Functional vision changes in the normal and aging eye
Bruce P. Rosenthal and Michael Fischer
Demographics
The World Population Clock showed 7 069 054 252 in one instant on 28 February 2013. The world population total is expected to rise to over 11 billion by 2050 (US Census Bureau, 2013) (see Table 51.1).
Table 51.1
Projected increase in global population between 2005 and 2030, by age
| Age | Increase |
| 0–64 | 21% |
| 65+ | 104% |
| 85+ | 151% |
| 100+ | 400+% |
The 21st century has continued to experience a dramatic increase in the aging population throughout the United States of America as well as the world. The number of individuals aged 85 and older, as well as centenarians, will grow significantly for the first time in history. The upswing in aging in developed as well as developing nations reflects a similar increase in aging. Many of these factors include healthcare management, decrease in fertility rates, increase in chronic diseases, health and diet awareness campaigns, training of medical and ancillary personnel, early diagnosis and early treatments. These dynamics in turn have translated into an increase in the ‘old old’ worldwide, especially where half of the world’s oldest of the old reside: China, the US, India, Japan, Germany and Russia. (The National Eye Institute distinguishes between the old and the oldest old, for research and policy purposes, as people age 85 and over.) One of the more remarkable worldwide statistics is that by 2030, nearly 24% of all older Japanese are expected to be at least 85 years old (National Institute on Aging, 2011).
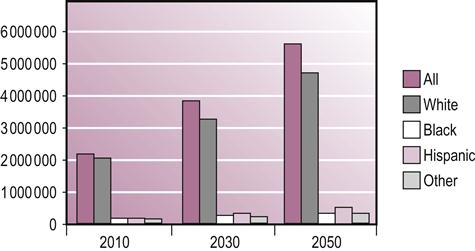
The increased aging population, throughout the world, will translate into greater numbers of persons developing age-related eye diseases. There is a 1.8% (3 377 037) rate of vision disability in the age group of 18–64 years (192 699 903). This increases to 36.6% (14 658 874) in the 65 years and over population of 40 086 253 (United States Census Bureau, 2012) (see Table 51.2 and Fig. 51.1).
Table 51.2
Prevalence of adult vision impairment and age-related eye disease in the United States of Americaa
| Total population≥40 | 142 648 393 |
| All vision impairment | 4 195 966 |
| Blindness | 1 288 275 |
| Myopia≥1.0 diopters | 34 119279 |
aEstimated number of cases by vision problem : age≥40 years.
Based on 2010 US Census populations.
The dramatically aging demographic shift converts into greater numbers of individuals who will experience changes in vision as a result of the normal aging process. These changes range from a decrease in the ability to focus on the printed page (presbyopia), to the reduction in the production of tear fluid, to a need for greater illumination when reading. By 2020, there will also be an increased cohort who will experience a significant loss of vision from pathological eye conditions such as macular degeneration (Fig. 51.2), diabetic retinopathy, glaucoma, stroke and cataract. This will translate into an increase in persons with visual impairment, blindness and low vision.
Vision-Related healthcare costs
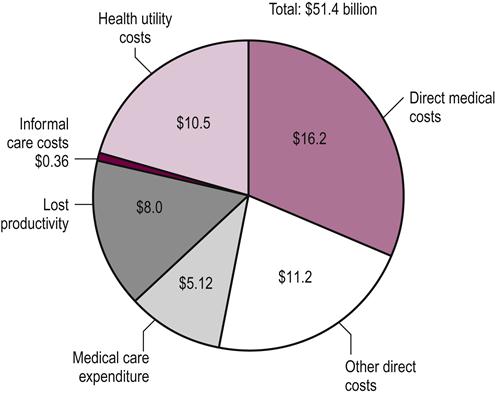
The annual burden to the US economy of age-related macular degeneration (AMD), cataract, diabetic retinopathy, glaucoma, refractive errors, visual impairment and blindness in adults age 40 and older was estimated in 2007 at $35.4 billion – $16.2 billion in direct medical costs, $11.1 billion in other direct costs and $8 billion in lost productivity (see Fig. 51.3).
Vision impairment and falls
Vision impairment has been found to be one of the leading causes of falls in the elderly, along with functional decline and depression. One study found that visual field loss was associated with a 6-fold risk of frequent falls (Wood et al., 2011).
Ramrattan et al. (2001) found that visual field loss, most commonly associated with glaucoma and stroke, was associated with a six-times risk of falling. Macular degeneration has been one of the eye diseases closely studied with regards to falls. Wood et al. (2011) found that persons with AMD reported a fall in 54% and more than two falls in 30% of the cohort studied. Of those falling, 63% of the falls reported resulted in injury. In another study on AMD, Soubrane et al. (2007) found that there was double the rate of falls in a population of persons as well as a quadrupled need for help with activities of daily living (ADLs).
The LALES study (Los Angeles Latino Eye) study followed 3202 Latino adults between 2004 and 2008. Decreased central vision from conditions such as macular degeneration and diabetic retinopathy and peripheral vision loss from conditions such as glaucoma and stroke resulted in more frequent and more serious falls. Macular degeneration is the major condition resulting in vision loss in Caucasians in the US. Central vision loss increased risk of fall or injury by 2.8 times, while peripheral vision loss increased this risk by 1.4 times. Over a 1-year period, 54% of individuals with AMD reported a fall and 30% reported more than one. Of all reported falls, 63% resulted in an injury (Wood et al., 2011) (see Table 51.3). Researchers concluded that elderly patients’ peripheral vision is a large factor in their chances of falling (Patino et al., 2010).
Table 51.3
Characteristics of falls and injuries sustained among older adults with AMD over a 12-month period
| No. falls | Percent | |
| All falls | 102 | 100 |
| Injurious falls | 64 | 63 |
| Injury sustained | ||
| Soft-tissue injury | 55 | 86 |
| Fracture | 4 | 6 |
| Head trauma | 5 | 8 |
Excerpted from Wood et al., 2011, Table 2.
Mogk and Watson (2008) have pointed out that seniors often rely on their vision to compensate for other age–related losses, so that when vision is lost too, they are particularly vulnerable to age-specific functional declines and dangerous falls.
Dual sensory loss, including hearing loss with vision loss, as well as other impairments, further contributes to falls. In the geriatric population, on average, sensory impairment doubles the number of falls, as noted by Harwood (2001; Harwood et al., 2005, 2009). Harwood’s suggestions for decreasing the number of falls include ‘simple interventions’ such as correcting refractive error as well as operating on cataracts.
Other concerns about vision changes
As noted, there is a sharp increase in the incidence of ocular disease in the seventh, eighth and ninth decade of life. It is, however, important to look at the changes in the visual system of the normal aging eye in order to understand, as well as differentiate these deviations from more serious changes in vision. These changes may be the result of comorbidities such as stroke, ocular pathology such as the complications from diabetes, hypertension, high cholesterol, auto-immune disease, tumors, kidney and heart disease.
Polypharmacy, common in the age group cited, may have serious implications in persons with low vision and may have a profound affect in adversely affecting the visual system. Zagar and Baggarly (2010) in fact point out that individuals with visual impairment have difficulty reading prescription and nonprescription medication information. They may even take the wrong medication or incorrect doses of medication which may result in serious negative consequences, including overdoses or inadequate treatment of health problems. This in turn may lead to emergency room visits or hospitalization.
The majority of individuals with vision loss also report increased anxiety related to medication management and having to rely on companions, or in some cases complete strangers, to obtain necessary drug information. Furthermore, 65% of Americans indicate that if they were to have severe vision loss, they would be most concerned about not being able to properly identify their medications (American Foundation for the Blind, 2004, 2008).
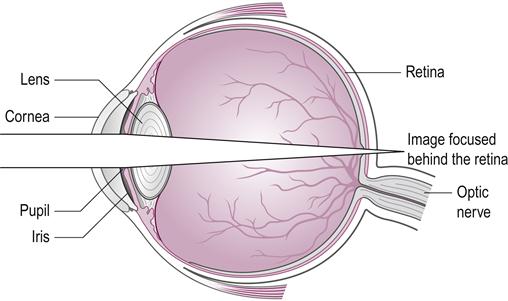
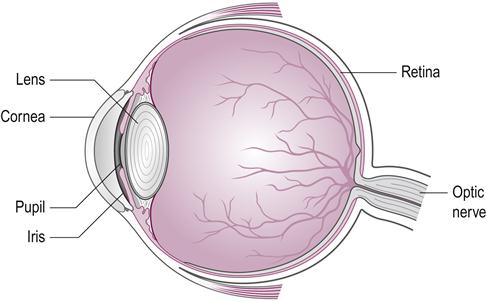
Presbyopia is an eye condition which makes its appearance as one of the earliest signs of aging of the visual system as well as the body. The word presbyopia comes from the Greek word presbys (πρ σβυς), meaning ‘old’, ‘elderly’, and the Neo-Latin suffix -opia, meaning ‘sightedness’ (Merriam-Webster Online Dictionary, 2013). Presbyopia generally begins in the early 40s and may be evident when the print is blurry, your arms are too short to hold text far enough away and fatigue sets in with prolonged close work as well as with using a computer or electronic device. The ability to accommodate or focus for close work such as reading or intermediate tasks such as the computer is known as accommodation. The near point of vision is the closest that one can accommodate (focus the eye) close up. The near point of the eye is generally considered to be about 3 in (7 cm) at age 10 moving out to about 6 in (16 cm) at age 40 and 39 in (1 meter) at age 60. As a result, a person from age 40 to 45 may require corrective lenses to read at a ‘normal’ reading distance, of 14–18 in (35–45 cm) (Fig. 51.4). The distance will depend on the length of one’s arms as well, since the further from the eye the print is held, the less the accommodative demand required for reading. The accommodative demand is also dependent upon the near visual task. It is normally accompanied by a convergence of the eyes to keep them directed at the same point, sometimes termed the accommodation convergence reflex (Bhola, 2006).
σβυς), meaning ‘old’, ‘elderly’, and the Neo-Latin suffix -opia, meaning ‘sightedness’ (Merriam-Webster Online Dictionary, 2013). Presbyopia generally begins in the early 40s and may be evident when the print is blurry, your arms are too short to hold text far enough away and fatigue sets in with prolonged close work as well as with using a computer or electronic device. The ability to accommodate or focus for close work such as reading or intermediate tasks such as the computer is known as accommodation. The near point of vision is the closest that one can accommodate (focus the eye) close up. The near point of the eye is generally considered to be about 3 in (7 cm) at age 10 moving out to about 6 in (16 cm) at age 40 and 39 in (1 meter) at age 60. As a result, a person from age 40 to 45 may require corrective lenses to read at a ‘normal’ reading distance, of 14–18 in (35–45 cm) (Fig. 51.4). The distance will depend on the length of one’s arms as well, since the further from the eye the print is held, the less the accommodative demand required for reading. The accommodative demand is also dependent upon the near visual task. It is normally accompanied by a convergence of the eyes to keep them directed at the same point, sometimes termed the accommodation convergence reflex (Bhola, 2006).
Distance, font size and contrast may also affect the accommodative demand. A computer, for example, is generally placed at 24 in (60 cm) or greater from the eye, while an electronic or digital device may be held at a closer distance. The font and the contrast will also allow an increase in the working demand with a decrease in the accommodative demand.
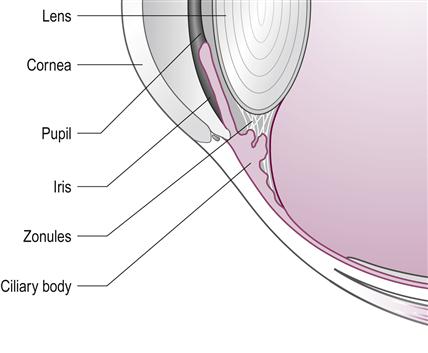
The mechanical system that regulates the flexibility of the human lens to become more convex (accommodate) for close work requires not only the lens but the ciliary body and the zonules (tiny guy wires in the insert connecting the lens to the ciliary body which help to make the lens more convex to see close up) (see Figs 51.5 and 51.6).
Age-Related eye diseases
The most prevalent age-related eye diseases include:
• AMD and other conditions of the retina
• Glaucoma
• Visual field loss resulting from stroke, ischemia and tumors.
Age-Related macular degeneration (AMD)
AMD is a leading cause of vision loss in the US (Fig. 51.7). AMD may result in a destruction of the macula, the critical zone of the retina that provides the highest resolution for sharp, central vision needed to see objects clearly.
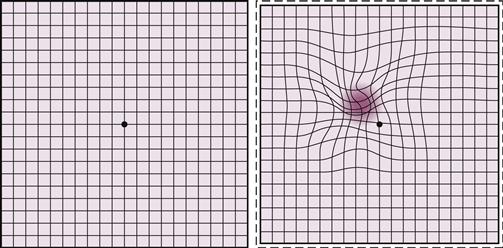
The macula is the small central portion of the retina that subtends an area of 20° of the visual field at 13 in (33 cm) from the eye. This 20° area is used to evaluate the integrity of the visual function with the use of a grid (the Amsler grid) that is 20×20 squares with each subtending an angle of 1° at that distance. Figure 51.8 illustrates a normal-appearing Amsler compared to an Amsler grid that has been impacted by a significant loss from AMD.
But the macula is integral for the quality of the central vision and color vision, as well as fine detail. The center of the macular, the fovea, has the highest density of receptors and is responsible for being able to read newsprint or the print on a prescription bottle. The macula has the highest density of the color receptors in the eye. The macula also plays an important role in regulating the ability to adapt to changes in conditions of illumination.
The retina is a complex structure that includes the photoreceptors (rods and cones) as well as the RPE (retinal pigment epithelial layer). The RPE, which cannot regenerate, plays a role in removing debris from the eye. Damage to the macula from the debris (also known as drusen) affects central vision and may result in blurring, distortion and loss of areas of vision (scotomas).
AMD is an umbrella term that includes dry and wet AMD. As noted in the statistics, it is a major cause of visual impairment in Caucasians throughout the world. The wet type of AMD is considered to be more destructive to visual function. But new treatments have been developed that preserve the vision. The treatment for wet AMD may involve anti-VEGF (vascular endothelial growth factor) injections.
Low vision remediation includes the prescription of low vision devices (see section on LV devices). It is also important to include a discussion on the use of anti-oxidants, including vitamin C, zinc and copper, as well as lutein and omega-3 in the treatment of AMD.
Cataracts
Cataracts are the most common age-related eye condition. They are best described as a clouding of the normally clear lens of the eye. The changes may range from an early opacification that causes little or no interference to vision to dense cloudiness, which results in marked visual impairment. The rate of progression of cataracts varies from person to person as well as between the right and left eye of the same individual.
A cataract is most common in age-related changes in the structure of the lens of the eye which manifests itself with symptoms that include: blurry vision, disability glare and difficulty when trying to read, for example, the highway signs when driving (see Fig. 51.9). The prevalence of cataracts increases with age, but may also be related to systemic pharmacological treatment of systemic conditions, such as the use of corticosteroids, as well as trauma.
Cataract surgery in the absence of other ocular pathologies, such as AMD, will result in a return to normal visual functioning. Treatment involves replacement of the normal lens with intraocular lenses by means of non-invasive stitchless surgery. New implant lens replacements have been complemented with multifocal implants. Patients will, however, have decreased vision following surgery when another pathological condition exists, such as AMD. Cataract surgery is generally performed when visual function, as well as visual efficiency, is reduced. Pre-existing conditions, particularly wet AMD, complicate the situation and necessitate a discussion with the ophthalmologist on the risks and benefits.
Symptoms of cataracts may include glare sensation to oncoming headlights of automobiles, a reduction of vision when wearing sunglasses, the need to shade the eyes when going outdoors in the sun, glare from fluorescent ceiling lights or bright reading lamps, or difficulty seeing street or highway signs.
Glaucoma
Glaucoma is a major health concern since vision loss may be progressive without evidence of pain. It is one of the most common age-related conditions that may result in serious vision loss when undiagnosed or not treated. The eye pressure generally ranges from 10 to 20 mmHg. The loss of the visual field from glaucoma can be profound and affect mobility, peripheral and night vision when the pressure is elevated or compromised, with other compounding factors including the thickness of the cornea.
The analogy of a drain outflow being affected can illustrate why vision can be lost from a ‘clogged’ drainage system in the eye. Aqueous fluid is continuously produced and drained by the trabecular meshwork which in turn drains the aqueous into the venous drainage in the eye. Obstruction of the aqueous fluid through the drainage trabecular meshwork may result in fluid build-up. The increase in the intraocular pressure without adequate drainage through the canal of Schlemn may damage the optic nerve. Damage to the optic nerve may affect quality of life, ADLs and, especially, mobility under conditions of poor illumination. Glaucoma is a very complex eye disease that was formerly thought to be the result of elevated eye pressure only. But new models have shown that the corneal thickness plays a role in destroying cells in the optic nerve with pressure heretofore thought to be normal. Progressive optic nerve loss from glaucoma may impair night vision, mobility and functioning in poorly lit or even crowded environments.
Treatment includes eye drops as well as surgical intervention. Despite the best efforts, longevity may result in a severe decrease in contrast and the usable visual field. Low vision coping interventions may include new glasses, improved lighting, or even prisms for mobility.
Diabetic retinopathy
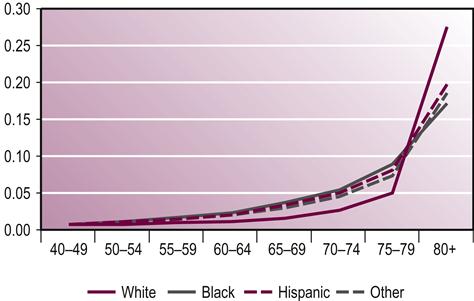
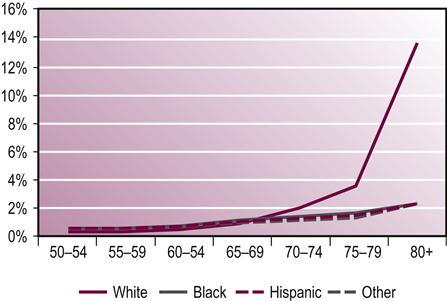
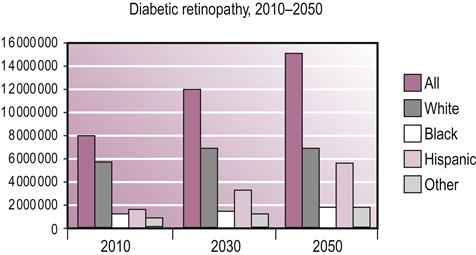
Diabetic retinopathy is the leading cause of blindness in American adults. The increase of diabetic retinopathy in the Caucasian, black, and especially Hispanic populations will be dramatic over the next 35 years. Diabetic retinopathy is the result of changes in the blood vessels of the retina. Individuals with diabetic retinopathy develop porous and leaky blood vessels that affect the photoreceptor layer (light-sensitive) tissue at the back of the eye. Diabetic retinopathy is treated with laser photocoagulation (PR) or steroids. The laser therapy preserves vision on one hand and destroys the peripheral or night vision on the other. Diabetes and diabetic retinopathy is predicted to be a major health crisis over the next 50 years (see Fig. 51.10 and Table 51.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree