Chapter 2 Functional Medicine
A Twenty-First Century Model of Patient Care and Medical Education
 What is Functional Medicine?
What is Functional Medicine?
One way to conceptualize where functional medicine falls in the continuum of health and health care is to examine the functional medicine “tree.” In its approach to complex chronic disease, functional medicine encompasses the whole domain represented by the graphic shown in Figure 2-1, but first addresses the patient’s core clinical imbalances (found in the functional physiologic organizing systems), the fundamental lifestyle factors that contribute to chronic disease, and the antecedents, triggers, and mediators that initiate and maintain the disease state. Diagnosis, of course, is part of the functional medicine model, but the emphasis is on understanding and improving the functional core of the human being as the starting point for intervention.
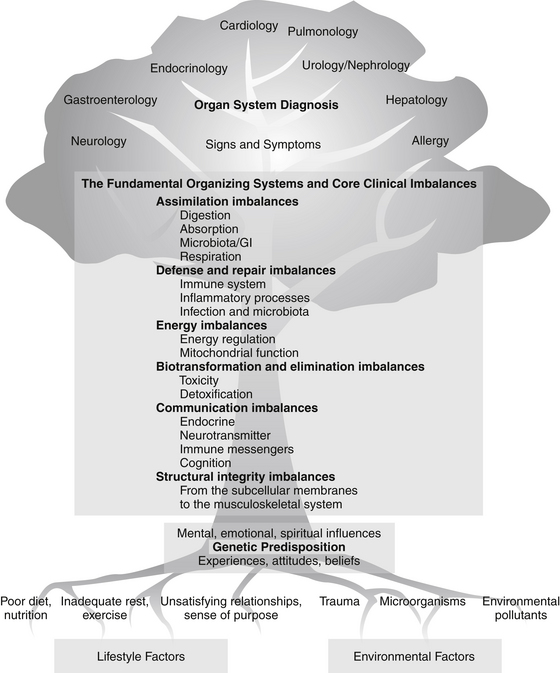
FIGURE 2-1 The continuum of health and health care: the functional medicine tree.
(Courtesy of the Institute for Functional Medicine.)
Functional medicine clinicians focus on restoring balance to the dysfunctional systems by strengthening the fundamental physiologic processes that underlie them and by adjusting the environmental and lifestyle inputs that nurture or impair them. This approach leads to therapies that focus on restoring health and function, rather than simply controlling signs and symptoms.
Principles
Seven basic principles characterize the functional medicine paradigm:
• Acknowledging the biochemical individuality of each human being, based on the concepts of genetic and environmental uniqueness
• Incorporating a patient-centered rather than a disease-centered approach to treatment
• Seeking a dynamic balance among the internal and external factors in a patient’s body, mind, and spirit
• Addressing the web-like interconnections of internal physiologic factors
• Identifying health as a positive vitality—not merely the absence of disease—and emphasizing those factors that encourage a vigorous physiology
• Promoting organ reserve as a means of enhancing the health span, not just the life span, of each patient
• Staying abreast of emerging research—a science-using approach
Lifestyle and Environmental Factors
The building blocks of life, as well as the primary influences on them, are found at the base of the functional medicine tree graphic (see Figure 2-1). When we talk about influencing gene expression, we are interested in the interaction between lifestyle and environment in the broadest sense and any genetic predispositions with which a person may have been born—including the epigenome.* Many environmental factors that affect genetic expression are (or appear to be) a matter of choice (such as diet and exercise); others are very difficult for the individual patient to alter or escape (air and water quality, toxic exposures); and still others may be the result of unavoidable accidents (trauma, exposure to harmful microorganisms). Some factors that may appear modifiable are heavily influenced by the patient’s economic status—if you are poor, for example, it may be impossible to choose more healthful food, decrease stress in the workplace and at home, or take the time to exercise and rest properly. Existing health status is also a powerful influence on the patient’s ability to alter environmental input. If you have chronic pain, exercise may be extremely difficult; if you are depressed, self-activation is a major challenge.
The influence of these lifestyle and environment factors on the human organism is indisputable,1,2 and they are often powerful agents in the battle for health. Ignoring them in favor of the quick fix of writing a prescription—whether for pharmaceutical agents, nutraceuticals, or botanicals—means the cause of the underlying dysfunction may be obscured but not eliminated. In general terms, the following factors should be considered when working to reverse dysfunction or disease and restore health:
• Diet (type, quality, and quantity of food; food preparation; calories, fats, proteins, carbohydrates)
• Nutrients (both dietary and supplemental)
• Microorganisms (and the general condition of the soil in which food is grown)
• Psychosocial and spiritual factors, such as meaning and purpose, relationships, work, community, economic status, stress, and belief systems
Fundamental Physiologic Processes
These fundamental physiologic processes are usually taught early in health professions curricula, where they are appropriately presented as the foundation of modern, scientific patient care. Unfortunately, subsequent training in the clinical sciences often fails to fully integrate knowledge of the functional mechanisms of disease with therapeutics and prevention, emphasizing organ system diagnosis instead.3 Focusing predominantly on organ system diagnosis without examining the underlying physiology that produced the patient’s signs, symptoms, and disease often leads to managing patient care by matching diagnosis to pharmacology. The job of the health care provider then becomes a technical exercise in finding the drug or procedure that best fits the diagnosis (not necessarily the patient), leading to a significant curtailment of critical thinking pathways: “Medicine, it seems, has little regard for a complete description of how myriad pathways result in any clinical state.”4
Even more important, pharmacologic treatments (and even natural remedies) are often prescribed without careful consideration of their physiologic effects across all organ systems, physiologic processes, and genetic variations.5 Pharmaceutical companies exploit this weakness. We do not see drug advertisements that urge the practitioner to carefully consider the impact of all other drugs being taken by the patient before prescribing a new one! The marketing of drugs to specific specialty niches, and the use of sound bite sales pitches that suggest discrete effects, skews health care thinking toward this narrow, linear logic, as notably exemplified by the cyclooxygenase-2 inhibitor drugs that were so wildly successful on their introduction, only to be subsequently withdrawn or substantially narrowed in use due to collateral damage.6,7
Core Clinical Imbalances
Biotransformation and Elimination Imbalances
Structural Integrity Imbalances
Using this construct, it becomes much clearer that one disease and/or condition may have multiple causes (i.e., multiple clinical imbalances), just as one fundamental imbalance may be at the root of many seemingly disparate conditions (Figure 2-2).
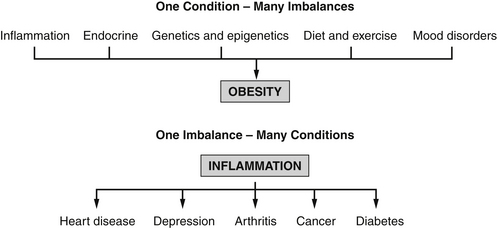
FIGURE 2-2 Core clinical imbalances—multiple influences.
(Courtesy of the Institute for Functional Medicine.)



