Fractures of the Lower Extremity
James P. Stannard
Justin N. Duke
Jorge E. Alonso
Lower extremity fractures are often severe injuries that may lead to long-term disability in patients who are involved in trauma. Most orthopaedic traumatologists spend their careers focusing on pelvic and lower extremity trauma. However, understanding these injuries is vitally important to general surgery traumatologists as well. As the “captain of a ship,” it is critical for traumatologists to understand how lower extremity trauma frequently has a major systemic impact. This chapter will initially focus on the management of lower extremity trauma patients when they present to the trauma room. Following that, we will discuss the concepts of damage control orthopaedics, open fractures, gunshot wounds, dislocations, geriatric patients, and heterotopic ossification. Finally, we will briefly discuss various lower extremity skeletal injuries and their appropriate management.
Severe lower extremity trauma is increasingly common as a result of our increasingly mobile society, high-speed driving, and the influence of alcohol, drugs, and firearms. As we become more mobile, the speed and thereby the achieved kinetic energy at which we can injure ourselves keeps pace with the engineering design changes intended to prevent these same injuries. The combination of improved automotive safety features and continued trauma system improvements have led to more patients’ surviving their injuries. It is important to understand the systemic impact of high-energy lower extremity injuries on multiply injured patients, in order to decrease their morbidity and increase the potential function following rehabilitation.
INITIAL PRESENTATION AND PHYSICAL EXAMINATION
Once the Airway, Breathing, and Circulation (ABCs) of resuscitation have been initiated and the extremity examinations are completed, it is time to pay special attention to many details. The history provided by the patient, emergency medical services (EMSs), or other witnesses can be very significant in evaluating the nature and severity of the patient’s skeletal injury. Here, because we are concerned with the lower extremity, facts such as potential environmental contamination become very important. Quantitating the energies associated with the injury can be very useful (see Fig. 1). For example, a young individual who sustains a relatively low-energy accident, such as a fall from standing, with a femoral neck fracture raises our suspicion for an underlying pathologic process. Although this information may seem appropriate for the nonacute treatment phase of care, it illustrates the importance of history when available. The presence of any crush injury is particularly important, especially if there was a prolonged extraction time at the scene of the accident. Rhabdomyelisis and compartment syndrome become much more likely with a crush injury than with other mechanisms of trauma.
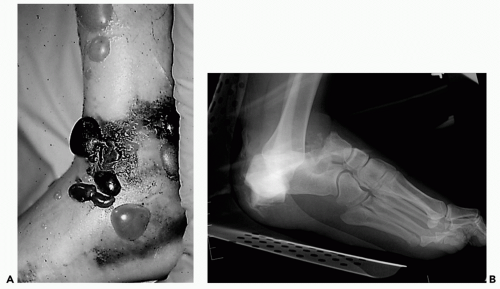
The initial survey of the lower extremity should be concerned with gross deformity, skeletal stability, soft tissue assessment, and the neurovascular status of each limb (see Fig. 2). With an awake and alert patient, these conditions
may be relatively easy to assess, but are more challenging and important in the obtunded and/or mechanically ventilated patient. If at all possible, the orthopaedic service should be consulted as early as possible, preferably during the initial assessment of the patient. This will allow a much more complete extremity neurovascular examination and involve orthopaedic surgery in the overall clinical decisions early in the course of care. Unfortunately, the realities of the care of trauma patients will dictate that patients often require airway management with intubation before evaluation by orthopaedics. Consequently, it is essential that the general surgery trauma team obtain the best baseline neurologic and vascular examination possible. The quality of this examination may dictate the subsequent treatment course of the lower extremity over the initial 48-to 72-hour resuscitation period.
may be relatively easy to assess, but are more challenging and important in the obtunded and/or mechanically ventilated patient. If at all possible, the orthopaedic service should be consulted as early as possible, preferably during the initial assessment of the patient. This will allow a much more complete extremity neurovascular examination and involve orthopaedic surgery in the overall clinical decisions early in the course of care. Unfortunately, the realities of the care of trauma patients will dictate that patients often require airway management with intubation before evaluation by orthopaedics. Consequently, it is essential that the general surgery trauma team obtain the best baseline neurologic and vascular examination possible. The quality of this examination may dictate the subsequent treatment course of the lower extremity over the initial 48-to 72-hour resuscitation period.
Many patients will present with fractures that demonstrate obvious deformity during the secondary survey. Radiographs should be obtained for the area of interest and the joint proximal and distal to the fracture. Unstable long bone should be temporarily stabilized using traction or splinting while a definitive plan for treatment is formulated. Stabilization is important not only for pain control but also to minimize hemorrhage and secondary soft tissue injury, as well as to maintain soft tissues properly.
DAMAGE CONTROL ORTHOPAEDICS
The topic of damage control orthopaedics is currently in evolution and somewhat controversial. It is well established that many patients benefit from early definite stabilization of long bone fractures of the lower extremities. However, the observation that some patients develop systemic complications following skeletal stabilization has led the concept of damage control orthopaedics.1,2 This approach is based on the observation that some patients with multiple systemic injuries may not tolerate, and in fact may be harmed by undergoing early definitive treatment of their fractures. The scenario most frequently studied is that of the polytrauma patient with a femoral fracture3 (see Fig. 3). It has been established that early fixation
reduces many risks of pulmonary complication for many patients; however, the type of fixation is a point of contention. There is concern that a subset of patients, often those with severe thoracic injuries or lung contusions, may not respond well to intramedullary nailing in the acute phase of their resuscitation. The second hit theory states that during the initial treatment course, polytrauma patients develop elevated levels of inflammatory markers and cytokines as part of their systemic response to trauma. Some investigators have expressed concern that performing invasive orthopaedic procedures during the immediate posttrauma period can be associated with an exaggerated inflammatory response that can overwhelm the body and can lead to multiorgan system failure, sepsis, and death. The greatest elevation in the level of inflammatory markers seems to be associated with reamed intramedullary nailing of the femur, although new methods of reaming while irrigating and suctioning moderate these risks.4,5 Consequently, research is under way as to the specifics of this second hit theory, and it remains highly controversial regarding which patients will benefit from early intramedullary stabilization, and those who would benefit from minimizing the initial orthopaedic surgical procedures and cultivating a damage control approach.
reduces many risks of pulmonary complication for many patients; however, the type of fixation is a point of contention. There is concern that a subset of patients, often those with severe thoracic injuries or lung contusions, may not respond well to intramedullary nailing in the acute phase of their resuscitation. The second hit theory states that during the initial treatment course, polytrauma patients develop elevated levels of inflammatory markers and cytokines as part of their systemic response to trauma. Some investigators have expressed concern that performing invasive orthopaedic procedures during the immediate posttrauma period can be associated with an exaggerated inflammatory response that can overwhelm the body and can lead to multiorgan system failure, sepsis, and death. The greatest elevation in the level of inflammatory markers seems to be associated with reamed intramedullary nailing of the femur, although new methods of reaming while irrigating and suctioning moderate these risks.4,5 Consequently, research is under way as to the specifics of this second hit theory, and it remains highly controversial regarding which patients will benefit from early intramedullary stabilization, and those who would benefit from minimizing the initial orthopaedic surgical procedures and cultivating a damage control approach.
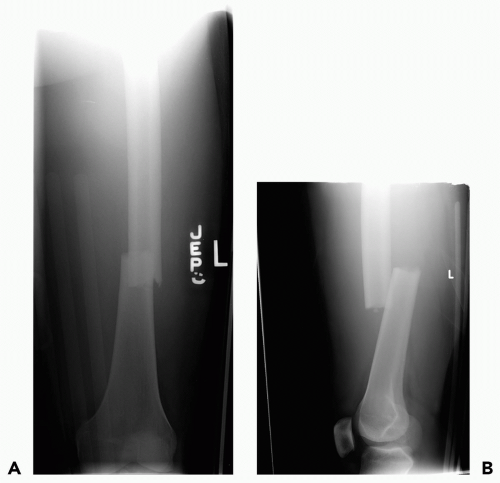 Figure 3 A: Anterior-posterior (AP) view of transverse femur fracture. B: Lateral view of transverse femur fracture. |
Patients who have sustained particularly severe multi-system trauma may benefit from minimizing the initial orthopaedic procedures. If a patient is hemodynamically tenuous or has sustained a severe chest or brain injury, a temporizing procedure such as external fixation may be the wisest initial treatment. Advantages of external fixation include that it can be applied very quickly and with minimal blood loss6 and that it can be performed concurrently while another surgical team performs a procedure on another site of the body. Disadvantages include the poor long-term results if the external fixation is used as definitive fixation, and the cost and risk of pin tract infections if the fixator is intended for only temporary stabilization.7
It is important that the primary trauma surgery team realizes that many external fixators are placed only for temporary stabilization of the fracture. Communication with the orthopaedic service should be maintained because external fixators require diligence to insure that the pin sites are kept clean, and that it does not stay in place too long. Ideally, the patient will be able to tolerate definitive fixation within the first 3 to 4 days of their admission, as the risk of complications with the exchange of external fixations for nails or plates increases the longer they stay in place. One potential exception involves open fractures with severe soft tissue injury. They may need to be spanned for a longer period of time until the wound and soft tissues have recovered enough to allow definitive fixation and coverage.
OPEN FRACTURES
Open fracture is one category of skeletal injury that requires prompt attention to optimize clinical outcome (see Fig. 4). Most North American orthopaedic surgeons employ the Gustilo and Anderson classification system to grade the severity of open fractures (see Table 1).8
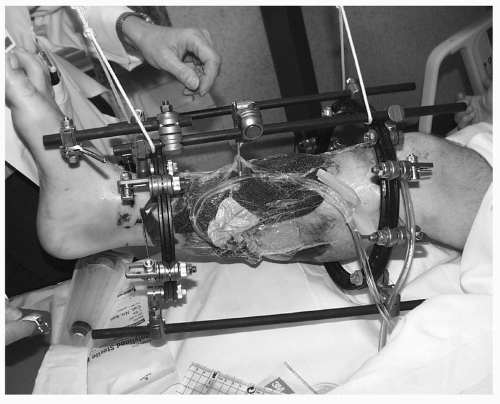
The introduction of negative pressure wound therapy (NPWT) devices (vaccum-assisted closure [VAC], Kenetic Concepts, Inc., San Antonio, TX) has remarkably improved our ability to cover open fractures that have significant soft tissue destruction without resorting to large free tissue transfers.9,10,11,12 The VAC is often placed at the end of the initial debridement, and then changed with each subsequent debridement (see Fig. 5). NPWT is thought to work through three mechanisms. First, it increases
blood flow and angiogenesis.13 Second, it is thought to improve the wound by removing excess fluid.14 This mechanism is very important in some injury patterns such as compartment syndrome and burns, but less important with other skeletal injuries. The third proposed mechanism of NPWT action involves mechanical stimulation of cell cytoskeletons leading to the production of substances and proteins associated with wound healing.15,16 An additional benefit of using NPWT in the operating room is that the wound is sealed off from the outside environment by the VAC dressing. This can be particularly helpful in patients who are in the intensive care unit environment where resistant organisms are more commonly encountered.17,18 The use of NPWT maybe associated with more rapid wound closure and a lower rate of infection in selected orthopaedic trauma patients.
blood flow and angiogenesis.13 Second, it is thought to improve the wound by removing excess fluid.14 This mechanism is very important in some injury patterns such as compartment syndrome and burns, but less important with other skeletal injuries. The third proposed mechanism of NPWT action involves mechanical stimulation of cell cytoskeletons leading to the production of substances and proteins associated with wound healing.15,16 An additional benefit of using NPWT in the operating room is that the wound is sealed off from the outside environment by the VAC dressing. This can be particularly helpful in patients who are in the intensive care unit environment where resistant organisms are more commonly encountered.17,18 The use of NPWT maybe associated with more rapid wound closure and a lower rate of infection in selected orthopaedic trauma patients.
TABLE 1 GUSTILO AND ANDERSON SYSTEM OF OPEN FRACTURE CLASSIFICATION | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||
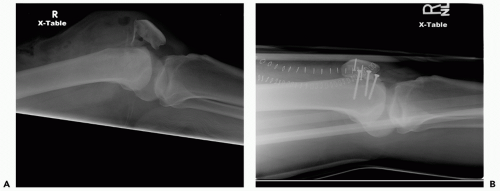
The initial treatment of open fracture should begin as soon as possible. Of course, life-threatening injuries always take precedence over limb-threatening injuries. However, once the trauma team has successfully addressed the initial ABCs and the patient is stable, the open fracture must be a priority. There are some important principles that should be kept in mind during the treatment of patients with open fractures: (i) limit the evaluation of the open wound to a single look; (ii) initiate antibiotics early; and (iii) initiate surgical irrigation and debridement expeditiously19,20,21,22 (see Fig. 6). The first principle is that the open fracture wound should be viewed once, and then kept covered. It will be very helpful if a digital photo can be taken when the wound is initially evaluated, so that subsequent caregivers can look at the photo rather than repetitively exposing the wound. The second principle is that antibiotic therapy should be initiated as soon as possible. For most open wounds this will include cefazolin 1 g every 8 hours, with the addition of an amiglycoside if the fracture is type II or III. If the wound is contaminated with soil or other sources of organic infection (i.e., ditch water or farm accidents) then penicillin or metronidazole should be added to the regimen. Alternatively, a broad-spectrum antibiotic plus penicillin, if there is organic contamination, can be employed. The rapidity of the initiation of appropriate antibiotic coverage is associated with decreasing the likelihood of the patient developing an infection or osteomyelitis.18,19 The tetanus status of the patient must also be determined; and without proof of tetanus vaccination status, patients should receive both toxoid of 0.5 mL and immunoglobulin of 250 U if they are older than 10 years. Following initial inspection, the wound should be covered with a sterile dressing, radiographs obtained, and a reduction attempted with splinting. The patient should be taken expeditiously to the operating room for a formal debridement and irrigation procedure and surgical stabilization of the fracture. If the patient is too unstable to be taken to the operating room quickly, a limited debridement and irrigation procedure should be undertaken in the intensive care unit. This procedure is performed using a sterile field, limited debridement, and pulsatile irrigation with at least 8 L of sterile saline (see Fig. 7). It is more controversial whether a cleansing procedure should be undertaken in the emergency room if a delay is anticipated in getting the patient to the operating room. Debridement should clearly not be performed in the emergency room or trauma bay, but a gentle washing with removal or gross contaminants is permissible. Sterile saline may be used with a “water can” cap that allows gentle irrigation, and one can add Betadine to the solution until the fluid is the color of iced tea. Any visible bone fragments should not be removed outside the operating room. There is no clear data to support or condemn a single gentle cleansing in the
emergency room. If such a procedure is performed, it is very important to understand that it is not a substitute for formal intraoperative debridement and irrigation.
emergency room. If such a procedure is performed, it is very important to understand that it is not a substitute for formal intraoperative debridement and irrigation.
GUNSHOT WOUNDS INVOLVING A FRACTURE
Fractures to the lower extremities caused by firearms require special consideration. As with all fractures, the mechanism can be very important to guiding the treatment of these fractures (see Fig. 8). Knowing whether the projectile came from a handgun, hunting or assault rifle, or shotgun, and from what range the injury occurred will aid in treatment. A close range injury is usually associated with higher energy than a bullet fired from a distance. More importantly, knowing the caliber and specifics of the ammunition can be of help. High-energy gunshot wounds create fargreater soft tissue damage in the zone of injury surrounding the fracture. These wounds require great vigilance and frequent trips to the operating room in order to avoid complications such as osteomyelitis, nonunion, or compartment syndrome. Treatment should be based on a thorough physical and neurovascular examination and supplemented by radiographs.
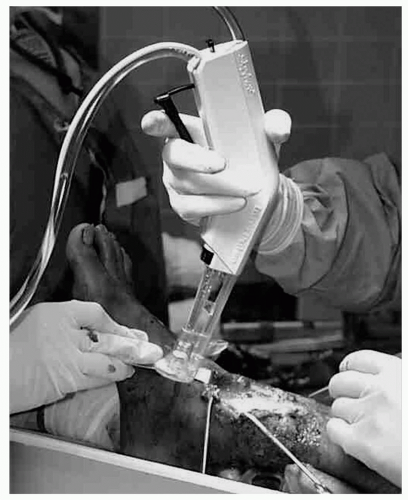 Figure 7 An example of pulsatile irrigation being performed in the operating room.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|