3 Fractures of the Ulna and Radius
Overview
 Anatomic Features
Anatomic Features
The ulna and radius are the bony structures of the forearm that form the elbow joint proximally with the humerus and the wrist joint distally with the carpals. The radius and ulna are joined by the proximal and distal radioulnar joints and by the interosseous membrane (IOM). The radioulnar joints are pivot joints where movements of supination and pronation take place. If one bone shows a fracture with displacement or angulation, usually the other bone will also have a fracture or displacement. Both the radius and ulna are long bones, prismatic in form, and lie roughly parallel to each other when the forearm is supinated. The ulna is relatively straight, while the radius is slightly curved longitudinally (Plate 3.1).
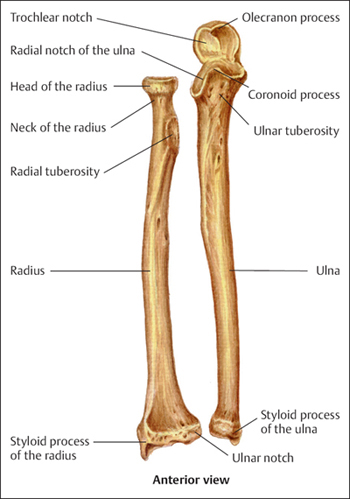
Plate 3.1
 AO Classification and Coding System for Fractures of the Ulna and Radius
AO Classification and Coding System for Fractures of the Ulna and Radius
Based on the AO classification, the ulna/radius should be considered as one unit of bone, with the location coding number “2.” The anatomic delineation of the segments, proximal, shaft, and distal is performed according to the “Heim’s Square,” with assigned numbers of “21, 22, and 23” respectively (Plates 3.2 and 3.3).
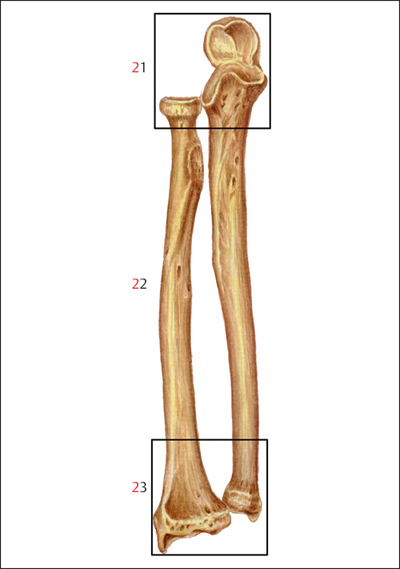
Plate 3.2
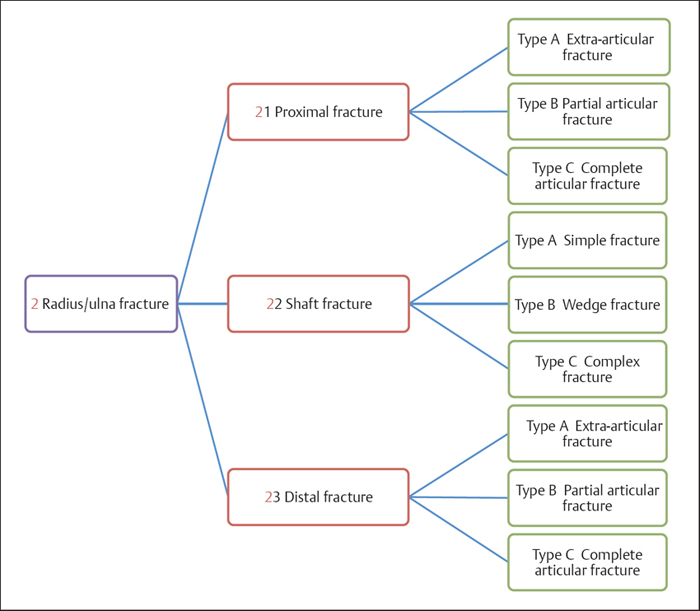
Plate 3.3
 Clinical Epidemiologic Features of Radius/Ulna Fractures
Clinical Epidemiologic Features of Radius/Ulna Fractures
A total of 9961 patients with 10191 radius/ulna fractures were treated at our trauma center over a 5-year period from 2003 to 2007. All cases were reviewed and statistically studied; the fractures accounted for 16.53% of all patients with fractures and 15.61% of all types of fractures, respectively. Among these 9961 patients, 2845 were children with 2884 fractures, and 7116 were adults with 7307 fractures.
Epidemiologic features of radius/ulna fractures are as follows:
• more males than females
• more left sides involved than right sides
• the highest-risk age group is 11–20 years. The most affected female age group includes ages 51–60 years, while males between the ages of 11 and 20 years have the highest risk
• distal fracture of the radius/ulna is the most common forearm fracture.
 Radius/Ulna Fractures by Sex
Radius/Ulna Fractures by Sex
Table 3.1 Sex distribution of 9961 patients with radius/ulna fractures
| Sex | Number of patients | Percentage |
| Male | 6071 | 60.95 |
| Female | 3890 | 39.05 |
| Total | 9961 | 100.00 |
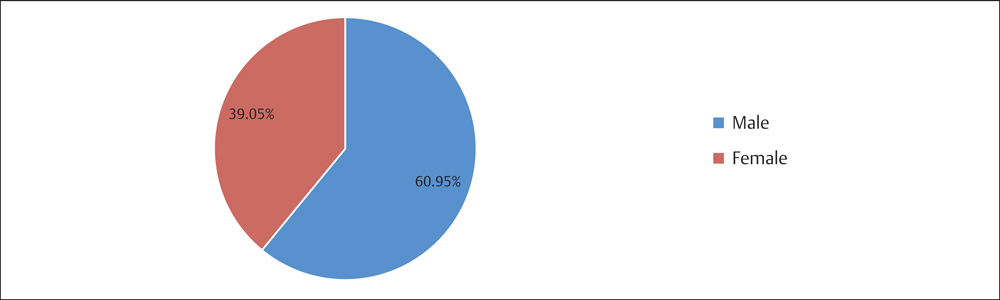
Fig. 3.1 Sex distribution of 9961 patients with radius/ulna fractures.
 Radius/Ulna Fractures by Injured Side
Radius/Ulna Fractures by Injured Side
Table 3.2 Injury side distribution of 9961 patients with radius/ulna fractures
| Injury side | Number of patients | Percentage |
| Left | 5376 | 53.97 |
| Right | 4488 | 45.06 |
| Bilateral | 97 | 0.97 |
| Total | 9961 | 100.00 |
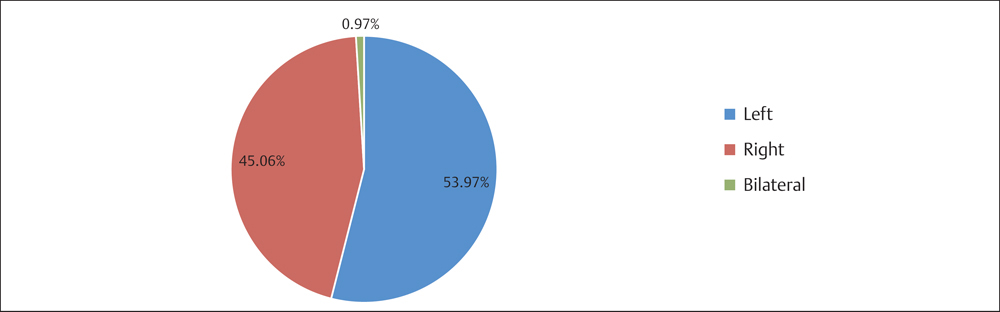
Fig. 3.2 Injury side distribution of 9961 patients with radius/ulna fractures.
 Radius/Ulna fractures by Age Group
Radius/Ulna fractures by Age Group
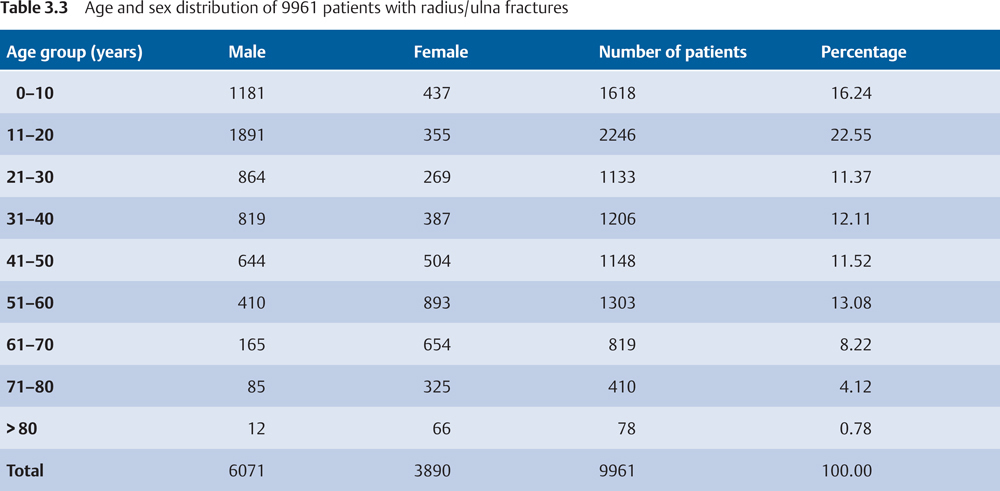
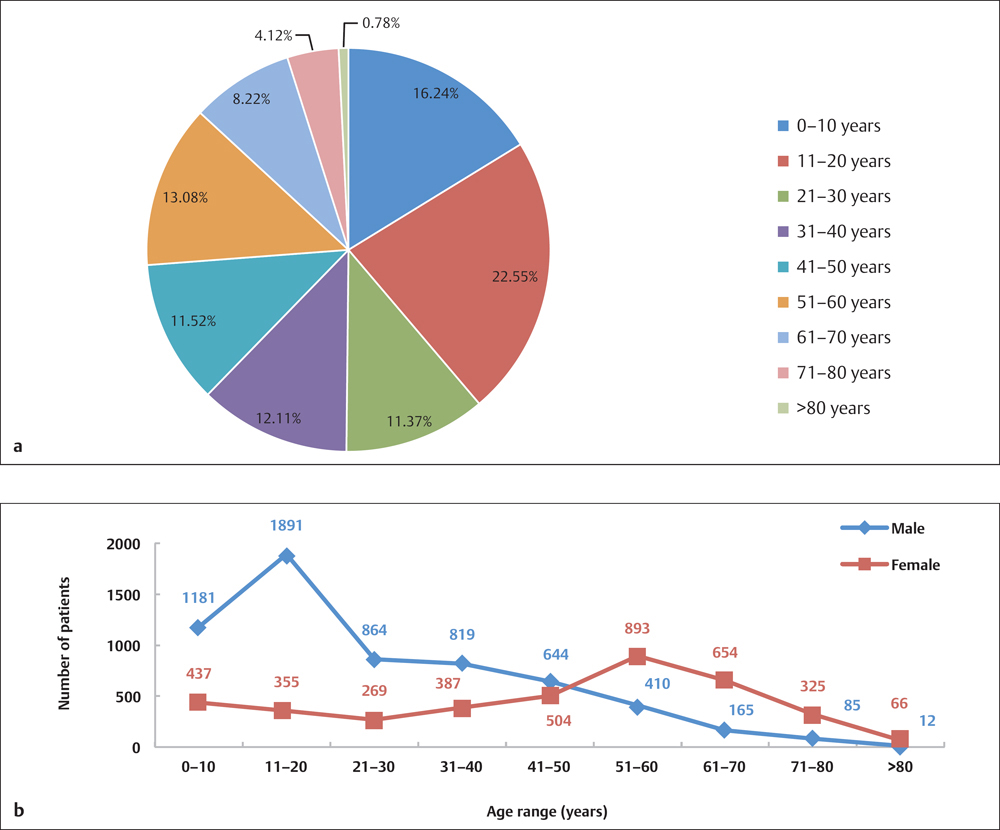
Fig. 3.3 a, b
a Age distribution of 9961 patients with radius/ulna fractures.
b Age and sex distribution of 9961 patients with radius/ulna fractures.
 Radius/Ulna Fractures by Location
Radius/Ulna Fractures by Location
 Radius/Ulna Fractures in Adults by Segment Based on AO Classification
Radius/Ulna Fractures in Adults by Segment Based on AO Classification
Table 3.4 Segment distribution of 7307 radius/ulna fractures in adults based on AO classification
| Segment | Number of fractures | Percentage |
| 21 | 973 | 13.32 |
| 22 | 1703 | 23.31 |
| 23 | 4631 | 63.38 |
| Total | 7307 | 100.00 |
Fig. 3.4 Segment distribution of 7307 radius/ulna fractures in adults based on AO classification.
 Radius/Ulna Fractures in Children by Segment
Radius/Ulna Fractures in Children by Segment
Table 3.5 Segment distribution of 2884 radius/ulna fractures in children
| Segment | Number of fractures | Percentage |
| Proximal | 458 | 15.88 |
| Diaphysis | 1152 | 39.94 |
| Distal | 1274 | 44.17 |
| Total | 2884 | 100.00 |

Fig. 3.5 Segment distribution of 2884 radius/ulna fractures in children.
Proximal Radius/Ulna Fractures (Segment 21)
 Anatomic Features
Anatomic Features
The bony structures of the proximal part of the radius/ulna consist of the olecranon, coronoid process, radial head, radial neck, and part of the metaphysis. The bony surfaces of the humeroradial joint constitute an enarthrosis or ball and socket joint, between the radial head and the capitulum of the humerus, while the proximal radioulnar joint is a trochoid or pivot joint between the radial head and the ring formed by the radial notch of the ulna and the annular ligament. These two joints play an important role in the complex action of turning the forearm over as in pronation or supination. The humeroradial joint is considered similar to a lateral column that provides stability to the elbow joint during its motion in flexion or extension.
The articular surfaces of the elbow joint are connected by a capsule that is attached to the radial neck, 1.5 cm distal to the humeroradial joint. The radial tuberosity, also known as the bicipital tuberosity, is the main insertion of the biceps brachii muscle.
The olecranon and the coronoid process form a large depression called the semilunar notch that serves as an articulation site with the trochlea of the humerus. The humeroulnar joint is a simple hinge joint that allows for flexion and extension. The tendon of the triceps brachii muscle inserts into the posterior portion of the upper surface of the olecranon, while the ulnar nerve winds along the olecranon or epicondylar groove.
Plate 3.4
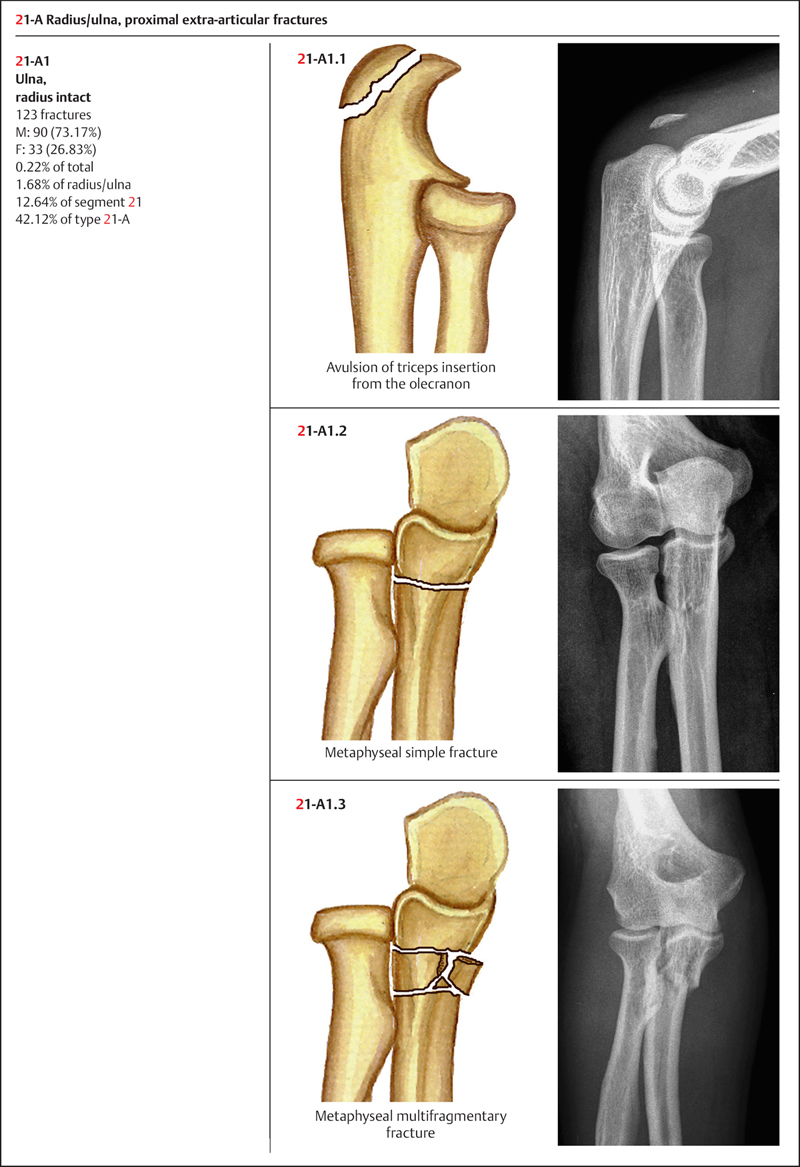
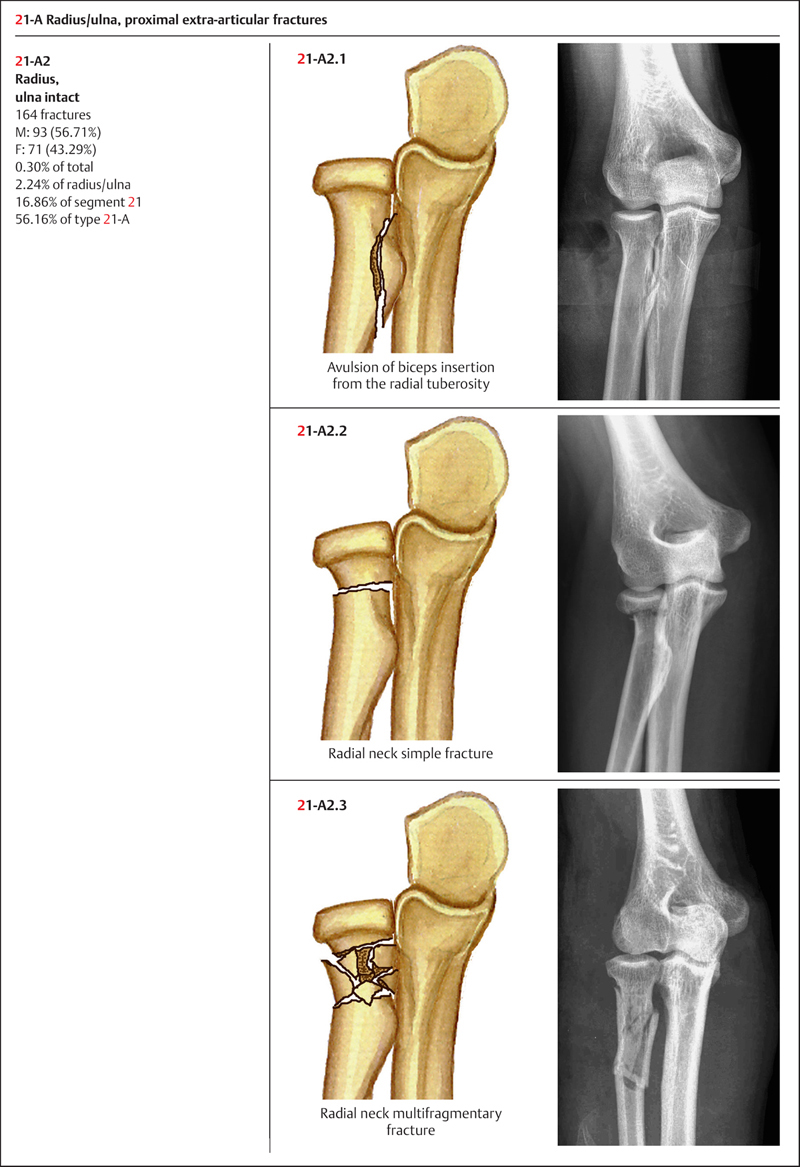
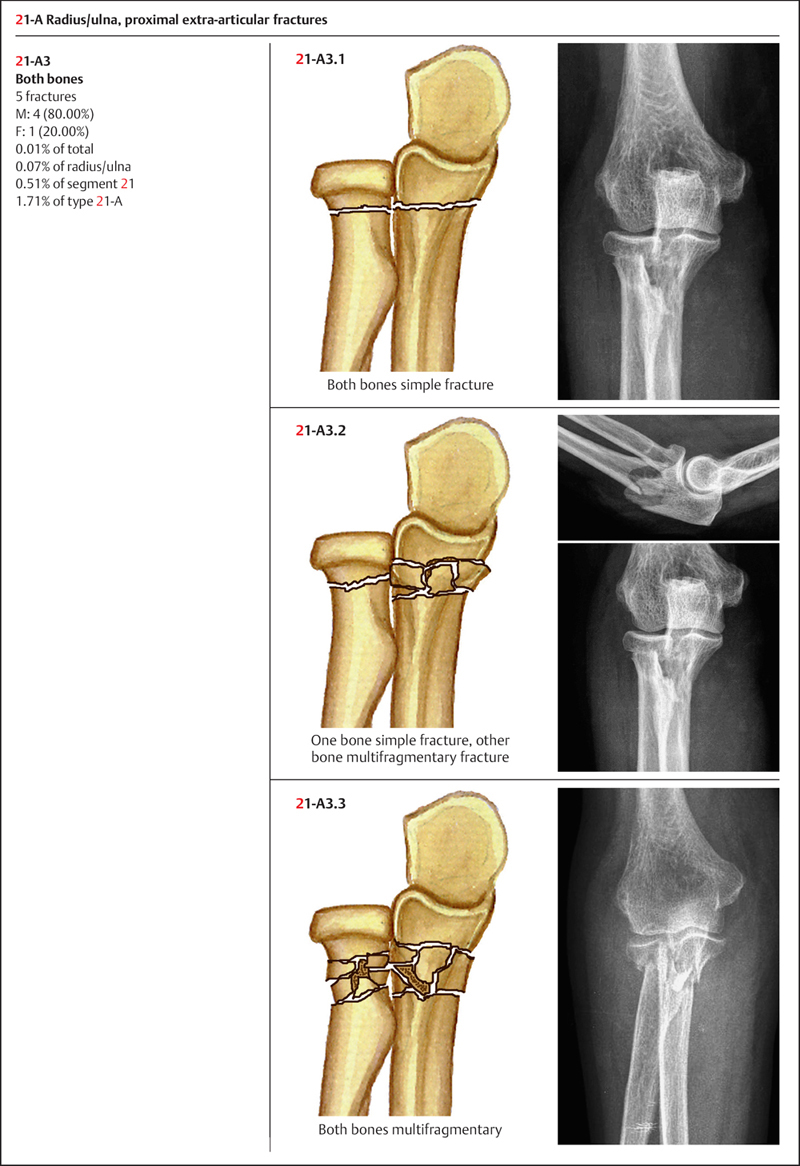
 AO Classification of Proximal Radius/Ulna Fractures
AO Classification of Proximal Radius/Ulna Fractures
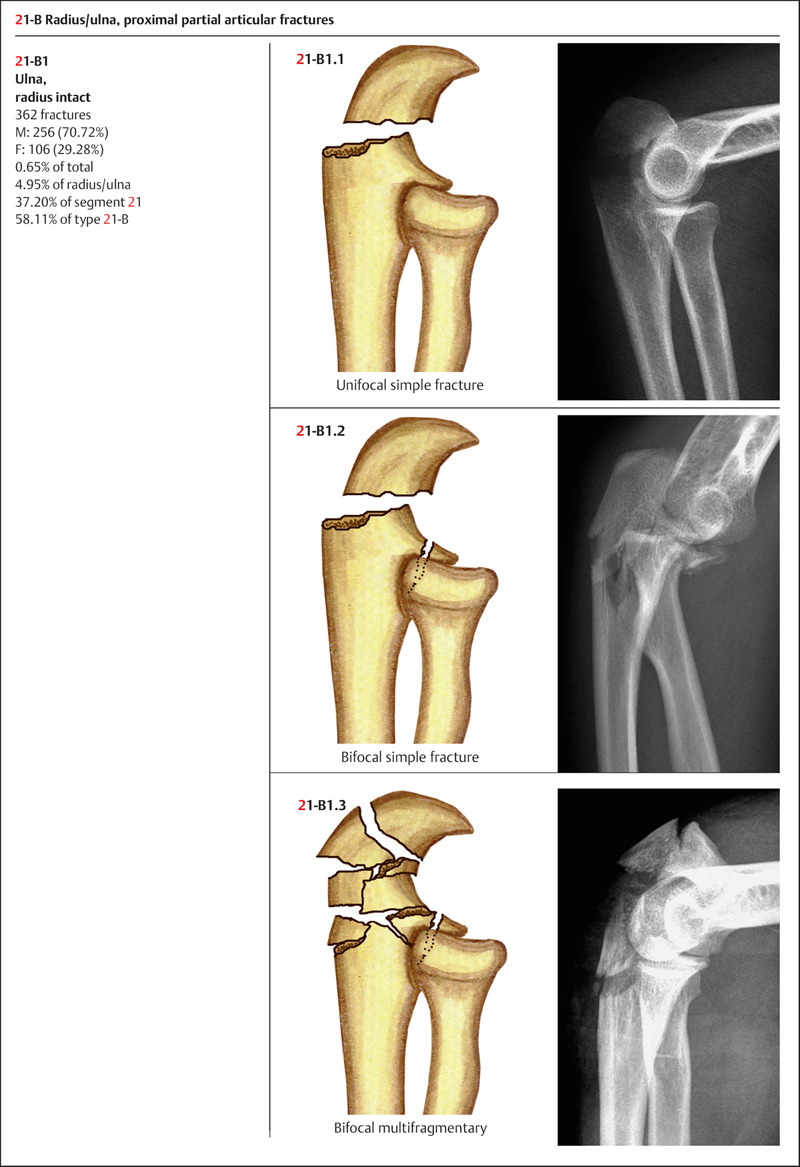
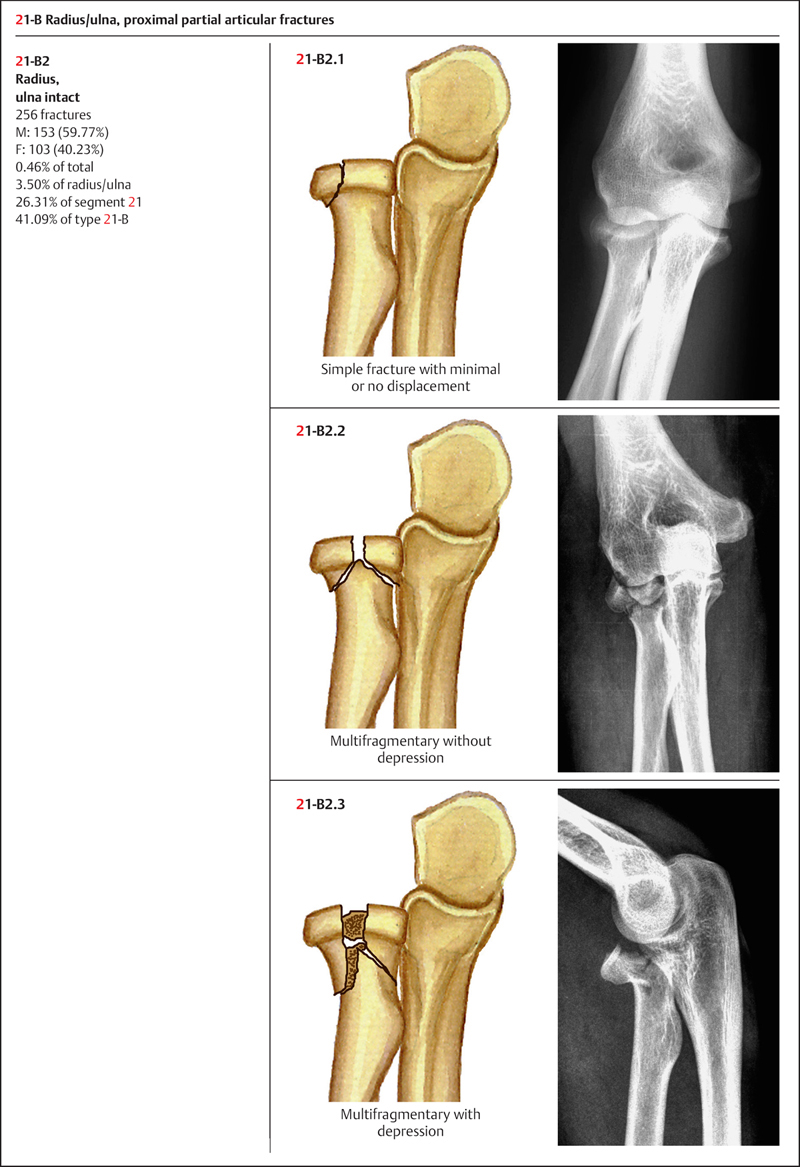
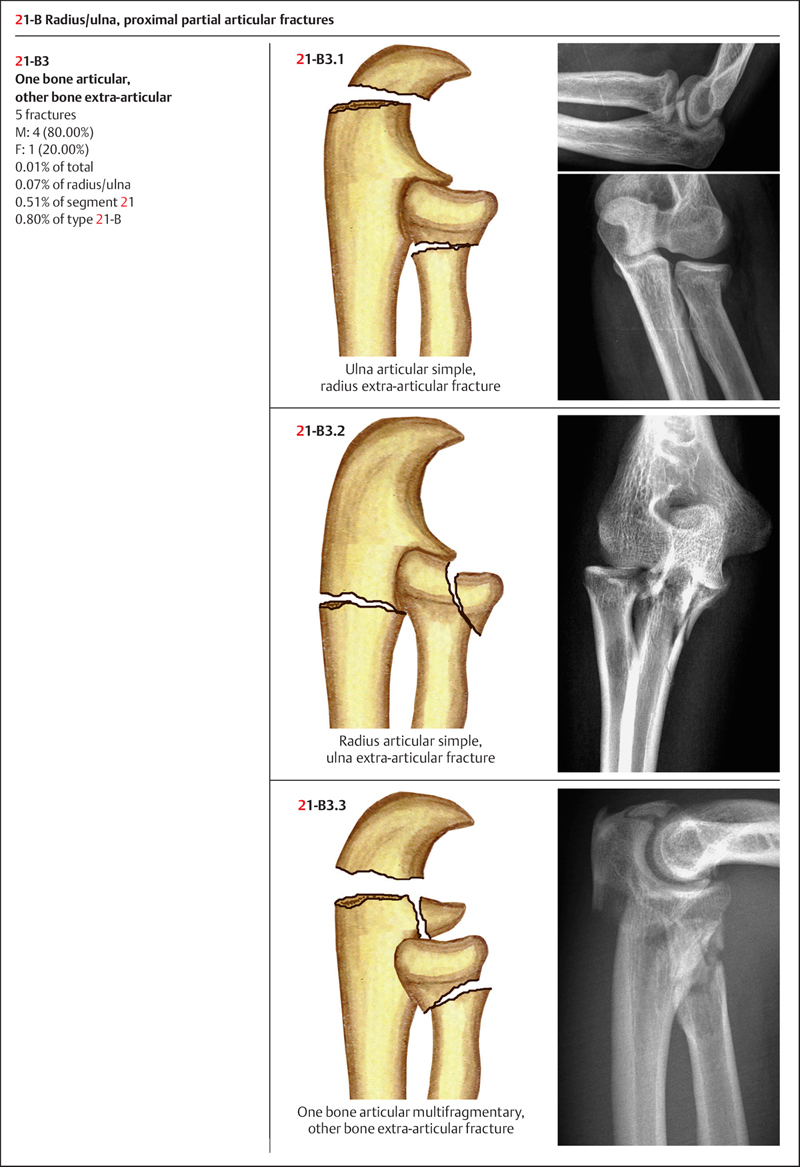
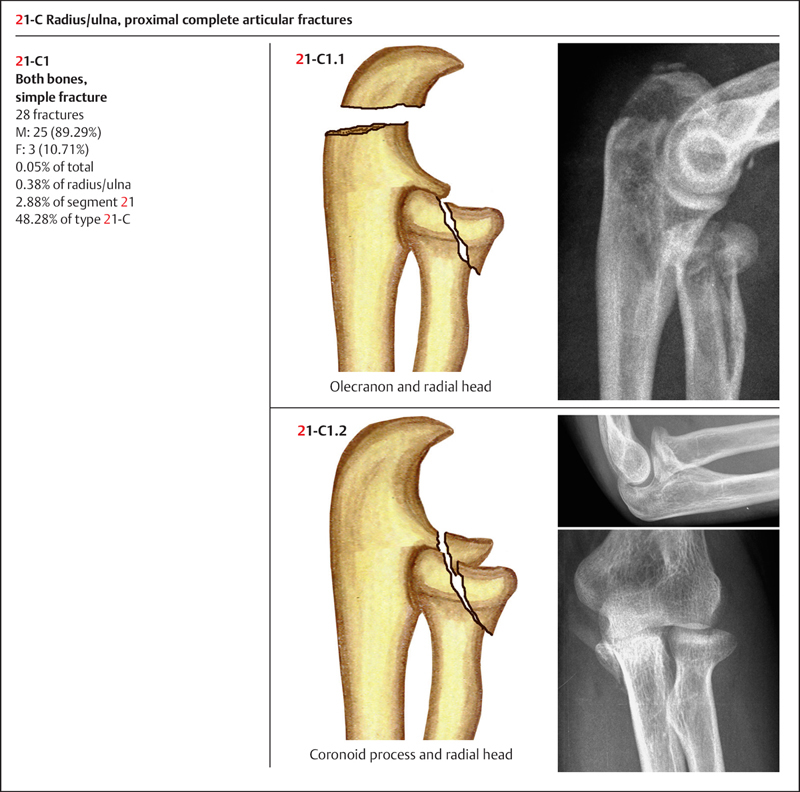
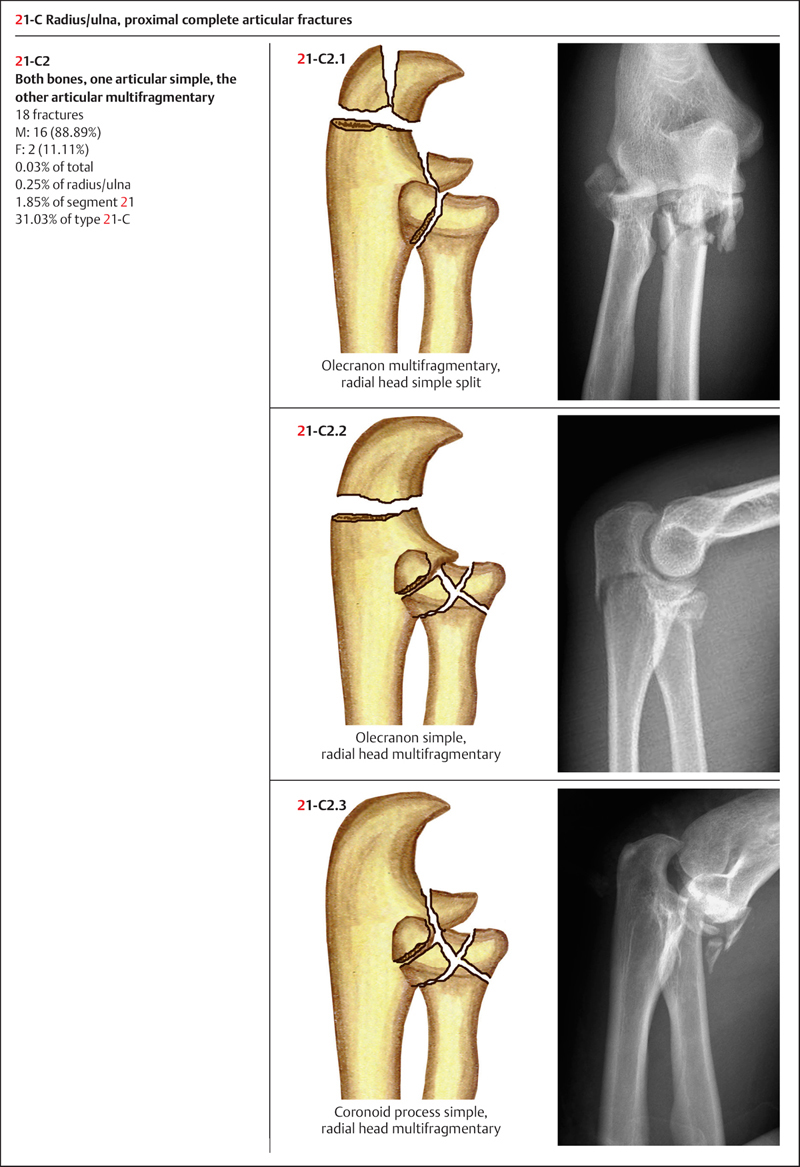
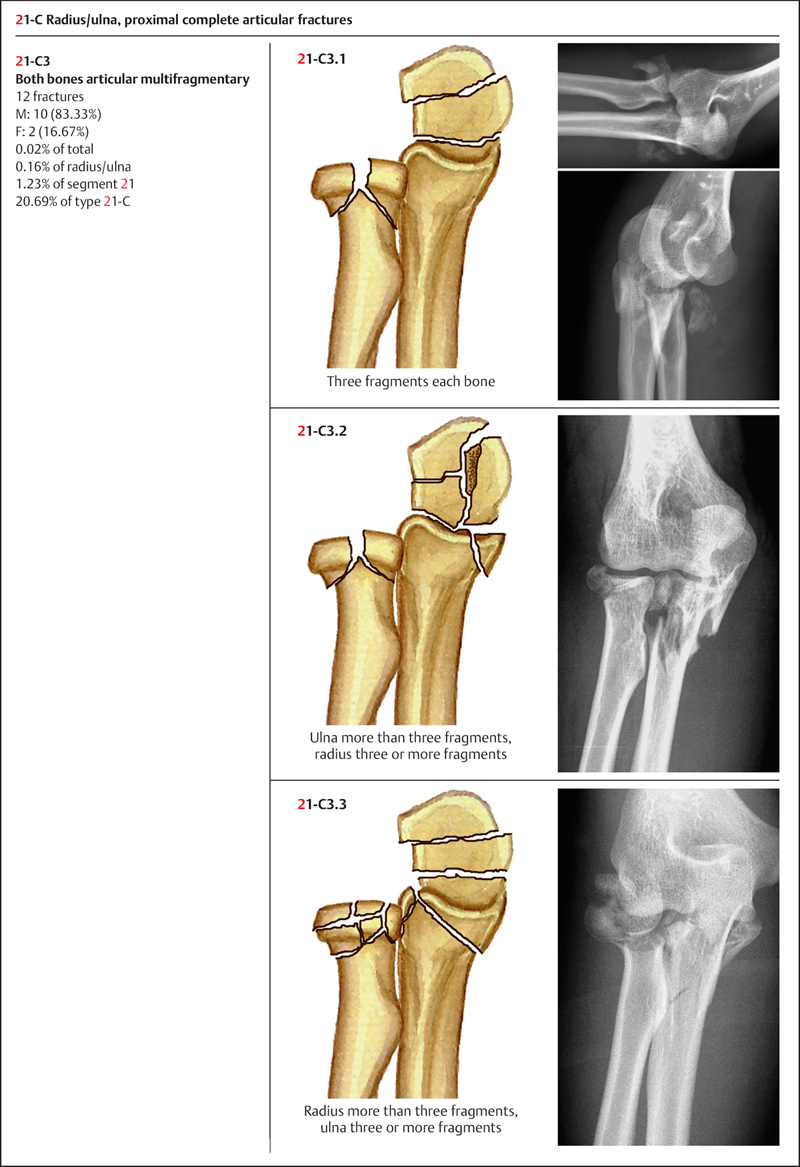
Based on AO classification, the delineation of the proximal radius/ulna is illustrated by a square whose lateral sides are parallel to the axis of the bone and whose length is equal to the maximum width of the epiphysis. According to this formula, the proximal radius/ulna is coded as the number 21 (Plate 3.4). On the basis of articular surface involvement, the radial/ulnar fracture is further divided into three types: 21-A: extra-articular fracture; 21-B: partial articular fracture; and 21-C: complete articular fracture (Plate 3.5).
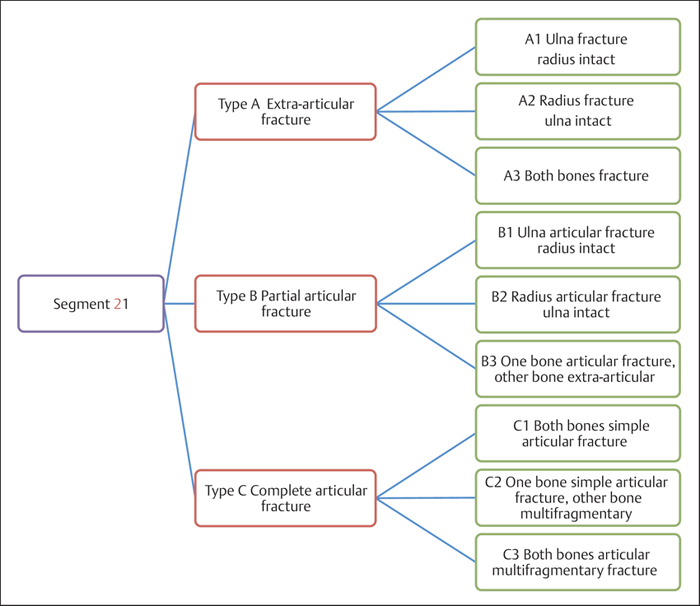
Plate 3.5
 Clinical Epidemiologic Features of Proximal Radius/Ulna Fractures (Segment 21)
Clinical Epidemiologic Features of Proximal Radius/Ulna Fractures (Segment 21)
A total of 973 adult proximal radius/ulna fractures (segment 21) were treated at our trauma center over a 5-year period from 2003 to 2007. All cases were reviewed and statistically studied; the fractures accounted for 13.32% of all fractures of the radius/ulna in adult. Their epidemiologic features are as follows:
• more males than females
• the high-risk age group is 21–40 years—the same age group for both males and females
• the most common fracture type among segment 21 fractures is type 21-B—the same fracture type for both males and females
• the most common fracture group among segment 21 fractures is group 21-B1; group 21-B1 most commonly occurs in males, while groups 21-B1 and B2 are most common in females.
 Fractures of Segment 21 by Sex
Fractures of Segment 21 by Sex
Table 3.6 Sex distribution of 973 fractures of segment 21
| Sex | Number of fractures | Percentage |
| Male | 651 | 66.91 |
| Female | 322 | 33.09 |
| Total | 973 | 100.00 |
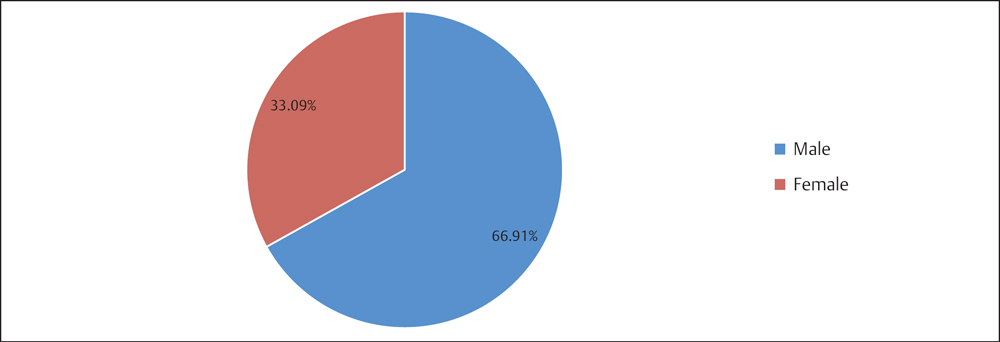
Fig. 3.6 Sex distribution of 973 fractures of segment 21.
 Fractures of Segment 21 by Age Group
Fractures of Segment 21 by Age Group
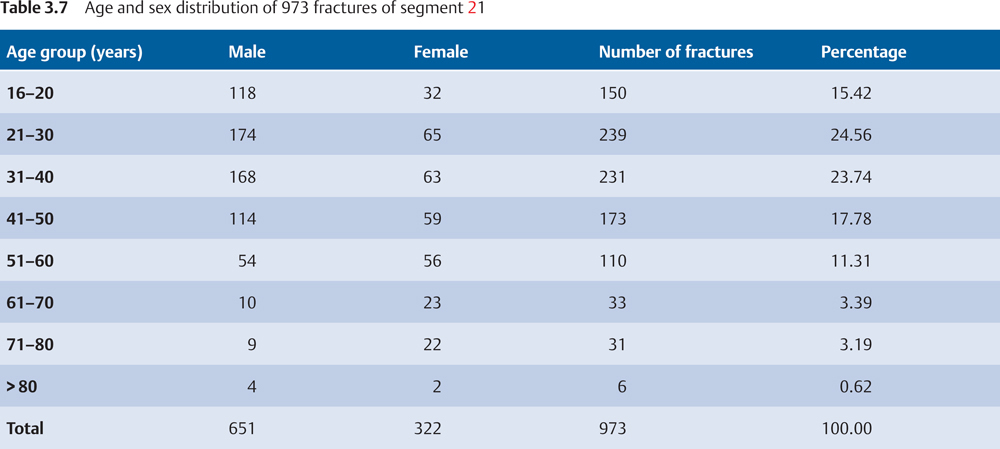
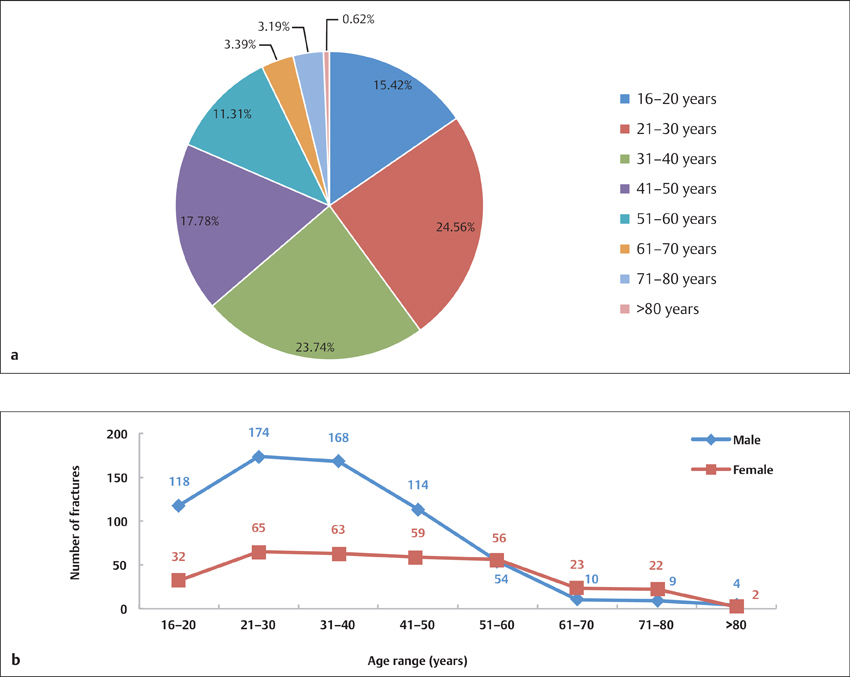
Fig. 3.7 a, b
a Age distribution of 973 fractures of segment 21.
b Age and sex distribution of 973 fractures of segment 21.
 Fractures of Segment 21 by Fracture Type
Fractures of Segment 21 by Fracture Type
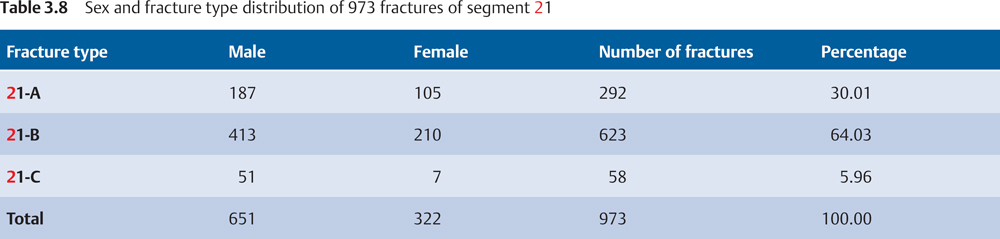
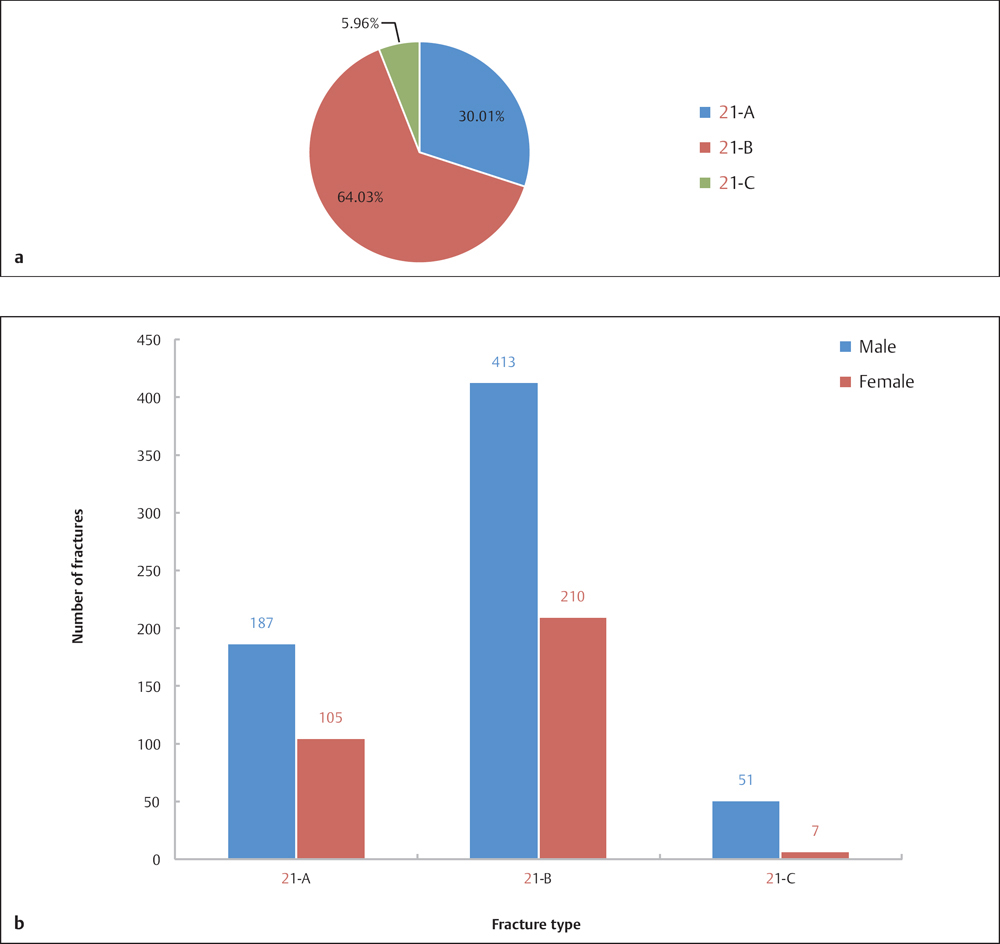
Fig. 3.8 a, b
a Fracture type distribution of 973 fractures of segment 21.
b Sex and fracture type distribution of 973 fractures of segment 21.
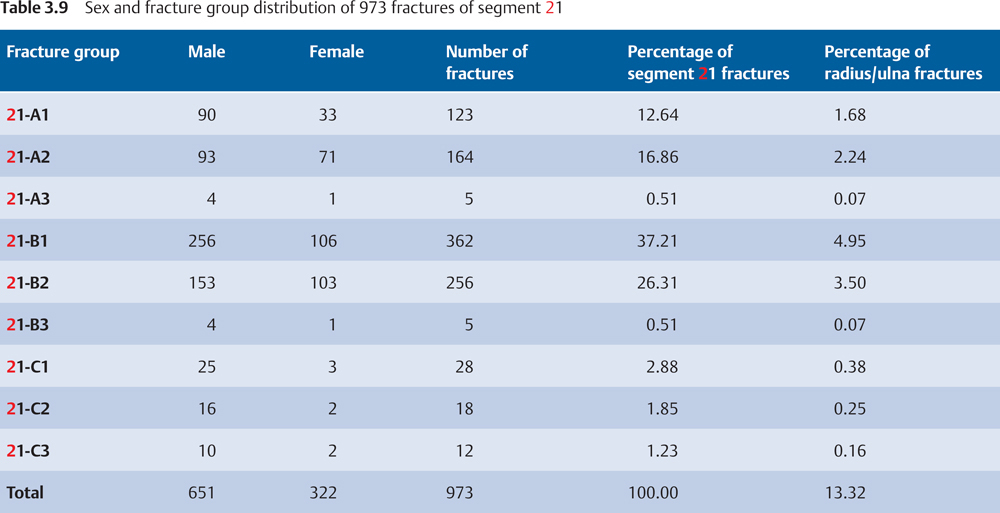
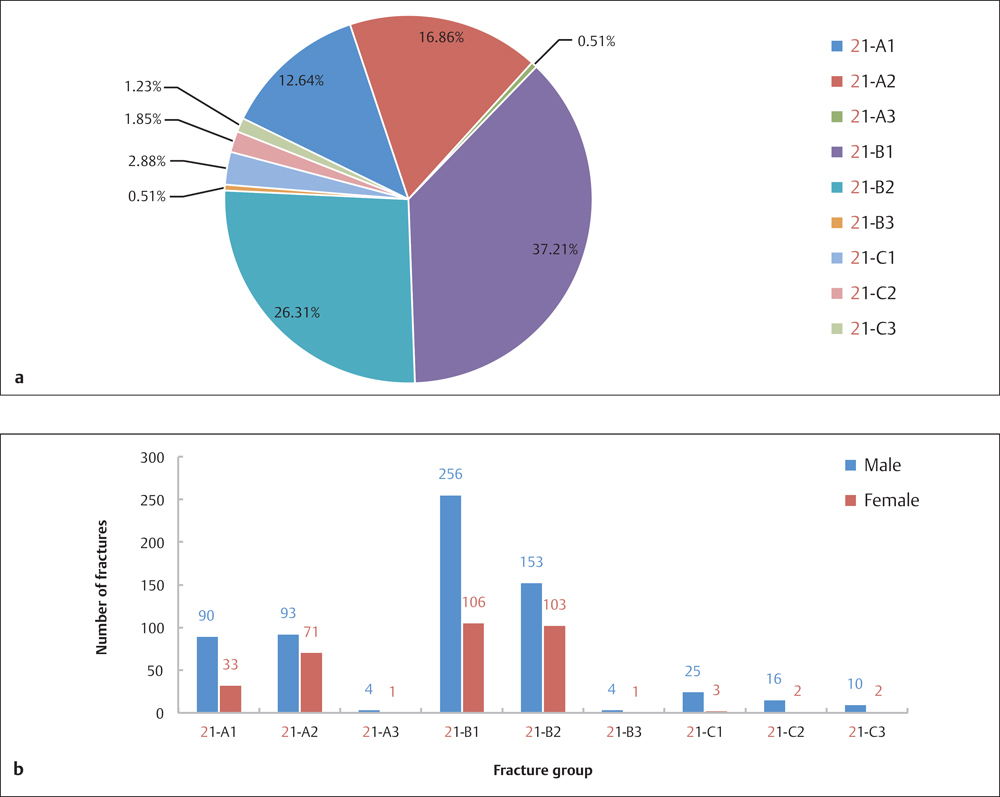
Fig. 3.9 a, b
a Fracture group distribution of 973 fractures of segment 21.
b Sex and fracture group distribution of 973 fractures of segment 21.
 Injury Mechanism
Injury Mechanism
Olecranon Fractures
Olecranon multifragmentary fracture can be caused by direct trauma, as in falls on or blows to the point of the elbow. Such types of fractures also occur during a fall on the semiflexed supinated forearm with the hand striking the ground, and the pull of the triceps muscle leading to a transverse or wedge fracture of the olecranon.
Fractures of the Radial Head or Neck of the Radius
This type of injury is usually from a fall on an outstretched arm with the force of impact transmitted up the hand through the forearm to the radial head, which is forced to the capitellum and often causes fractures in the anterolateral aspect of the radial head or neck of the radius. Multifragmentary fractures or dislocation may occur by high-energy trauma.
Coronoid Fractures
Coronoid fracture, rarely seen in isolation, usually occurs in combination with olecranon fracture; this type of fracture results from an avulsion fracture of the bony structure of the coronoid, by contraction of the joint capsule with the elbow in hyperextension.
 Diagnosis
Diagnosis
The insertion of the triceps muscle on the olecranon is usually compromised when olecranon fractures occur. In most cases, the patient cannot fully strengthen his or her arm due to the pain and is unable to overcome any resistance. The movement of supination aggravates the pain from fractures in the radial head or neck of the radius and limits the range of motion.
The radiographic examination should include anteroposterior (AP) and lateral views of the elbow. If the patient has marked physical signs but inconclusive X-rays, computed tomography (CT) or magnetic resonance imaging (MRI) scans may be required to clarify the nature and extent of the injury. Note that the individual will be unable to fully extend the forearm when taking the AP view of the elbow, so the beam must be placed perpendicularly to the radial head (the left figure shows the correct projection position, while the wrong one commonly seen in practice is shown on the right) (Plate 3.6).
 Treatment
Treatment
Olecranon fractures are unstable fractures, usually requiring surgical intervention. Plate fixation, tension band wiring, and other internal fixators can be utilized in stabilizing the fracture, depending on the fracture type.
Stable fractures of the radial head or the neck of the radius with no displacement can be managed nonsurgically, but with close monitoring of fracture progression within 4 weeks. Minimal invasive internal fixation is preferable for fractures with dislocation or when nonsurgical treatment fails. Based on fracture type, patient age, and general condition, various internal fixators can be selected, including screws, absorbable screws, and Kirschner wires (K-wires). Anatomic reduction to the utmost, rigid fixation, and early mobilization, are applied even for complex fractures. Excision of the radial head and replacement with a prosthesis should be considered only as a last resort.
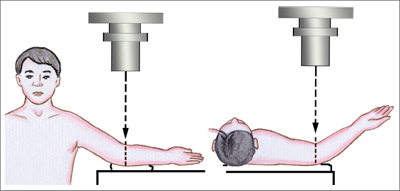
Plate 3.6
Fractures of the Radial/Ulnar Shaft (Segment 22)
 Anatomic Features
Anatomic Features
The ulna is relatively straight, while the radius is slightly curved. In the anatomic position, the width of the space between the ulna and radius is variable, with a maximum width of 1.5–2.0 cm. The IOM, which connects the radius and ulna along their entire length, bears tensile loads with the forearm in a neutral position and is slackened when the forearm is in pronated position. The fibers of the IOM run obliquely upward and lateral from the interosseous crest of the ulna to that of the radius. When one of the bones is fractured, energy is transmitted along the IOM, causing fractures on the other bone in a different plane and a dislocated proximal radioulnar joint. Many muscles are attached to the radius and ulna, with their insertion points spread around their shafts. Consequently, complex fractures with marked displacement usually occur due to contraction of multiple muscles, which makes the reduction very difficult.
 AO Classification of Radial/Ulnar Shaft Fractures
AO Classification of Radial/Ulnar Shaft Fractures
The numeric code for the shaft of the radius and ulna is “22” based on AO classification (Plate 3.7). Fracture of the radial/ulnar shaft is divided into three types: 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








