CHAPTER 44 Future Directions in Shoulder Arthroplasty
Shoulder arthroplasty has advanced immeasurably since the first shoulder replacement was implanted by Péan in 1893.1 Implant designs continue to evolve and improve, as do the materials from which these designs are constructed. The reverse prosthesis has gained widespread use in the United States since 2004 and continues to evolve, with minor design changes introduced by many companies that manufacture a version of this semiconstrained device.
Our personal interest in the future of shoulder arthroplasty has focused largely on computer-assisted navigation.2,3 Computer-assisted navigation has been used successfully to improve implant alignment in hip and knee arthroplasty.4,5 We have used similar technology involving an image-free system to monitor and improve implant alignment during shoulder arthroplasty.
PREOPERATIVE PLANNING FOR NAVIGATION IN UNCONSTRAINED SHOULDER ARTHROPLASTY
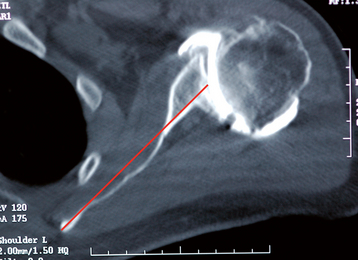
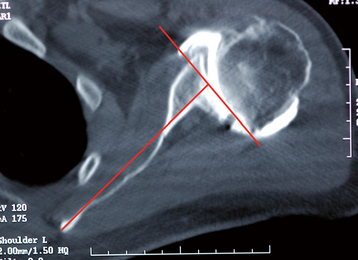
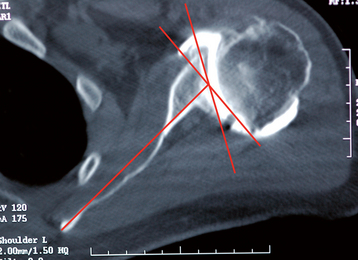
The angle of glenoid version is determined relative to the long axis of the scapula from an axial computed tomogram.6 The plane of section needed for this measurement is located in approximately the middle of the glenoid cavity and is estimated by using the first section inferior to the tip of the coracoid process. The long axis of the scapula is determined by taking the center point of the anteroposterior diameter of the glenoid and constructing a line from this point to the medial aspect of the scapula (Fig. 44-1). A reference neutral axis (0-degree version) is drawn perpendicular to the long axis of the scapula (Fig. 44-2). A line is drawn tangential to the anterior and posterior rims of the glenoid cavity (Fig. 44-3). The acute angle formed by these two lines is the angle of glenoid version (Fig. 44-4). Once version is measured, the amount of correction may be determined. Normal glenoid version ranges from 2 degrees of anteversion to 9 degrees of retroversion.6 For the example in Figures 44-1 to 44-4, the retroversion measures 23 degrees.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree