1
Fundamentals
Hand Therapy Concepts and Treatment Techniques
Hands are visible, expressive, and vulnerable. When clients use their hands to get dressed, eat, touch, gesture, or communicate, they are performing exquisite and complex movements. Limitations of motion or even a small scar can affect a person’s life in profound ways.1 When we touch our clients’ hands, we touch their lives. Although it is very important to be knowledgeable about the details of hand anatomy and to be structure specific in our treatment, it is equally important not to lose sight of the whole person whose extremity we are treating. We must continuously encourage clients to tell us about themselves and their needs so that their therapy can be relevant and successful. While getting to know the person we are treating, we can explain how our interventions and the client’s home programs will be helpful. As a rule, I find that if I listen well, clients frequently tell me in lay terms or even show me exactly what motion or function is missing. The challenge is to identify and treat clients’ specific tissues effectively while not losing sight of them as people.
Hand Therapy Concepts
Timelines and Healing
Tissues heal in predictable phases. However, the length of these phases varies depending on client variables, such as age and health. The three phases of healing are inflammation, fibroplasia, and maturation (also called remodeling). In the inflammation phase, vasoconstriction occurs, followed by vasodilation, with migration of white blood cells to promote phagocytosis in preparation for further healing. In this stage, which lasts a few days, immobilization often is advised, depending on the specifics of the diagnosis.2 If wound contamination or delayed healing is a factor, this phase can last longer.3
The fibroplasia phase begins about 4 days after injury and lasts 2 to 6 weeks. In this phase, fibroblasts begin the formation of scar tissue. The fibroblasts lay down new collagen, on which capillary buds grow, leading to a gradual increase in the tissue’s tensile strength. In this stage, active range of motion (AROM) and orthotics typically are used to promote balance in the hand and to protect the healing structures.2
The timeline for the maturation (remodeling) phase varies; this phase may even last years. In the maturation phase, the tissue’s architecture changes, reflecting improved organization of the collagen fibers and a further increase in tensile strength. The tissue is more responsive (that is, reorganizes better) if appropriate therapy is started sooner rather than later. In this stage, gentle resistive exercises may be appropriate, and the client should be monitored for any inflammatory responses (also known as a flare response). Dynamic or static orthoses may also be helpful.2
Positioning to Counteract Deforming Forces
Predictable deforming forces act on an injured upper extremity (UE). Edema (swelling) routinely occurs after injury, creating tension on the tissues. The resulting predictable deformity posture is one of wrist flexion, metacarpophalangeal (MP) hyperextension, proximal interphalangeal (PIP) and distal interphalangeal (DIP) flexion, and thumb adduction.4 This deformity position occurs as a result of tension on the extrinsic muscles caused by dorsal edema.
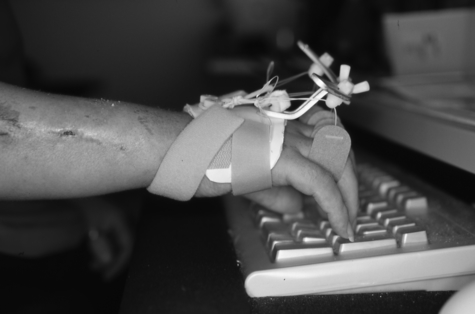
Use of the antideformity (intrinsic-plus) position is recommended after injury unless it is contraindicated by the diagnosis (for example, it is not used after flexor tendon repair). The antideformity position consists of the wrist in neutral position or extension, the MPs in flexion, the IPs in extension (IPs refers to the PIP and DIP joints collectively), and the thumb in abduction with opposition (Fig. 1-1). The antideformity position maintains length in the collateral ligaments, which are vulnerable to shortening, and counteracts deforming forces.
Joint and Musculotendinous Tightness
Joint tightness is confirmed if the passive range of motion (PROM) of a joint does not change despite repositioning of proximal or distal joints. Musculotendinous tightness is confirmed if the PROM of a joint changes with repositioning of adjacent joints that are crossed by that particular muscle-tendon (musculotendinous) unit.5
Joint tightness and musculotendinous tightness can be treated with serial casting, dynamic orthoses static progressive orthoses or serial static orthoses (see Chapter 7 and also the “Orthotics” section later in this chapter). With joint tightness, splinting can focus on the stiff joint, and less consideration is needed for the position of proximal or distal joints. With musculotendinous tightness, because the tightness occurs in a structure that crosses multiple joints, the orthotic must carefully control the position of proximal (and possibly distal) joints to remodel tightness effectively along that musculotendinous unit.
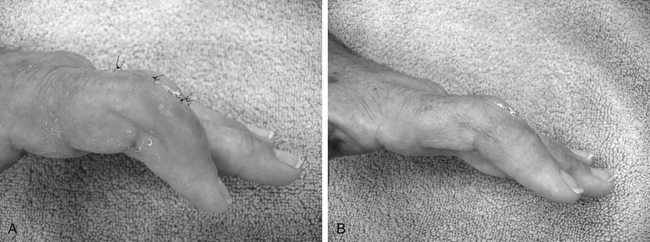
The client in Fig. 1-2, A, had an infected PIP joint in the index finger. He was treated with hospitalization, intravenous administration of antibiotics, and joint debridement. He arrived for therapy 2 weeks later than his physician had ordered; he had no orthotic, significant edema, and a severe flexion contracture of the PIP joint. Because the stiffness was localized to the PIP joint, he needed only a digit-based extension orthosis for that joint. Fig. 1-2, B, shows his progress after 2 weeks of edema control and serial static digit-based orthoses.
Intrinsic or Extrinsic Extensor Muscle Tightness
Intrinsic muscles are the small muscles in the hand. Extrinsic muscles are longer musculotendinous units that originate proximal to the hand. Intrinsic tightness and extrinsic extensor tightness are tested by putting these muscles on stretch. This is accomplished by comparing the PROM of digital PIP and DIP flexion when the MP joint is passively extended and then passively flexed. With interosseous muscle tightness, passive PIP and DIP flexion is limited when the MP joint is passively extended or hyperextended (Fig. 1-3). With extrinsic extensor tightness, PIP and DIP flexion is limited when the MP joint is passively flexed (Fig. 1-4).5

Proximal interphalangeal (PIP) and distal interphalangeal (DIP) flexion is passively limited when the metacarpophalangeal (MP) joint is passively extended or hyperextended.

PIP and DIP flexion is passively limited when the MP joint is passively flexed.
Extrinsic Extensor or Flexor Tightness
Extrinsic tightness can involve the flexors or the extensors. To test for tightness, put the structure on stretch by positioning the proximal joint crossed by that structure. With extrinsic extensor tightness, passive composite digital flexion is more limited with the wrist flexed than with the wrist extended. With extrinsic flexor tightness, passive composite digital extension is more limited with the wrist extended than with the wrist flexed.5
Lag or Contracture
When a lag is present (PROM exceeds AROM), treatment should focus on promoting active movement. Blocking exercises (Fig. 1-5), differential tendon gliding exercises (see Fig. 1-18), place and hold exercises (see Fig. 1-19), and dynamic or static functional orthotics can be helpful (Fig. 1-6). If a contracture is present, promote both PROM and AROM with the same exercises and with corrective orthoses, which may be the dynamic, static progressive, serial static, or casting type.
Joint End-Feel
A joint with a soft end-feel has a spongy quality at the end-range. This is a favorable quality that indicates a potential for remodeling. Orthoses for soft end-feel may be the static type or the low-load, long duration type (see the “Orthotic” section and Chapter 7).
A joint with a hard end-feel has an unyielding quality at end-range. This is a stiffer joint, and correcting it may require serial casting or static progressive orthoses with longer periods of splint wear.2 Documenting the end-feel and explaining the implications of your findings to the client are very important.
Taking Care with Passive Range of Motion
PROM of the hand should be performed gently and with care.
Precaution. PROM can injure swollen and inflamed joints and tissues. Colditz5 cautions that the only joints for which manual PROM is safe are joints with a soft end-feel. Nevertheless, clients may request more aggressive therapy. They may even be passively stressing their swollen, stiff hands at home. It is very important that the therapist inquire about this and put a stop to it. Explain to your client how injurious and counterproductive it is, emphasizing that delicate hand tissues are all too easily injured (see Chapter 12).
Quality of Movement and Dyscoordinate Co-Contraction
Dyscoordinate co-contraction is a poor quality of movement that can result from co-contraction of antagonist muscles. Clients may demonstrate dyscoordinate co-contraction when they use excessive effort with exercise or when they fear pain with exercise or PROM, or it may be habitual. The resulting motion looks unpleasant and awkward. For example, you may feel the extensors contract as the client tries to activate the flexors. It is important not to ignore dyscoordinate co-contraction. Instead, teach the client pain-free, smooth movements that feel pleasant to perform. Replace isolated exercises with purposeful or functional activities and try proximal oscillations (small, gentle, rhythmic motions) to facilitate a more effective quality of movement. Biofeedback or electrical stimulation may also be helpful. Imagery offers additional possibilities (for example, ask your client to pretend to move the extremity through gelatin or water).7 Do not bark at the client to “Relax!” Instead, be gentle with your voice and your verbal cues.
Adjunct Treatments
Superficial heating agents can have beneficial effects on analgesic, vascular, metabolic, and connective tissue responses. Analgesic effects are seen in diminished pain and elevated pain tolerance. Vascular effects are evidenced by reduced muscle spasms and improved pain relief. Metabolic effects are related to an increased flow of blood and oxygen to the tissues with improved provision of nutrients and removal of byproducts associated with inflammation. Connective tissue effects include reduced stiffness with improved extensibility of tissues.8
Application of external heat (for example, hot packs) is a popular method in many clinics. Although the use of heat is fine if it is not contraindicated, be mindful that heat increases edema, which acts like glue, and this may contribute to stiffness. Heat can degrade collagen and may contribute to microscopic tears in soft tissue.9 For these reasons, be very gentle and cautious if you perform PROM after heat application. Monitor the situation to make sure that the overall benefits of heat outweigh any possible negative responses. Measuring edema is a good way to objectify these responses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree