diagnostic testing shows a nonfunctioning kidney or major injury with extracapsular extravasation, prompt referral is indicated. Referral to a urologist and appropriate treatment, including bed rest and/or surgery, is preferable in managing this situation.
The examining physician should check for injury to other intra-abdominal organs whenever a serious kidney injury is suspected. The athlete should not exercise further and hospital transport should be expedited. Surgery is usually indicated for pedicle tears, kidney lacerations, and massive hemorrhage of the kidney. It should be noted that there is a risk for rebleed following major renal vascular surgery. The occurrence rate is approximately 15% and is typically seen 15 to 20 days postoperatively, corresponding with clot resolution. Also, postinjury hypertension has been described at various rates of occurrence.
Prevention of severe kidney injuries should be considered in collision sports. Hip pads do not generally extend high enough to protect the kidneys, but kidney pads can be hung by straps from the shoulders. The use of a flak jacket also provides excellent kidney protection in most cases. Proper coaching techniques and adherence to regulations about protective equipment can reduce the incidence of severe kidney injuries.
Kidney Injuries from Prolonged Heavy Exercise
Renal function is affected by prolonged exercise. Renal blood flow decreases in response to exercise as blood is shunted to exercising muscles (3,4). Renal blood flow decreases more in exercising dehydrated or hypovolemic patients, but will generally return to pre-exercise levels within approximately 60 minutes. The mechanism for decreased renal blood flow is related to sympathetic nervous system–induced constriction of afferent and efferent arteries and increased levels of epinephrine and norepinephrine. Dramatic decreases in renal blood flow up to 50% may result in ischemia of the kidney and hematuria.
The following changes in renal physiology have been observed during exercise: (1) a drop in renal blood flow is proportionate to the severity of the exercise performed; (2) glomerular filtration rate (GFR) is usually well maintained but may decrease; (3) free water clearance decreases during even short exercise periods in well-hydrated subjects; (4) transient proteinuria may develop; (5) significant reduction in sodium excretion is observed because of increased tubular reabsorption; (6) antidiuretic hormone (ADH) may increase threefold with heavy exercise, and urinary water excretion is usually decreased as there is a decrease in urine flow during exercise, and (7) an increased excretion of white blood cells (WBCs) and red blood cells (RBCs) in addition to increased urinary excretion of casts (hyaline and granular) occurs.
These renal changes are transient and disappear after exercise. For the most part, renal function typically normalizes within 10 to 36 hours. Damage to renal parenchyma does not occur during heavy exercise. All renal changes noted in the preceding text are attributed to constriction of the renal vasculature. It has been postulated that an increase in core body temperature will increase permeability and also lead to some of the renal changes noted during exercise.
Acute renal failure (ARF) may be seen with renal ischemia during heat injury or severe dehydration. Severe muscle damage will produce myoglobinemia. The physician should be aware that nephrotoxins are usually excreted in this situation. Treatment of ARF should follow normal guidelines for this diagnosis. Prevention of this problem is related to proper hydration of the athlete before and during competition and exercise activities.
Injury to the Ureter and Bladder
Ureters
Injury to the ureter is commonly associated with severe renal damage. Fractures of the pelvis and lower lumbar vertebrae should be considered when assessing this type of injury. IVP is useful in diagnosis. Traumatic injuries to the ureter are rare and should be referred to a urologist.
Bladder
An empty bladder is rarely damaged by trauma. Traumatic bladder injuries do occur in the martial arts. The most common type of bladder injury is a contusion. Complete rupture of the bladder is rare. Most bladder injuries are related to blunt trauma on a distended bladder. Bladder trauma is present in 10% to 15% of patients with a fractured pelvis (5). Repetitive jarring of the bladder in long-distance racing may cause transient bladder contusions. The patient presents with a history of trauma, suprapubic pain, and guarding. Diagnostic evaluation should include a cystogram with a postdrainage film. Athletes with bladder trauma can pass small blood clots and often report dysuria and hematuria.
Two types of bladder injury are common. The first is a contusion where the degree of hematuria does not correlate well with the severity of the injury. Patients with a contusion are treated with bed rest and observation. Severe contusions require the use of an indwelling catheter for 7 to 10 days and antibiotic treatment. The second type of injury involves a bladder rupture, which can be intra- or extraperitoneal, or a combination of both. These injuries
are usually associated with a pelvic fracture and require immediate surgery.
are usually associated with a pelvic fracture and require immediate surgery.
The urologist should dictate treatment. Follow-up with frequent urinalysis examinations will be necessary. The athlete may return to competition when symptom free and all evidence of hematuria has cleared. Prevention of most bladder injuries is accomplished by having the athlete completely empty the bladder before competition.
Biker’s Bladder
A possible complication of aggressive bicycling is the development of “biker’s bladder” (detrusor muscle irritability). The athlete usually has an abrupt onset of urinary frequency, diminished urinary stream, nocturia, and terminal dribbling. This symptom complex is similar to that described secondary to prostate irritation from prolonged cycling. These problems may be avoided by frequently and properly emptying the bladder during long bicycle rides. Once symptomatic, athletes will usually respond favorably to rest from the offending activity. Some cases will require urologic referral.
Urethral Injuries
Injuries to the anterior urethra can be seen in athletes. The injury is typically sustained when an athlete falls into a straddle position on a hard object or suffers a direct blow to the perineum. This injury can predispose to future urethral stricture secondary to scarring. Diagnosis is established by history and physical examination findings (blood at the urethral meatus, perineal or penile hematoma). The diagnosis should be confirmed by retrograde urethrogram. Partial injuries can be treated conservatively with urethral cauterization and/or stenting. More severe injuries require surgical repair. Posterior urethral injuries are rarely seen and are usually associated with severe trauma and pelvic fracture. Urologic evaluation is recommended for most urethral injuries.
Urinary Incontinence
Stress incontinence has an unknown relation to exercise. Athletes may notice symptoms sooner than their nonathletic peers (6). Treatment is the same in athletes as it is in nonathletes. Referral to a urologist or gynecologist may be required for female athletes to treat severe cases of urinary incontinence that interfere with daily activities and exercise.
Hematuria
Hematuria is the most common urinary symptom seen after vigorous athletic activity (6). Distance swimmers and runners usually have the greatest incidence of exercise-induced hematuria, although it has been commonly reported in lacrosse, running, football, and rowing athletes. Most studies in the literature report clearing of hematuria within 48 hours after vigorous exercise (7,8,9,10,11,12,13,14). Direct kidney injury, renal vein kinking, bladder contusion, or preexisting renal pathology may also cause hematuria. The problem for the team physician is to distinguish significant organic disease from transient, benign conditions that cause hematuria.
Gardner (15) was the first to use the term athletic pseudonephritis when he described hematuria and proteinuria in 45% of football players examined. Microscopic hematuria is very common in the general population. In a population-based study at the Mayo clinic, 13% of men and postmenopausal women had asymptomatic microscopic hematuria (16). A study at Kaiser Medical Center, Honolulu, on patients undergoing multiphasic screening revealed a 15% incidence of microhematuria (11). Microscopic hematuria is also common in younger patients. In a survey of 8,954 Finnish school children, microscopic hematuria was found in one or more specimens in 4% of the children (14). The lower urinary tract is regarded as the most common source of hematuria after prolonged and exhaustive exertion. The existence of renal stones, urinary tract infection, or exercise-induced irritation of the urethral meatus from contusion or cold exposure should be eliminated in the differential diagnosis of hematuria.
No consensus exists on the upper limit of normal for urinary RBC. Urinary RBC count may rise after events such as mild trauma, exercise, or sex (17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree