Functional Spinal Rehabilitation
Lorraine Hendry BSc(PT), MCPA, FCAMT
Low back pain affects up to 80% of the population at least once in their lifetime.
The term core stabilization is used to describe the management of low back pain through training of the deep stabilizing muscles of the trunk to protect the spine and to allow improved motor control of the spine.
The spinal stability system features passive, active, and control subsystems, each of which is interdependent but capable of compensating for a deficit in another (1).
The multifidus is the most medial and largest of the paraspinal muscles. It has an origin and insertion from one vertebra to another within the lumbar spine and between the lumbar and sacral vertebrae.
The anterior, middle, and posterior layers of the thoracolumbar fascia create an envelope for the muscles of the lumbar spine.
The transversus abdominis is the deepest muscle of the abdominal muscle complex. It originates from the lateral one-third of the inguinal ligament, the anterior two-thirds of the inner lip of the iliac crest, the lateral raphe of the thoracodorsal fascia, and the internal aspect of the lower six costal cartilages interdigitating with the costal fibers of the diaphragm.
Pain can be significantly decreased and functional ability increased with lumbar stabilization exercises.
Proprioception may be assisted by postural retraining and stabilization exercises in neutral postures progressing to unstable surfaces in functional movements.
The supine active straight-leg raise test (ASLR) is a valid tool for assessing the load transfer between the trunk and lower extremities. When functioning normally and with adequate stability, the patient should be able to raise his or her straight leg from the table without a great deal of effort and without movement of the pelvis in relation to the thorax and lower extremity. This test combines observations by the patient and the doctor.
Functional exercise programs should be directed towards retraining the motor control in as many potential lumbar spine stabilizers, while in erect weight-bearing postures to stimulate day-to-day activities.
Low back pain is a common complaint and reportedly affects up to 80% of the population at least once in their lifetime (2). A recurrence of low back pain or chronic low back pain is seen in 10% to 40% of this population (2,3). “Eighty-five percent of low back pain patients are classified as ‘non-specific’ because a definitive diagnosis cannot be achieved by current radiological methods” (2).
The terms core stabilization and motor control have been used to describe the management of low back pain through training of the deep stabilizing muscles of the trunk to protect the spine and to allow improved movement of the spine in functional tasks (4,5).
Impairment to the lumbopelvic and hip regions requires integration and coordination of treatment approaches to allow effective load transfer between the lower extremity, the trunk, and the upper extremity. There must be a clear understanding of the causes of dysfunction when evaluating the lower quadrant, including the lumbar spine, pelvis, and lower extremity, to determine the causes of dysfunction. Optimal function requires both mobility and stability (6) in the joints and muscles of the lumbar spine and
pelvis. A lack of identification of the areas of dysfunction, and lack of follow-up with appropriate treatment, may lead to recurrence of low back pain in both daily and sporting activities. Athletes require coordination, strength, endurance, and flexibility between the trunk and extremities to be effective in achieving rapid and precise movements. Research has focused on the factors contributing to low back pain and on the treatment used to improve stability through improved motor control of the lumbar spine. This chapter reviews the literature concerning stabilization of the lumbar spine and current exercise programs.
pelvis. A lack of identification of the areas of dysfunction, and lack of follow-up with appropriate treatment, may lead to recurrence of low back pain in both daily and sporting activities. Athletes require coordination, strength, endurance, and flexibility between the trunk and extremities to be effective in achieving rapid and precise movements. Research has focused on the factors contributing to low back pain and on the treatment used to improve stability through improved motor control of the lumbar spine. This chapter reviews the literature concerning stabilization of the lumbar spine and current exercise programs.
Panjabi (5) introduced a spinal stability system that includes passive, active, and control subsystems. The passive subsystems involve the osteoarticular and ligamentous components, which provide restraint primarily in the end range of motion. The active subsystems are of great interest in the research and clinical fields for looking at the role of muscle and fascia and their ability to control the mechanical components of the spine segments. The control subsystems introduce neurological function as well as its effect and timing on motor control. The role of the neural subsystem is to coordinate feedback from the active and passive subsystems, with appropriate levels of muscular contraction to balance against destabilizing forces between the subsystems (7). The emotional or psychological subsystem (8) has been added to account for psychological and social factors influencing the patients’ pain and “their capacity to increase the central nervous system mediated drive of pain via the forebrain” (9,10,11).
The passive, active, and control subsystems are interdependent, with each one being capable of compensating for a deficit in another (1,5,12). Back pain may be related to a deficit in control of one subsystem and to an inability of the remaining subsystems to compensate for this deficit (4). A deficit in one subsystem may produce back pain as a result of decreased control of a spinal segment, with compression of neural and articular structures (1) (Fig 7-1).
Panjabi (1) described articular motion in the lumbar spine with the terms neutral and elastic zones: “The neutral zone is a region of intervertebral motion around the neutral posture where little resistance is offered by the passive spinal column” (1). The elastic zone is the part of the motion “from the end of the neutral zone up to the joint’s physiological limit” (1). He used the concept of a ball in a bowl to describe the neutral and elastic zones. The ball resting in the center of the bowl represents the neutral zone within a joint that has a higher degree of laxity (Fig 7-2). As the ball rolls toward the ends of the bowl, increasing resistance from the soft tissue is seen, as at the end of physiological range of motion in a joint with a stiffening effect. “The neutral zone of the spinal segment is dependent on the muscles for control and proprioceptive feedback” (13). Research indicates that the “lumbar spine’s vulnerability to instability is greatest in the neutral zone of motion, under low load conditions and where motor control of the spine is compromised” (14). The risk of injury in the elastic zone increases as the motor system relaxes to allow passive systems to provide restraint in the spinal segment (13).
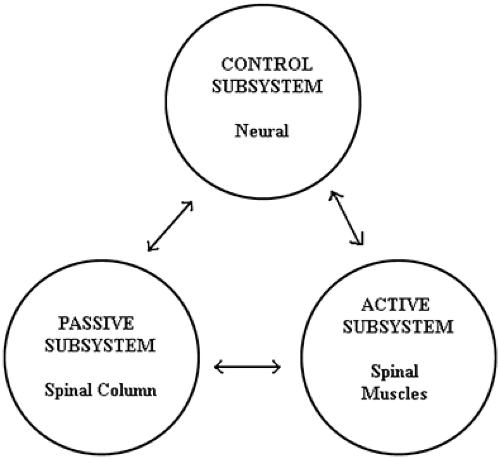 Fig 7-1. Spinal stability systems. (Adapted from Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5:390–396. ) |
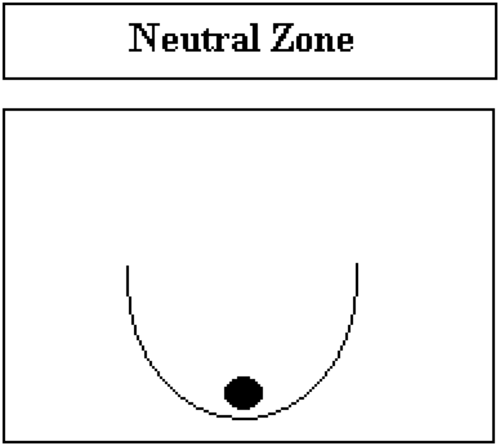 Fig 7-2. Neutral zone. (Adapted from Hodges PW. Science of stability: clinical application to assessment and treatment of segmental spinal stabilization for low back pain. Course Notes; 2000. ) |
Hypomobility is described as restricted movement within the articular surfaces of a joint. Hypermobility is described as excessive movement within a joint that is beyond a normal degree of movement before the stabilizing structures provide restraint.
According to Panjabi (1), “Clinical instability is a significant decrease in the capacity of the stabilizing system to maintain the intervertebral neutral zone within physiological limits so that there is no neurological dysfunction, no major deformity and no incapacitating pain.” He describes clinical instability as a lack of motor control within the
neutral zone (1). Motor control also has been described as “the way in which a task is performed. Altered motor control describes the manner by which the movement or posture has changed” (13). Clinical instability at a segmental level is seen with increased movement in the neutral zone and excessive motion at the end of range (15). “Instability of the lumbar motion segments is closely related to deep muscles which support and control intersegmental movement during functional tasks” (15). The size of the neutral zone may increase with disc degeneration, spinal injury, or poor muscle control, which will all affect stability (1).
neutral zone (1). Motor control also has been described as “the way in which a task is performed. Altered motor control describes the manner by which the movement or posture has changed” (13). Clinical instability at a segmental level is seen with increased movement in the neutral zone and excessive motion at the end of range (15). “Instability of the lumbar motion segments is closely related to deep muscles which support and control intersegmental movement during functional tasks” (15). The size of the neutral zone may increase with disc degeneration, spinal injury, or poor muscle control, which will all affect stability (1).
Bergmark (16) introduced the concept of two muscle classifications. These are the local and global stabilizing systems.
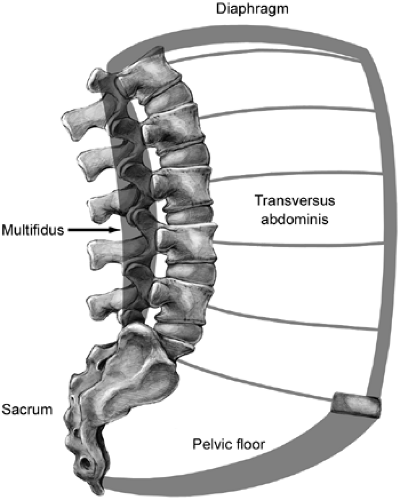
The local muscle groups provide specific segmental spinal stability through their attachment directly to the lumbar vertebrae. These muscles provide control of intersegmental motion and position of the lumbar spine (16). This group would include the transversus abdominis (TrA) (6,17,18), multifidus (19,20), and internal oblique (fiber insertion into thoracolumbar fascia) (16,21). Additional studies have found that the pelvic floor muscles (6,18,22,23,24), the diaphragm (18,25,26), and the intertransversarii, interspinales, longissimus thoracis pars lumborum, iliocostalis lumborum pars lumborum, and medial fibers of the quadratus lumborum (16) also are included as local stabilizing muscles. The TrA and internal oblique muscles provide stability for the lumbar spine through the thoracolumbar fascia along with the control of the intra-abdominal pressure. (27,28,29,30,31) (Fig 7-3).
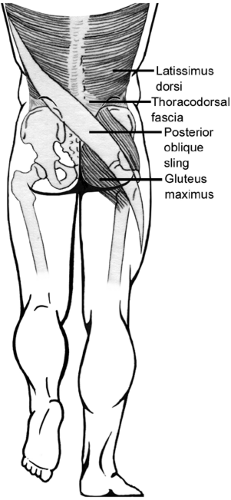
The global muscle groups provide large trunk movements and general trunk stability through their attachments between the thorax and pelvis and/or pelvis and legs, with no specific attachment to the lumbar spine (27). This group would include the rectus abdominis, external oblique, and thoracic erector spinae muscles, longissimus thoracis pars thoracis, iliocostalis lumborum pars thoracis, quadratus lumborum lateral fibers, and internal oblique (16). The global muscle group also has been described as being divided into four slings between the thorax, pelvis, and lower extremity (6,32,33,34). The posterior oblique sling would include the latissimus dorsi and the gluteus maximus via the thoracolumbar fascia. The anterior oblique sling would include the external oblique, the anterior abdominal fascia, the contralateral internal oblique abdominal muscle, and adductors of the lower extremity. The longitudinal sling involves connections between the peroneii, the biceps femoris, the sacrotuberous ligament, the deep lamina of the thoracodorsal fascia, and the erector spinae. The lateral sling includes the gluteus medius and minimus, the tensor fascia latae, and the lateral stabilizers of the thoracopelvic region (6,32,33,34). The integration between and within these slings provides stability and effective transfer of loads between the spine and the extremities. The local stabilizing muscle system sometimes is referred to in the literature as the inner unit, with the global stabilizing system being referred to as the outer unit (Fig 7-4).
A significant neurophysiological difference exists in the timing of the contraction of these two local and global muscular systems. Motor control refers to the “timing of specific muscle action and inaction” (6). When loads are predictable, the local system contracts in anticipation before the movement, regardless of the direction of movement (17,18,19,20,35,36). The global system contracts later and is direction dependent (6,18,37,38). Local muscles are controlled independently of the global system (4,12).
With low-load situations, the local muscle system is associated with low levels of intra-abdominal pressure and relaxed respiration. Activity is seen in the muscles of the pelvic floor, the transverse abdominal wall, the psoas, and the multifidus. The psoas acts synergistically with the lumbar multifidus to control the position of the pelvis on the hips and lordosis (13). The global muscle system is involved in posture and initiation of movement and is associated with low levels of intra-abdominal pressure and relaxed respiration (13). With high-load situations, the local and global systems co-contract, in association with higher levels of intra-abdominal pressure, to act as a splint and to restrict the movement of the pelvis and thorax (13).
Lee (6) has focused on the local system of the lumbopelvic region, including the pelvic floor, diaphragm, multifidus, and TrA, in looking closely at the evaluation and treatment of pelvic girdle dysfunction. Sapsford et al. (39) reported that “in healthy subjects, voluntary activity in the
abdominal muscles results in increased pelvic floor muscle activity.” Difficulties in establishing a stable base within the pelvic girdle will affect stabilization strategies of the lumbar spine and, therefore, need to be addressed concurrently.
abdominal muscles results in increased pelvic floor muscle activity.” Difficulties in establishing a stable base within the pelvic girdle will affect stabilization strategies of the lumbar spine and, therefore, need to be addressed concurrently.
Multifidus
The multifidus is the most medial and largest of the paraspinal muscles. It has an origin and insertion of vertebra to vertebra attachments within the lumbar spine and between the lumbar and sacral vertebrae (12,40).
The multifidus is composed of repeating fascicles, which originate from the laminae and spinous processes of the lumbar vertebrae and insert in a caudal direction. The shortest (deepest) fascicles (laminar fibers) of the multifidus arise from the vertebral laminae and insert on the mamillary process of the vertebrae two levels caudal. The L5 fibers insert on an area of the sacrum just above the first dorsal sacral foramen (12). “The other fascicles arise from the spinous process and are longer than the laminar fibers. Each lumbar vertebra gives rise to one group of fascicles which overlap those of the other levels. The fascicles from a given spinous process insert onto mamillary processes of the lumbar and sacral vertebrae three, four, or five levels inferiorly. The longest fascicles, from L1, L2, and L3, have some attachment to the posterior superior iliac spine” (12). The fascicles in each group diverge caudally to assume separate attachments to mamillary processes, the iliac crest, and the sacrum. Some of the deeper fibers of these fascicles attach to the capsules of the zygapophyseal joints next to the mamillary process. “The attachment of the muscles of the thoracolumbar fascia represents a raphe separating the multifidus from the gluteus maximus muscle” (41) (Fig 7-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree