Gait Analysis
Paul Tortland
A well-known physical therapist once said, “When the foot hits the ground, the mud hits the fan.” His point was that there are inextricable links between foot mechanics, gait, and human performance. Volumes have been written about gait analysis, and a complete discussion of this topic is beyond the scope and purpose of this chapter. Rather, the goal here is to discuss functional foot and gait mechanics and the influence on—and by—the spine within an osteopathic framework.
To understand how gait disturbances can play a role in sports injuries (and how more proximal injuries can affect gait mechanics), one must first have a basic understanding of the gait cycle and normal gait mechanics.
THE GAIT CYCLE AND NORMAL MECHANICS
The Gait Cycle
The gait cycle is routinely divided into two phases, swing and stance. Alternatively, gait may be divided into single-support and doublesupport phases. The gait cycle is defined as the processes that occur between two successive occurrences of one of the repetitive events of walking (1). The start of the gait cycle is generally accepted as beginning with heel strike, which initiates the stance or initial doublesupport phase. The swing phase begins with toe-off of the same limb, and ends with heel strike, thus completing one cycle. This is illustrated in Figure 25.1 (2).
In normal walking 60% of the gait cycle encompasses the stance phase, and 40% is the swing phase. Ten percent of the gait cycle consists of double support, that portion between heel contact of one limb and toe-off of the opposite limb when both limbs are in full contact with the ground. This ratio, however, can be dramatically altered depending on the speed of walking or running. In fact, the disappearance of double support marks the transition from walking to running (1).
Foot Mechanics
The key joints of the foot related to gait are the talocrural joint (tibia-fibula-talar dome articulation), the subtalar joint, the midtarsal joints, and the metatarsophalangeal (MTP) joints.
Dananberg has described three “rocker” mechanisms that occur in sequence in the foot during the gait cycle (3). The first is the rounded bottom of the calcaneus that “pivots” during and through heel strike. The second is the dorsiflexion that occurs at the talocrural joint, described subsequently (3). The third is the extension that occurs at the MTP joints.
During gait, the talocrural joint must allow for 10 degrees of dorsiflexion from the point of full ground contact in midstance in order for the body’s center of gravity to pass forward normally. The talar dome is wider posteriorly than anteriorly. As the joint moves into dorsiflexion, the fibula moves laterally and proximally to allow the mortise joint to widen to accommodate the wider posterior portion of the talus. At the same time, the distal tibia-fibula syndesmosis stores energy, preparing for the ensuing plantarflexion.
The subtalar joint (the articulation between the talus and the calcaneus) may be viewed as a type of differential gear, capable of converting limb rotation into pronation and supination (3). During heel strike, the tibia, femur, and
pelvis are rotating internally. Under this load the subtalar joint pronates.
pelvis are rotating internally. Under this load the subtalar joint pronates.
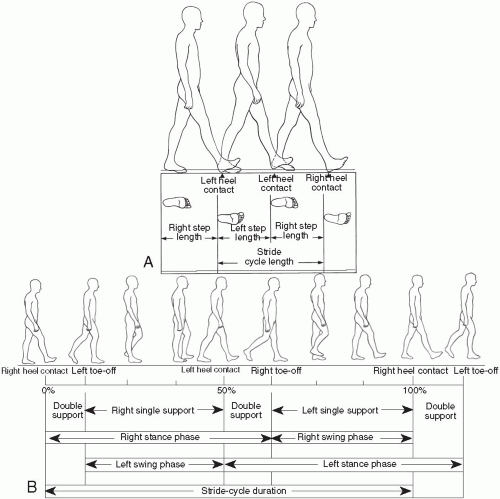 FIGURE 25.1. The gait cycle. (From Shumway-Cook A, Woollacott MH. Control of normal mobility. In: Motor control. Baltimore: Williams & Wilkins, 1996). |
Much ado is made in the clinical and popular recreational sports literature about pronation. Pronation is a combination of talar eversion, forefoot abduction and dorsiflexion, along with flattening of the medial, anterior, and lateral arches. It is a normal occurrence that begins after heel strike and ends just before midstance, comprising no more than 25% of the gait cycle (4). Pronation ends once the leg and foot begin to externally rotate in preparation for toe-off. Pronation is necessary to transform the relatively flexible and accommodating foot into a more rigid platform from which to push off.
Likewise, supination is a normal mechanical event that begins at midstance. The limb that was rotating internally at heel strike begins to rotate externally as the opposite limb pulls forward and rotates the pelvis. The subtalar joint therefore moves into supination (a combination of talar inversion, forefoot adduction, and plantarflexion) to facilitate this transition.
The midtarsal joints act as a mechanical link between the ankle-subtalar complex and the metatarsophalangeal joints. They also act as termination points for most of the extrinsic and intrinsic muscles acting on the foot and ankle. Finally, they act as close-packing mechanical links when loads are applied, facilitating the transition of the foot from a flexible accommodating structure to a rigid propulsive structure, as will be seen later in the chapter.
Finally the MTP joints form the third and final pivot point of the normal rocker motion of the foot during gait.
The first MTP joint is the most important component of this final pivot. The plantar fascia has its strongest distal attachment (50% of its entire thickness) at the base of the proximal first phalanx. Also the motion of the first MTP joint is critical for normal gait to occur. The normal total available range of motion at the joint is 65 degrees. This amount of motion is necessary to account for normal movement of the torso and leg. As the body’s center of gravity passes through midstance, the hip extends 20 degrees. At heel lift, the ankle plantarflexes 20 degrees and the knee flexes 45 degrees. The first MTP joint must flex accordingly to accommodate these movements and allow the body to pass smoothly through toe-off.
The Role of Muscles
Conventional wisdom maintains that the legs are the motive force in locomotion, bringing the passive torso along for the ride. However, more recent and detailed electromyographic analysis has demonstrated that the muscles of the lower extremity fire predominantly in an eccentric contraction, rather than the concentric contraction one would expect if these muscles were prime movers (5).
Gracovetsky proposed the theory of the spinal engine to describe the central role of the spine in the gait process. Essentially, the spine initiates gait by generating pelvic rotation. Accordingly, the lower extremity follows in a pendulum manner, and the muscles of the leg generally fire eccentrically, acting as a “brake” to slow down the limb movement and to generate stability. At heel strike, forces are transmitted up through the leg into the knee, hip, sacroiliac joint, and spine. The entire process is a carefully orchestrated pattern of movements involving the muscles, joints, and myofascial elements of the spine, pelvis, and lower extremity (6).
GAIT DYSFUNCTION
The average adult completes 2,500 stance-swing cycles per limb per day, assuming an average of only 80 minutes per day of weight-bearing activity. This equates to approximately 1,000,000 steps per year for each limb. These numbers can go significantly higher in athletic populations, especially in sports involving running, where the actual amount can double or even triple (7). Any perturbations in normal gait mechanics may result in cumulative adverse structural and performance compensations.
Pes Planovalgus
Much ado is made about “overpronation” and flat feet as a cause of gait disruption (Fig. 25.2). Pronation is a normal and even necessary event in proper gait mechanics. Nonetheless, excessive pronation can be problematic. Abnormal pronation continues past midstance through toe-off.
One of the major effects of pes planovalgus is that it alters the normal timing of events in the gait sequence by retarding the return of the foot
to supination to enable toe-off. The altered timing changes the forces acting on the proximal joints. Altered forces can strain the sacroiliac and lumbosacral joints, leading potentially to instability and abnormal thickening of the inguinal ligament (4). At the knee it can create a valgus stress.
to supination to enable toe-off. The altered timing changes the forces acting on the proximal joints. Altered forces can strain the sacroiliac and lumbosacral joints, leading potentially to instability and abnormal thickening of the inguinal ligament (4). At the knee it can create a valgus stress.
 FIGURE 25.2. Pes planus, or flat feet.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




