Frailty in older persons
Martha Acosta
Introduction
The concept of frailty usually evokes an image of an older person barely able to stand and/or laboriously walking with an assistive device across the room of an extended care facility. Although the end stages of frailty may have some semblance to this picture, the frailty phenotype is now known to be more variable and modifiable with evidence-based therapeutic interventions. Perhaps most importantly it is possible to identify and reduce the risk for frailty, even amongst the oldest-old population.
Frailty is a distinct and multidimensional clinical syndrome (Fried et al., 2001), and is commonly associated with declining status in physical and functional states that are associated with physiological, social and emotional changes. From this perspective, deteriorating health can result in a loss of reserves in energy, physical ability, cognition and health. When combined, these factors give rise to vulnerability (Rockwood, 2005). However, studies of frail older adults have identified positive benefits from training to functional capacity in areas, including increased gait speed (Chandler et al., 1998: 91), decreased risk of falls (Liu-Ambrose et al., 2004) and improved physical endurance (Ehsani et al., 2003). Even older adults in the ninth decade of life can show increases in muscle strength from resistance exercise training, despite the age-related changes in muscle strength (Fiatarone et al., 1990).
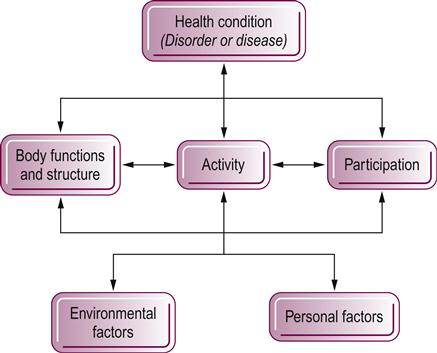
To fully appreciate frailty from a comprehensive framework, it is useful to consider the domains of health that make up the International Classification of Functioning, Disability and Health (ICF) model (Fig. 65.1). In this model, the domains impacting the frail (health) condition can be external and/or internal to the individual. In addition, the model itself can provide an integrated framework with terms that are compatible to those used in frailty language. An analysis of that compatibility determined that the functional status indicators defined in the classification scheme of the ICF model provided a profile of frailty that reflects the multifactorial aspect of the frail condition (Nash, 2008). Thus, a thorough assessment of all the potential domains that may be involved with a frail older adult is critical. But, preceding a discussion of its multidimensional nature, frailty must first be defined. There is no complete agreement on a standardized definition of frailty, which may explain in part how the image of a person barely able to move through the environment and/or in a certain age category are often the only criteria used to define frailty. An examination of how definitions of frailty have evolved is a starting point in the following discussion. Noting the research studies that have specified frailty criteria will help the clinician determine the most appropriate tool to use for screening and/or for patient treatment outcomes.
Historical perspective
Frailty is typically associated with declining health, functional status and the loss of abilities. A commonly held belief is that frailty is an inevitable part of the aging process. However, some older persons never become frail and some younger persons can be characterized as frail. Reviewing the progression of ideas over time that have lead up to proposed models of frailty will help clarify the definitions-in-progress of frailty used in clinical care and research.
In the early 1970s the term frailty was used synonymously with institutionalization (Abellan van Kan et al., 2008). Then, the concept of failure to thrive, which referred to weight loss with cognitive and functional decline at the end of life, was introduced in the late 1980s (Braun et al., 1988). A practical definition of frailty was reported in 1994 as persons needing help with activities of daily living (ADLs) or at a high risk of becoming dependent (Rockwood et al., 1994). A more multidimensional definition was reported in 1998 that includes 16 variables across four functional domains (physical, cognitive, nutritive and sensory domains) (Box 65.1). If impairments existed in two or more domains, the individual was considered frail (Strawbridge et al., 1998).
Other authors defined frailty as it relates to disability (Campbell & Buchner, 1997). A few years later, the definition included the concept of risk due to instability of health, where frailty leads to an increased risk of disability and death (Rockwood et al., 1999). As the conceptualization of frailty expanded, so did its definitions, which reflected the increased understanding of its multidimensionality.
Defining frailty
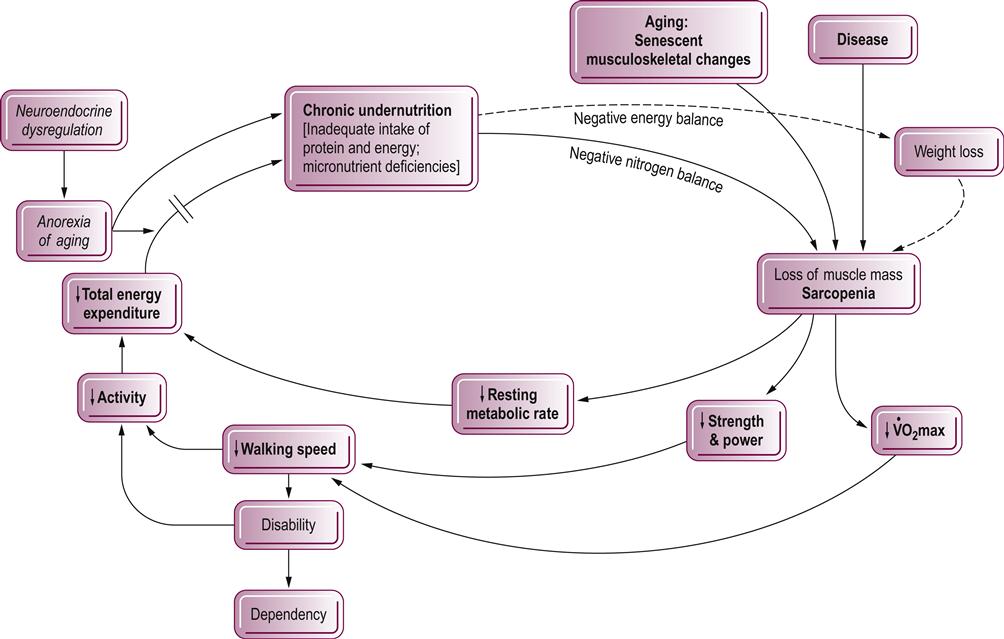
Frailty research has grown exponentially over the past 20 years. In the majority of studies, multisystem involvement and decreased reserve capacity across all systems are characteristic of the syndrome of frailty. In 2002, Bortz defined frailty as the result of early disease in multiple systems, resulting in impaired muscle strength, mobility, balance and endurance (Bortz, 2002). Similar references to frailty as a biologic syndrome in which reserves and resistance to stressors are diminished, further suggest that the decline in a multiplicity of systems leads to vulnerability for adverse outcomes (Buchner & Wagner, 1992; Lipsitz & Goldberger, 1992). Based on the markers of frailty accepted by several researchers, Fried et al. (2001) formulated a set of frailty criteria (frailty phenotype) including age-related losses in strength, lean muscle mass, balance, endurance, walking performance and low physical activity (Fried et al., 2001). Presence of three or more of these criteria identify a person as being frail (Fig. 65.2).
Fried utilized data from the Cardiovascular Health Study, a prospective, observational study of 5317 men and women 65 years and older recruited from four US communities. This frailty phenotype has demonstrated predictive validity for adverse outcomes that geriatricians associate with frailty: increased risk for falls, disability, hospitalization and death. Frailty remained an independent predictor of risk for these adverse outcomes even after adjusting for socioeconomic status, health status, clinical and subclinical disease, depressive symptoms and disability status at baseline.
The current literature suggests that frailty is best described as an aggregation of relevant domains into phenotypes. The discussion centers mostly on deciding whether physical, cognitive, social and functional domains should be components of the model for frailty outcomes. An example of this controversy regarding measurement is the concept of disability and whether it is considered a component of the syndrome or an outcome (Abellan van Kan et al., 2010). However, it is widely accepted that frailty is a clinical syndrome resulting from multisystem impairments that are separate from the normal aging process. Grouping these impairments into a phenotype provides a basis for various assessment measures used in research.
The two main phenotypes used in assessments are the phenotype of physical frailty and the multidomain phenotype that includes cognitive, functional and social aspects (Morley et al., 2006: 41). The physical phenotype includes five measurable items (weight loss, exhaustion, weak grip strength, slow walking speed and low energy expenditure) that identify frailty and has consistently predicted poor clinical outcomes. An overall grouping of functional impairments formed the basis for this phenotype (Fried et al., 2001). The multidimensional phenotype includes components such as cognitive impairment, chronic diseases, sensory impairment, mood disorders, poor social conditions and support, and disability (Morley et al., 2006).
The physical phenotype based on an operational definition of frailty has been conceptualized as a syndrome with diminished physiologic reserves and resiliency, where a cycle of declining systems results in decreased endurance for exertion, decreased strength, sarcopenia and a negative balance of energy. Within this phenotype, the five measurable characteristics identifying frailty include weight loss, exhaustion, weak grip strength, slow walking speed and low energy expenditure. A person is classified as frail if three or more of the criteria are met. If only one or two criteria are met, the category is labeled intermediate. If no criteria are met, an individual is considered robust. With the data from the Cardiovascular Health Study (4317 community-dwelling adults aged 65 and over) and using these criteria, a 7% prevalence of frailty was found, increasing to 30% in the subgroup 80 years and older (Fried et al., 2001). In the Women’s Health and Aging Studies (moderately to severe disabled population of 1002 community-dwelling women aged 65 and over), a 28% prevalence of frailty was identified (Bandeen-Roche et al., 2006). Additionally, in these cohorts the phenotype classification predicted poor clinical outcomes, including falls, hospitalization, development of disability and mortality (Fried et al., 2001).
In addition to the five criteria of the physical phenotype, the multidomain phenotype includes cognitive, functional and social circumstance domains. Addition of these factors has added value to the predictive capacity of the physical phenotype for projecting poor outcomes. This aggregation of the domains is referred to as expanded model of physical frailty (Abellan van Kan et al., 2010).
In one multidomain model, researchers from the Canadian Study of Health and Aging (CSHA) examined function with regard to comorbidity and disability (Theou et al., 2012). Although considered distinct entities, comorbidity and disability are related conceptually according to the physical phenotype. As reported by Theou et al, results from Fried’s study in 2004 indicated the proportion of older women were more frail compared to older men, and had more ADL impairments; men had a higher death rate and reported more chronic conditions. Fewer than 10% of persons who were frail did not experience any comorbidity or disability. Also, ADL limitations and chronic diseases occurred more frequently in the group with the highest levels of frailty (Theou et al., 2012). The presence of chronic diseases will impact clinical management of the older patient and may help explain the higher mortality among men compared to women. The impact of multiple chronic diseases is well known to physical therapists working with the older patient. In the area of cognition, dementia can be considered an outcome or a component of frailty depending on which definition is used. The addition of lower cognitive function to the physical phenotype does slightly increase the prediction of developing disability although there was no effect on mortality as identified in the MacArthur Study of Successful Aging, a longitudinal cohort study (Sarkisian et al., 2008; Avila-Funes et al., 2009). When considering socioeconomics and frailty, a statistically significant association was found between lower health-related quality of life scores and frailty in the Hispanic Established Populations for the Epidemiological Studies of the Elderly (EPESE) (Masel et al., 2009). Similarly, a statistically significant association was found between lower socioeconomic status (SES) and frailty in the Women’s Health and Aging Studies. In this cross-sectional analysis of 727 older women, the odds of frailty among women of low SES increased independent of age, race, insurance, smoking status and comorbidities (Szanton et al., 2010). Overall, the multidomain phenotypes have added clinical significance to the assessment process with frail older adults.
In addition to the phenotypes, another approach to operationalizing frailty uses the concept of deficit accumulation whereby a Frailty Index (FI) is constructed. The index is calculated as the proportion of the number of deficits present to the number of deficits counted (Mitnitski et al., 2001; Jones et al., 2004). The index was determined from 92 variables representing a range of disabilities and health conditions. Variables for the frailty index included symptoms, signs, comorbidities, functional impairments, abnormal lab values and disabilities. The summed scores are then stratified to define three levels of frailty: mild, moderate and severe. Clinically the FI gives an overview of health status and permits the risk stratification of potential adverse outcomes. Clinical applications of the FI have been used to describe functional and clinical characteristics of frailty as well as examine differences in health status comparing rural and urban older adults. Hence, the tool assessed the risk of death better than measures of comorbidity, function or cognition.
Biological foundations of frailty
Factors that underlie the cause of frailty continue to be the subject of geriatric research. Although all the mechanisms involved remain unclear, an essential cause of frailty that has been proposed is a multisystem dysregulation of the neuromuscular, endocrine and immune systems (Ko, 2011). Collectively, these system changes may have synergistic adverse effects greater than the age-related or disease-related individual factors; therefore, it is important to examine this concept in more detail.
Age-related sarcopenia (loss of muscle mass) accelerates after age 50 (Rice et al., 1989; Metter et al., 1997). Loss of muscle mass and strength is reflected in most definitions of frailty. Sarcopenia can be defined in a formal assessment of body composition using dual-energy X-ray absorptiometry that can produce estimates of lean body mass. Absolute values or scores are reported relative to normal gender-specific values and skeletal size, the ‘relative skeletal muscle index’ (RSMI). Sarcopenia defined by the RSMI is<2 standard deviations below normal in approximately 15% of persons aged 60–69 years and approximately 40% of those over 80 years (Fried et al., 2009). The biological basis for muscle decline includes age-related changes in type I muscle fibers, alpha-motor neurons, growth hormone (GH) production, sex steroid levels, inflammatory markers and physical activity (Fried et al., 2009). However, the age-related loss of muscle mass is modifiable with resistance training in the older adult. This topic will be discussed in more detail later in the chapter.
Although sarcopenia is a central manifestation of frailty, the age-related decline in muscle mass is modulated by several physiologic factors, including hormones, neurologic integrity, nutritional status, physical activity and inflammation (Fried et al., 2009). With regards to the endocrine system, hormones that are crucial to skeletal muscle metabolism include sex steroids and insulin growth factor (IGF-1). Lower levels of these hormones contribute to age-related loss of muscle mass and strength, particularly decreased estrogen in postmenopausal women and testosterone in older men (Poehlman et al., 1995; Morley et al., 1997). In addition, serum levels of the sex hormone dehydroepiandrosterone sulfate (DHEA-S) and IGF-1 are significantly lower in frail versus non-frail older women (Leng et al., 2004). In relation to outcomes, lower levels of IFG-1 are also associated with poor muscle strength, slow walking speed, progressive disability and increased mortality as evidenced in the Women’s Health and Aging Study (Cappola et al., 2001, 2003). Future investigations in these modulatory functions will broaden our understanding of frailty.
In common with many other conditions, the immune system has been linked to frailty. Chronic elevation of serum levels of proinflammatory cytokine interleukin 6 (IL-6) which is characteristic of chronic inflammation, is strongly associated with frailty (Leng et al., 2002). Also, IL-6 has been strongly associated with weight loss, increased susceptibility to infections and adverse physiologic effects of sarcopenia. It may also contribute to anemia by interfering with iron metabolism or by directly inhibiting erythropoietin production (Ershler, 2003). Finally, elevated white blood cell (WBC) counts and IL-6 levels were independently associated with prevalent frailty in community-dwelling older women in the Women’s Health and Aging Studies (Leng et al., 2007).
The biological and physiological features of frailty indicate multisystem involvement with interactions among systems, rather than a single system. Thus a global approach to the assessment and management of problems affecting frail older adults is warranted.
Considerations for assessment
As healthcare clinicians, the assessment measures used should be standardized, evidence-based and psychometrically sound. Researchers and therapists strive to develop and test such clinical tools. Although geriatric assessments used by physical therapists are numerous, there are currently no instruments that are specific for measuring and evaluating frailty, either as screening or outcome tools. Considering the challenges with singularly defining the frailty construct, this is understandable. Nevertheless, the issue is being addressed, as noted below.
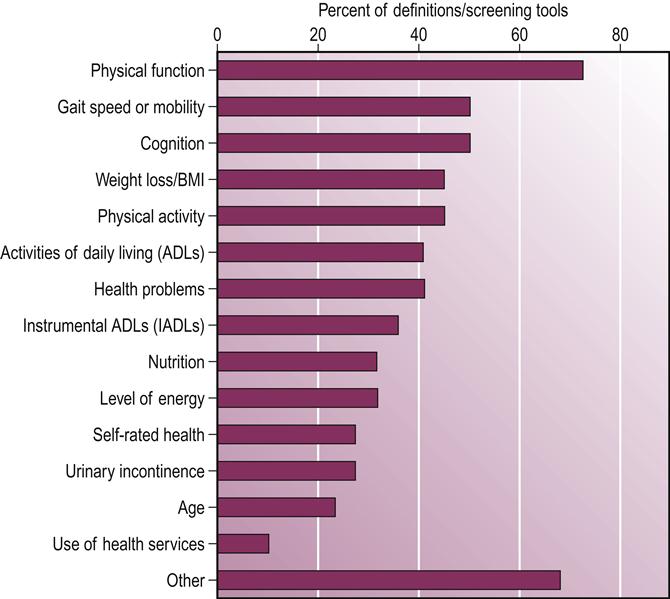
To understand the scope and scale of the issue, a systematic review (SR) investigated the clinical operational definitions of frailty, frailty screening instruments and tools to measure the severity of frailty (Sternberg et al., 2011: 1). Inclusion criteria were studies examining community-dwelling adults aged 65 and older who had clinically relevant outcomes (change in functional status, hospitalization or death), articles describing original tools (not subsequent validation studies) and articles that mentioned frailty rather than simply disability. Results of the SR pertaining to definitions and screening criteria are shown in Figure 65.3. Findings indicate the most commonly identified factors for frailty in definitions and screening tools were physical functioning (73%), gait speed (50%) and cognition (50%). Gait speed and cognition are found more often in recent literature compared to factors of ADLs (41%) and IADLs (instrumental activities of daily living) (36%) in earlier studies. These findings can direct the clinician in the absence of a specific frailty instrument by using the identifying factors as a guide to select which standardized assessment tools address the problem areas.
Subsequent to determining the best assessment instrument, establishing the extent of the frail condition will be a key component of the patient’s profile at baseline. One way to accomplish this is by stratification using levels of frailty. An FI was operationalized by Jones et al. (2004) with three levels of frailty including mild, moderate or severe. To determine the FI, a standard Comprehensive Geriatric Assessment (CGA) representing impairment, disability and comorbidity burden was scored and summed, thus becoming the FI-CGA levels. The three levels of frailty are: mild (FI-CGA 0–7), moderate (FI-CGA 7–13) and severe (FI-CGA>13) (Jones et al., 2004). Information on the extent of the frail condition will benefit the clinician in establishing targeted outcomes besides gaining a more robust composite of the impact on future health.
Beyond the patient’s status at baseline, monitoring changes in the frail condition will provide necessary information for planning interventions and realistic outcomes. The Clinical Global Impression of Change in Physical Frailty (CGIC-PF) tool is used to evaluate changes in physical frailty (Studenski et al., 2004). The CGIC-PF measures six domains (mobility, healthcare utilization, appearance, self-perceived health, ADL, emotional status and social status). This tool also captures the multidimensional nature of frailty.
A final assessment consideration is the potential predictive capacity of some assessment tools. In one study, three criteria (gait speed, grip strength and repeated chair stands) were added to the original five criteria used by Fried and Rockwood. All three criteria were predictive for identifying frailty, with gait speed being the best indicator of multidimensionality frailty. Adults who walked slower than 0.65 m/s were>20 times as likely to be frail compared to those who walked faster. Individuals with grip strength<25 kg were six times more likely to be frail. When rising from seated position<7 times per 30 seconds people were 14 times more likely to be frail. These three single-item criteria predicted mortality at 6 months, with walking speed as the best predictor for adverse outcomes like mortality, hospitalization or disability (Abellan van Kan et al., 2008).
Therapeutic interventions with frail elders
In 2006, an international consensus report described frail older persons as having impairments in balance, mobility, strength, cognition, motor processing, nutrition, endurance (fatigue) and physical activity (Ferrucci et al., 2004). Most of these areas are routinely addressed in physical therapy interventions. Physical activity or regular exercise training can favorably impact several of the frailty criteria, such as muscular weakness, low physical activity, exercise intolerance and slowed motor performance. Confirmation of the benefits of low levels of physical activity, defined as walking at least a mile a week, decreased the risk of developing ADL/IADL impairments as evidenced in the Longitudinal Study of Aging after adjusting for age, gender, comorbidities and baseline disability. These findings provided evidence that engagement in at least low levels of physical activity can slow the progression of ADL and IADL disability (Miller et al., 2000). Additional studies addressing the effects of exercise on non-disease-specific characteristics of frailty suggest the potential for reversal of these traits (Fiatarone et al., 1994; Faber et al., 2006).
Physical activity pertaining to age-related declines in physical function is associated with decrease in measures of exercise tolerance including muscle strength, maximal aerobic capacity and fatigue levels (Walston et al., 2006). However, the idea of endurance/aerobic training for the frail older adult can be unnerving to many clinicians who are not familiar with exercise tolerance capacity in the frail older adult. A more thorough understanding of the impact of aerobic exercise on frailty may alleviate this concern.
Aerobic exercise can alter the frailty phenotype via two mechanisms: increase muscle mass and improvement in maximal oxygen uptake (VO2 peak). The maximum rate of oxygen consumption during vigorous exercise (VO2 peak) is related to exercise tolerance and submaximal exercise capacity (Liu & Fielding, 2011). In one intervention study, a 9-month program of walking and strength training in frail men and women increased endurance by improving VO2 by 14% during peak effort of cardiac output measurements in response to training; the goal was 78% of peak heart rate (Ehsani et al., 2003). Another study demonstrated improved maximal aerobic capacity by 30% among seven healthy elderly (71±2 year) sedentary women after a 12 week regimen of cycle ergometer training (Harber et al., 2009). This study also found an increase in quadriceps muscle mass by 12% with endurance training. In previous studies it had been shown that aerobic exercise did not change muscle size in older adults; however, the percentage of muscle mass in the extremities did increase with aerobic training compared to sedentary older persons (Sugawara et al., 2002).
The effectiveness of progressive resistance strength training in older adults is well documented (Latham et al., 2004: 199). Even into the ninth decade, the reversibility of muscle weakness through strength training has been documented. In an 8-week program of high intensity resistance training, 10 frail, institutionalized adults aged 90±1 year participated in a training program that was adapted from standard rehabilitation principles of progressive resistance training including concentric (lifting) and eccentric (lowering) muscle contractions. At 8 weeks the average strength gain was 174%±31% (P<0.0001) from baseline. Improvements in functional mobility accompanied strength gains (Fiatarone et al., 1990). Considering the major level of frailty often seen among nursing home residents, the efficacy of resistance training in this population is especially encouraging, and is a viable option in treatment planning. Beneficial effects of exercise for frail, institutionalized older adults were also confirmed in a systematic review of institutionalized older adults aged 70 years and older (Weening-Dijksterhuis et al., 2011). In this review, authors took a comprehensive approach to address several outcome measures simultaneously, thus although the benefits in muscle strength from progressive resistance training were identified, the training effects based on exercise specificity was less evident. In contrast, a single-blinded randomized controlled trial (RCT) of 22 institutionalized older adults (mean age, 81.5 years) studied the dose–response effect of a free-weight resistance program comparing two intensity training levels on knee extensor muscles (Seynnes et al., 2004: 202). The high-intensity group (n=8) trained at 80% of their 1-repetition maximum (RM) and the low intensity group trained at 40%. Results demonstrated significant improvements in the high-intensity strength training group (80% of 1 RM) for knee extensor strengthening, endurance and the 6-minute walking test with a similar trend for chair-rising and stair-climbing, compared to a low-intensity (40% of 1 RM) group. Findings further identified a strong dose–response relationship between strength gains and resistance training intensity as well as between improved strength and functional outcomes. Thus, to optimize functional performance, a high-intensity resistance training (80% of 1 RM) is preferable. With a free weight-based program that is supervised, this form of higher-intensity resistance training appears to be as safe as lower-intensity training, although it is more effective functionally and physiologically than lower intensity for frail older adults.
Added benefits in areas of motor performance, secondary to resistance training, have been identified. Walking speed improved among healthy and frail elders after resistance training as reported in 14 studies. Also, an increase in distances in the 6-minute walk test were found in six trials in this same systematic review (Latham et al., 2004). Improvements in gait speed specifically among frail older persons living in nursing homes and the community were also seen after 10 weeks of resistance training (Fiatarone et al., 1994; Chandler et al., 1998). Benefits of resistance training for frail older persons are well founded and can contribute to favorable treatment expectations.
Exercise interventions for frail older persons have shown similar benefits with reduction of fall risk. A single fall is known to increase three-fold the chance of nursing home placement, after adjusting for social, cognitive, psychological, functional and medical factors (Tinetti & Williams, 1997). However, the risk of falls was decreased by 57% from baseline after resistance training for 25 weeks in a study of older women aged 75–85 years with low bone mass (Liu-Ambrose et al., 2004).
In addition to the motoric effects of exercise interventions, underlying mechanisms at the cellular level can potentially be affected by exercises. One such mechanism is the immunologic response, which declines with age-related changes in the thymus gland and T cells (Gruver et al., 2007). This was examined in a RCT of frail older nursing home residents where an intervention of functionally oriented endurance and resistance exercise training was provided every 2 hours from 8 am to 4 pm for 5 days a week for 8 months. Results of the study showed no beneficial or detrimental effects on the immune system as measured by changes in lymphocyte subpopulations, activation markers, in vitro proliferation and cytokine activity (Kapasi et al., 2003). In a related study among frail older women, researchers investigated the effects of dehydroepiandrosterone (DHEA) combined with exercise on strength, bone mass and physical function. Participants received 50 mg/d DHEA or a placebo for 6 months; they all received calcium and cholecalciferol. The exercise regimen included was a 90-minute program of gentle exercises with chair aerobics or yoga twice weekly. Results indicated improved lower extremity strength and function in those taking DHEA, although no changes were seen in bone mineral density. Also among those taking DHEA supplement, significant increases were found in all levels of hormones, including estradiol, DHEAS, estrone and testosterone (Kenny et al., 2010).
Another area of major concern with frailty is disability in performing ADLs. In Latham’s systematic review (41 studies), the risk of ADL disability did not decrease with resistance exercise training (Latham et al., 2004). In contrast, the Cochrane Review of 121 trials found an association between resistance training and reduced ADL disability (Liu & Latham, 2009: 254). It is noted that neither of these two reviews were stratified by severity of frailty. In a RCT of a 6-month home program of combined resistance exercises with balance training and home safety and assistive device evaluations, the intervention group classified as moderately frail had a decrease in functional decline over time as per their disability scores. Disability scores in the intervention and control groups were 2.3 and 2.8, respectively, at baseline; 2.0 and 3.6 at 7 months for the comparison between the groups in change from baseline); and 2.7 and 4.2 at 12 months. This change was not observed in the severely frail adults. Moderate frailty was defined as the inability to rise from a chair with arms folded, or the inability to perform a rapid gait test which requires more than 10 seconds to walk a 3 meter course. Severe frailty was defined as lacking both characteristics or abilities (Gill et al., 2002: 80). In a different study, there was no improvement in the Older American Resources and Services (OARS) ADL score in a group of mild to moderately frail persons secondary to a regimen of balance, resistance and flexibility training (Binder et al., 2002). More recently, the FRASI (Frailty Screening and Intervention) RCT addressed the question of preventing ADL disability in non-disabled, frail, older persons screened in primary care (Bandinelli et al., 2006). The study built on previous research showed that supervised exercises improved physical performance in older persons and prevented functional decline in persons who already have mild disability. Whether such a program can prevent new disability in frail older persons is yet to be determined.
Designing exercise programs for frail older persons must be relevant to functional activities, particularly in the presence of limited reserve capacity and increased fatigue. As a result of compromised levels in both areas, task specificity may become paramount in improving function, compared to intensity level of exercises (de Vreede et al., 2007). In frail older persons, increases in strength from participating in task-specific exercises have produced results similar to those of resistance exercises (Bean et al., 2003; de Vreede et al., 2004; Manini et al., 2007). Performance of daily tasks in a safe and energy-efficient manner are at the core of achieving independence in self-directed activities. Decreases in muscle strength impact specific functional tasks in areas of mobility over even and uneven surfaces, transfer skills and upright activities requiring good balance skills. Task-specific interventions to address these areas can include weight-shifting exercises, stepping up and over, reaching, stooping and other multidirectional movement exercises. These can be progressed with increasing loads and/or speed of movement (Avers & Brown, 2009). In the frail older person, task-specific training may supersede resistance training alone for improved functional gains (de Vreede et al., 2004).
Special considerations
Community-dwelling older persons
Characteristics related to community-dwelling status may potentially impact the risk of developing frailty. In a longitudinal study of 2069 Mexican American adults, factors including access to healthcare, cognitive functioning and neighborhood characteristics had a protective effect with regards to rates of frailty for adults 75+years of age (Aranda et al., 2011). In contrast, findings of a systematic review have confirmed the positive impact of resistance strengthening exercise programs, revealing gains in muscle strength and walking speed (Latham et al., 2004), improved balance and reduction in falls (Bulat et al., 2007), and increased bone mineral density (Layne & Nelson, 1999). In one longitudinal study, physical activity modified the effect of disability on depression in older adults (Lee & Park, 2008).
Results of studies focusing exercise programs among community-dwelling frail older persons have varied findings, possibly secondary to different levels of frailty. In one RCT, participants with moderate frailty benefited from a 6-month intervention of home-based physical therapy with less functional decline at 12 months. Focus of the intervention was on underlying impairments including balance, muscle strength, transfers and mobility. Similar results were not seen in those with severe frailty (Gill et al., 2002). In another RCT of elderly persons after hospital discharge, there was no effect on rehabilitation outcomes of physical performance after receiving a vitamin D supplementation and a home-based high-intensity quadriceps resistance exercise program (Latham et al., 2003). In regards to this study, it is noted that participants were recently ill, and the authors did generalize findings to the wider population of frail persons based on the study design and the broad characteristics of patients who were recruited for the study. Further research is needed on the impact of levels of frailty on efficacy of interventions.
A cohort study of community-dwelling older adults in the Canadian Study of Health and Aging involved 36 centers (Hubbard et al., 2009) and used a Frailty Index based on 40 variables representing a range of health conditions and disabilities to capture the gradations in health status. Results indicated that persons who participated in high levels of physical activity had a lower risk of death compared to non-exercisers or those who did minimal exercise. Also, the death rates for men and women over 75 years who did exercise were comparable to their peers aged 65–75 who did not exercise. After adjusting for age and sex, there was a greater chance for improving health status in the exercisers compared to non-exercisers. And interestingly, the greatest impact on health status was among those who were the most frail at baseline. The authors noted that they used the definition of frailty based on the Frailty Index (deficit count) rather than the phenotypic definition. They further noted that these results are not applicable to nursing home or residential clients, or those with significant cognitive impairments. Benefits derived were extended to those with a higher number of health deficits at baseline, which offers evidence to support the idea that health prevention in older adults extends longevity in a healthy state.
Frail older person with balance deficits
A large-scale study of the efficacy of targeted and non-targeted exercises on fall risk and fall-related injuries involved RCTs in the multicenter Frailty and Injuries: Cooperative Studies on Intervention Techniques (FICSIT). With consideration of the variations among interventions with respect to type of exercise, intensity, frequency and duration, the combined multisite outcomes showed a significant decrease (13%) in fall risk for those individuals who engaged in interventions that had exercise as a core component. The risk was further reduced (by 24%) if the exercise intervention included specific balance and walking activities (Province et al., 1995). In another RCT, a group of frail homebound women (≥80 years) who were identified as high risk for falls, received an individualized exercise program (Otago home exercise program) 3 times per week for 12 months and included walking 3 times per week. Results included a significant reduction in fall rates (about one-third) and injurious falls, and significant improvement in balance at 6 months (Campbell & Buchner, 1997).
Tai chi has been shown to lower the risk of multiple falls by 47.5% among certain groups of older adults (Wolf et al., 1996; Li et al., 2005; Voukelatos et al., 2007). An Eastern form of exercise, tai chi also provides numerous health benefits in functional balance, physical performance and reduced fear of falling. In contrast, a 48-week intervention program of intense tai chi did not significantly reduce the risk of falls in a group of older adults (70–97 years) who were classified as frail or becoming frail (Wolf et al., 2003). However, as the researchers have noted, the imprecise definition of transitional frailty used in the study may have contributed to lack of significance. Therefore, the therapist’s clinical judgment will still be driven by the patient s’ presenting problems, which can range from minimal debility to complex polypharmacy considerations. Tai chi as a stand-alone strategy may be less effective than a multifactorial intervention that combines other traditional clinical approaches in the reduction of fall risk. Given the multifactorial nature of frailty, besides the number of contributing factors to a heightened fall risk, a thorough analysis of all factors involved will be critical to the development of a well-rounded treatment program.
Frailty and incontinence
The older adult population has the highest prevalence of urinary incontinence and is a reflection of the exponential growth of the aging population worldwide. In a report from the 4th International Consultation on Incontinence, the clinical phenotype used to address frailty included impairments in physical activity, mobility, balance, muscle strength, motor processing, cognition, nutrition and endurance (DuBeau et al., 2010). This report further identified associations that contribute to urinary incontinence with other factors besides age-related changes in muscular, hormonal and structural features. They included comorbidities and impairments (dementia, falls, decreased vision and hearing, dizziness), neurological and psychiatric disorders, and/or medications as important factors associated with urinary incontinence. The overall impact of incontinence frequently involves functional decline secondary to decreased mobility and becoming socially isolated from a fear of urinary accidents in public. Identification of this issue early in the assessment process is critical to planning interventions and outcomes.
Studies have also shown an association between an increased risk of urinary incontinence with ADL and physical performance functional limitations (Cigolle et al., 2007; Huang et al., 2007). For an extensive summary of evidence regarding treatment and management of urinary incontinence, the reader is referred to the 4th International Consultation Report (DuBeau et al., 2010).
Frailty and Parkinson’s disease
Few research studies are available on frailty and Parkinson’s disease (PD). One study does shed light on the prevalence of PD and its relationship to individual frailty criteria and the level of severity of PD (Ahmed et al., 2008). In an observational, cross-sectional analysis of adults with PD, disease severity was measured using the unified Parkinson’s disease rating scale (UPDRS). This assessment tool is divided into three sections: the first section addresses mood and intellectual functioning; the second section evaluates a person’s daily functioning (rolling in bed, showering and writing); the third looks at motor ability. Higher scores indicate more severe disease, with results reported on a 0–199 scale. To diagnose frailty, the five components of Fried were used (walking speed, exhaustion, grip strength, weekly caloric expenditure and weight loss). Three or more of the five criteria confirmed frailty. Average age of the population was 70.8±9.2 years. Results of the study indicated that the prevalence of frailty in adults with optimally treated PD was higher than expected (32.6%). The best discriminator between those who met the frailty criteria and those who did not was weekly caloric expenditure. The number of criteria that were positive for frailty increased with the severity of the disease. Also, there was a direct relationship between walk time and the severity of the disease. UPDRS scores ranged from 11 to 75 with the mean score of 35.8±15.0. These scores in combination with the high prevalence (nearly five times higher than the general population) emphasize the importance of proper diagnosis and treatment of frailty in people with PD.
Frailty and chronic diseases
Chronic diseases in the older adult play a major role in their health trajectory in later life. There is less time spent in the frail state compared to being disabled because of the higher risk of mortality (Thorpe et al., 2009). In the Cardiovascular Health Study (CHS), among those with comorbidities (comorbidity defined as having two or more of the following nine diseases: myocardial infarction, angina, congestive heart failure, claudication, arthritis, cancer, diabetes, hypertension, chronic obstructive pulmonary disease), 46% were also frail (Fried et al., 2001). The diagnosis of Parkinson’s disease was excluded from this study as a condition that could present with frailty characteristics consequential to a single disease. Also in this study, the mean number of comorbid diseases in the frail older adults was approximately 2.1 compared to 1.4 in the non-frail group.
With aging we observed an increased susceptibility to multiple chronic diseases that had no evident ‘usual’ risk factors. The regulatory network of biological signaling that maintains homeostatic equilibrium is involved as it progressively becomes less efficient. Physiologic dysregulation in multiple systems may contribute to the loss of reserves and vulnerability as well as disease manifestations seen in frail older adults (Fried et al., 2009).
In cohort studies of older adults, chronic diseases that have been associated with frailty include (in descending order of prevalence): hypertension, chronic kidney disease, osteoarthritis, depressive symptoms, coronary heart disease, diabetes mellitus, chronic lower respiratory tract disease, myocardial infarction, rheumatoid arthritis, stroke, peripheral arterial disease and congestive heart failure. From among these diseases there was no association identified between a single disease and frailty (Weiss, 2011).
Related to chronic diseases, other common conditions associated with frailty have been identified. A poor nutritional state in the frail older adult (Semba et al., 2006) together with low activity levels suggested an energy dysregulation that is also involved in congestive heart failure, diabetes, stroke and chronic lung disease. Anemia and its potential association with frailty is being studied to understand the synergistic interactions with cardiovascular disease as a risk factor for frailty (Weiss, 2011). Heightened inflammation and changes in the immune system likely are responsible for the overall decline in immunologic function in the frail, older adult (Yao et al., 2011). Lastly, an association has been found between frailty and the risk for venous thromboembolism in community-dwelling older adults with intermediate to definite frailty (Folsom et al., 2007).
The multidimensional nature of frailty provides the basis for impaired function in more than one system (Bandeen-Roche et al., 2006; Inouye et al., 2007). The numerous physiologic subsystems suggest there may be several subtypes of frailty (Fried et al., 2005) with several points of entry into the frailty process, such as advanced chronic disease complicated by malnutrition. Analyses of interactions and relationships among these subsystems may require more complex, non-linear models in research (Weiss, 2011). Also, this multifactorial approach to frailty is reflective of impaired homeostasis in several systems.
Conclusion
As definitions of frailty have evolved, so have the multiple factors for consideration when assessing and treating the frail older adult. The variability of the multidimensional nature of frailty is well documented. Along that line, knowledge of the cluster of signs and symptoms for early identification of frail or pre-frail status will be paramount in developing appropriate therapeutic interventions. With evidence from the research identifying the benefits of strengthening programs even for the oldest-old, therapists can confidently intervene and expect positive outcomes. The key will be to capture all aspects of frailty at baseline, then apply evidence-based principles of practice. Future studies will direct the way for more specific tools as the older population continues to grow worldwide.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree