Chapter 167 Gallstones
 General Considerations
General Considerations
Gallstones are another example of a “Western diet”–induced disease. In the United States, autopsy studies have shown that gallstones exist in approximately 20% of women and 8% of men older than age 40. Conservative estimates suggest that about 20 million Americans (10% of the U.S. population) and 5% to 22% of the population in the Western world have gallstones.1 Each year 1 million more develop gallstones. More than 300,000 gallbladders are removed each year in the United States owing to the presence of gallstones.2–5 Gallstones are also considered a significant risk factor for gallbladder cancer.6,7
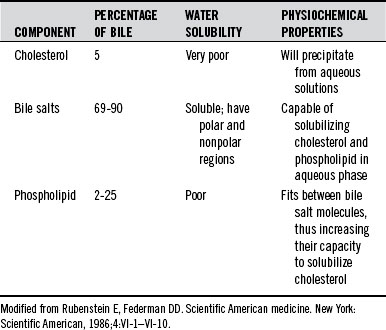
The bile components include bile salts, bilirubin, cholesterol, phospholipids, fatty acids, water, electrolytes, and other organic and inorganic substances.8 Table 167-1 shows the characteristics of the major bile components. Gallstones arise when a normally solubilized component of bile becomes supersaturated and precipitates. Gallstones can be divided into four major categories:
• Pure pigment (calcium bilirubinate)
• Mixed—containing cholesterol and its derivatives along with varying amounts of bile salts, bile pigments, and inorganic salts of calcium
Pure stones, either cholesterol or calcium bilirubinate, are extremely rare in the United States, where recent studies indicate that approximately 80% of the stones are of the mixed variety. The remaining 20% of the stones are composed entirely of minerals, principally calcium salts, although some stones contain oxides of silicon and aluminum.2–4
 Pathogenesis
Pathogenesis
The formation of gallstones has been divided into three steps:
Cholesterol and Mixed Stones
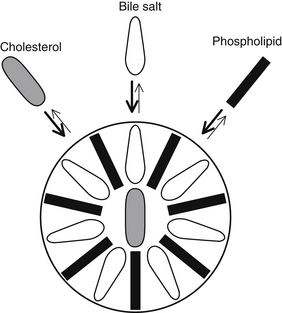
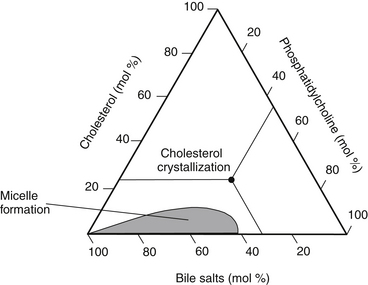
The requisite step in cholesterol and mixed stone formation is cholesterol supersaturation of bile within the gallbladder. Bile solubility, as well as bile supersaturation, is based on the relative molar concentrations of cholesterol, bile acids, phosphatidylcholine (lecithin), and water. Because free cholesterol is water insoluble, it must be incorporated into a lecithin-bile salt micelle (Figure 167-1). Using triangular coordinates, it is possible to demonstrate the solubility of cholesterol in bile (Figure 167-2).
As illustrated in the figures, either an increase in cholesterol secretion or a decrease in bile acid or lecithin secretion will lead the bile to become supersaturated. Once the bile is supersaturated, stone formation is initiated by such factors as biliary stasis, infection, and increased mucin secretion by the gallbladder epithelium. Once the stone begins to form, its radius increases at an average rate of 2.6 mm/year, eventually reaching a size of a few millimeters to more than a centimeter. Symptoms typically occur an average of 8 years after formation begins. Cholelithiasis is present in 95% of patients with cholecystitis.8
Risk Factors for Cholesterol and Mixed Stones
The major risk factors for the development of cholesterol and mixed gallstones include the following2–4:
Genetic and Ethnic
The prevalence of gallstones appears to have some genetic aspects. Gallstones are most common in Native American women over age 30. Nearly 70% of this group have gallstones. In contrast, only 10% of black women over 30 have gallstones. The difference in the prevalence rate between ethnic and genetic groups reflects the extent of cholesterol saturation of the bile. The extent to which dietary factors affect this value probably outweighs genetic factors.9
Obesity
Obese subjects are at risk for developing gallstones both by being overweight and when initially losing weight.10 Obesity causes an increased activity of HMG-CoA reductase with increased secretion of cholesterol in the bile as a result of increased cholesterol synthesis. Therefore, obesity is associated with a significantly increased incidence of gallstones due to biliary cholesterol saturation.
Important to note is that during active weight reduction, changes in body fat and diet can actually promote gallstone problems. During the first stages of weight loss, biliary cholesterol saturation initially increases.4 The secretion of all biliary lipids is reduced during weight loss, but the secretion of bile acids decreases more than that of cholesterol. Once the weight is stabilized, bile acid output returns to normal levels while the cholesterol output remains low. The net effect is a significant reduction in cholesterol saturation. In prescribing diet therapies for obese patients with a high risk of gallstones, it should be recognized that prolonged dietary fat reduction can also promote biliary stasis,1 thus contributing to cholesterol saturation. Studies show that at least 10 g of fat per day is necessary in order to assure proper gallbladder emptying.11
Drugs
Tamoxifen treatment in postmenopausal breast cancer patients greatly increases gallstones. One retrospective cohort study of 703 women demonstrated that after 5 years, the incidence of stone formation in the tamoxifen-treated patients was 37.4%, whereas it was 2% in patients who did not receive tamoxifen.12 Most gallstones became apparent after 3 years.
In addition to oral contraceptives and other estrogens, as discussed earlier, drugs that increase the risk of gallstones include the cephalosporin ceftriaxone, octreotide, HMG-CoA reductase inhibitors,1 and possibly other lipid-lowering drugs.
Age
Gallstones have been reported from fetal age to extreme old age, but the average patient is 40 to 50 years old. Decline in the activity of cholesterol 7-α-hydroxylase with age1 leads to an increase in biliary cholesterol hypersecretion13 and thus cholesterol saturation, with accelerated formation of gallstones.
 Therapeutic Considerations
Therapeutic Considerations
A number of dietary factors are important in the prevention and treatment of gallstones. Foremost is the elimination of foods that can produce symptoms. Also important are increasing dietary fiber, eliminating food allergies, and reducing the intake of refined carbohydrates and animal protein. There is a protective effect of vegetables and fruits against gallbladder cancer, and red meat (beef and mutton) was found to be associated with an increased risk of gallbladder carcinogenesis.14 Because gallstones are a risk factor for gallbladder cancer,6,7,14 appropriate nonlithogenic dietary practices will protect against both cancer and the development of gallstones.
Biliary cholesterol concentration and serum cholesterol levels do not seem to correlate.15 Although some authors have reported an inverse correlation between high-density-lipoprotein cholesterol and bile saturation and a direct correlation between low-density-lipoprotein cholesterol and bile saturation,16,17 more detailed research does not appear to support these correlations.15 There does, however, seem to be an association between increased levels of serum triglycerides and bile saturation.18
Asymptomatic Gallstones
The natural history of silent or asymptomatic gallstones supports the contention that elective cholecystectomy is not warranted. Although there is a cumulative chance of developing symptoms—10% at 5 years, 15% at 10 years, and 18% at 15 years—a patient should never experience discomfort if controllable risk factors are eliminated or reduced.3
Diet
Dietary Fiber
The hypothesis that the main cause of gallstones is the consumption of fiber-depleted refined foods has considerable research support.4,5 As mentioned earlier, in population studies, gallstones are associated with the Western diet. Such a diet, high in refined carbohydrates and fat and low in fiber, leads to a reduction in the synthesis of bile acids by the liver and a lower bile acid concentration in the gallbladder.
Another way in which fiber may prevent gallstone formation is by reducing the absorption of deoxycholic acid.4,5 This compound is produced from bile acids by bacteria in the intestine. Deoxycholic acid greatly lessens the solubility of cholesterol in bile.
Dietary fiber has been shown both to decrease the formation of deoxycholic acid and to bind deoxycholic acid and promote its excretion in the feces. This greatly increases the solubility of cholesterol in the bile. A diet high in fiber, especially those fibers capable of binding to deoxycholic acid (i.e., predominantly the water-soluble fibers found in vegetables and fruits, pectin, oat bran, and guar gum), is extremely important in both the prevention and reversal of most gallstones.5
Interestingly, diets rich in legumes with high concentrations of water-soluble fibers are associated with an increased risk for gallstones.9 Chileans, Pima Indians, and other North American Indians have the highest prevalence rates for cholesterol gallstones, and all consume a diet rich in legumes. Evidently, legume intake increases biliary cholesterol saturation as a result of legumes’ saponin content.9 A study conducted in The Netherlands showed just the opposite, because legume intake was shown to offer significant protection against gallstones.62 Until this issue is clarified, it might be best to restrict legume intake in individuals with existing gallstones.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree