30
Flexor Tendon Injury
Flexor tendon repair and rehabilitation have posed challenges to surgeons and therapists for decades. Flexor tendons are required to glide large distances to allow the digits full composite flexion and extension, running within a tight pulley system to maximize their efficiency (Fig. 30-1). Following repair, flexor tendon adhesions develop quickly, because the tendon becomes adherent to surrounding tissue due to scar formation, especially when repaired within the pulley system. Once adherent, the flexor tendon does not glide as needed to perform active flexion, resulting in functionally limiting deficits in range of motion (ROM) with active range of motion (AROM) more limited than passive range of motion (PROM). Prevention of adhesions to the repaired flexor tendon would be possible if the tendon were allowed to glide immediately after surgery, but this approach historically resulted in rupture of the tendon repair. For this reason, a large number of solutions have been attempted over the past 50 years, resulting in numerous approaches to repair and rehabilitation. The goal of the evolving approaches has been to improve flexor tendon gliding by minimizing adhesion formation to the tendon while avoiding rupture of the repaired tendon.

Anatomy
The flexor tendons to the digits enter the hand through the carpal tunnel. They are comprised of the flexor digitorum superficialis (FDS) for each finger, flexor digitorum profundus (FDP) for each finger, and flexor pollicis longus (FPL) to the thumb. The FDP tendons are deep to the FDS tendons in the forearm, wrist, and hand. At the level of the proximal phalanx, the FDS tendon separates, becoming two separate slips, which then re-converge just before attachment on the middle phalanx (Fig. 30-2). The FDS flexes the metacarpophalangeal (MP) and proximal interphalangeal (PIP) joints. The FDP tendon emerges through the separation of the FDS tendon at the level of the proximal phalanx and continues distally to insert on the distal phalanx. The FDP tendon is the sole tendon responsible for distal interphalangeal (DIP) flexion of the finger. In the thumb, the FPL tendon inserts on the distal phalanx and is the sole flexor of the thumb interphalangeal (IP) joint.

As the flexor tendons run under the retinaculum and transverse carpal ligament at the wrist and palm, they are surrounded by a synovial bursa, which is a sheath filled with synovial fluid that allows tendon gliding without excess friction (see Fig. 30-1). A synovial sheath also surrounds the flexor tendons in the digit, where they run under a series of pulleys that prevent the flexors from bowstringing as active flexion occurs (see Fig. 30-1). Bowstringing describes the manner in which, when the pulleys are not intact, a flexor tendon is pulled away from the bone with a muscle contraction, rather than being efficiently pulled proximally. The pulleys that hold the flexor tendon snugly to the bone result in an efficient proximal glide of the flexor tendon with muscle contraction.
Diagnosis and Pathology
To diagnose if the FDP tendon is intact, hold the finger below the DIP joint and ask the client to bend the tip of the finger (Fig. 30-3). Because the FDP is the only flexor tendon to cross the DIP joint, active DIP flexion indicates that the FDP tendon is intact.

To diagnose whether the FDS tendon is intact, blocking the action of the FDP is necessary, because the FDP assists flexion at the PIP joint. To block the action of the FDP at the PIP joint and isolate the FDS to determine if it is intact, manually hold all the other fingers completely straight and ask the client to flex the PIP joint of the finger being tested (Fig. 30-4). The DIP joint of the finger being tested should be without tension if the FDP is being blocked successfully by holding the FDP of the other fingers at length.
Timelines and Healing
Flexor tendons retract after laceration or rupture, and surgical repair is necessary to allow healing to regain active motion. The tendon gradually heals after repair by both intrinsic and extrinsic means. The blood supply to the tendon enters from the dorsal surface of the tendon through vinculae supplied by the digital arteries (see Fig. 30-2). Flexor tendons are relatively avascular between these vinculae as well as on the volar surface of the tendon. The vinculae may be damaged during the injury or repair. Lacerated flexor tendons in the digit were initially thought to require blood supply from adhesions to heal following repair (extrinsic healing). Research has since shown that repaired flexor tendons have the ability to heal by nutrition from direct blood supply and from diffusion of nutrients in the synovial fluid that surrounds the tendons as they run within the pulley system (intrinsic healing).1
Tendon phases of healing include the inflammatory phase (0 to 2 weeks following repair), the fibroplasia phase, or reparative phase, (approximately 2 to 6 weeks following repair), and the remodeling phase (more than 6 weeks following repair).2 During the inflammatory phase, the tendon is at its weakest, and collagen is just beginning to be laid down at the repair site. The intermediate phase of tendon healing is when the tendon repair gains tensile strength. Tensile strength describes the amount of force the tendon will tolerate before rupture. During the late phase of tendon healing, the tendon repair continues to gain tensile strength and begins to remodel in alignment with the tension placed on it. The repaired flexor tendon is considered to have adequate tensile strength to tolerate most functional activities at 12 weeks after repair, and clients are allowed normal use of the hand at 12 to 14 weeks after repair. Rehabilitation following flexor tendon repair is, therefore, most protective of the repair for the first 3 to 4 weeks postoperatively with gradual advancement of force during active motion during the second month if active motion is limited, and use of specific exercises to assist the remodeling process in the third postoperative month of healing if adhesions limit tendon gliding. The advancement from passive flexion to active flexion and eventually resisted flexion depends on the tensile strength of the repair technique and each individual’s tissue response to injury and surgery. See the “Progression of Exercises” section for specific guidelines.
Operative Treatment
Flexor tendon repair techniques have been changing for the past decade. Historically, outcomes of flexor tendon repairs in the digit had been plagued by poor results because of adhesions or, if early active motion were attempted, rupture. Numerous studies have investigated suture materials and techniques to determine the best way to create a repair strong enough to tolerate immediate stress on the flexor tendon and obtain gliding while minimizing adhesions, without rupture.3–10 When lacerated, the flexor tendon ends are approximated and sutured with the technique of choice while attempting to maintain as much of the pulley system as possible. The A2 and A4 pulleys are the most important to preserve to prevent bowstringing. When the FDP has ruptured from its distal phalanx attachment or is lacerated within 1 cm of its distal attachment, the surgeon performs advancement and reinsertion of the tendon.9 In this situation, the FDP tendon is sewn back to the bone using a suture that extends through the tendon into the distal phalanx and is either attached to the bone with an anchor, or the suture is brought dorsally all the way through the bone and nail, where it is knotted over a button placed on the nail (Fig. 30-5). Repair of the FPL to the thumb is approached in a similar manner as finger flexor tendon repairs.

Research shows that, in general, the more strands of suture material that cross the tendon repair, the stronger the repair.3,10 The traditional suture repair technique consists of a two-strand repair, meaning that two strands of suture material cross the repair site. This type of repair tolerates application of an immobilization protocol or immediate passive motion protocol in the early phase of tendon healing, but it is not shown to be sufficiently strong enough to consistently tolerate immediate active motion protocols following a flexor tendon repair. A four-strand repair has been shown to tolerate gentle active motion.3 Repairs of six or more strands certainly will tolerate gentle active motion; however, these repairs are technically demanding and may become so bulky as to prevent gliding under the pulleys, create friction, possible wearing, and potential rupture. Thus a four-strand suture technique is commonly used for flexor tendon repair in which an immediate active motion protocol is applied, although some surgeons are electing to perform repairs with six or more strands.11
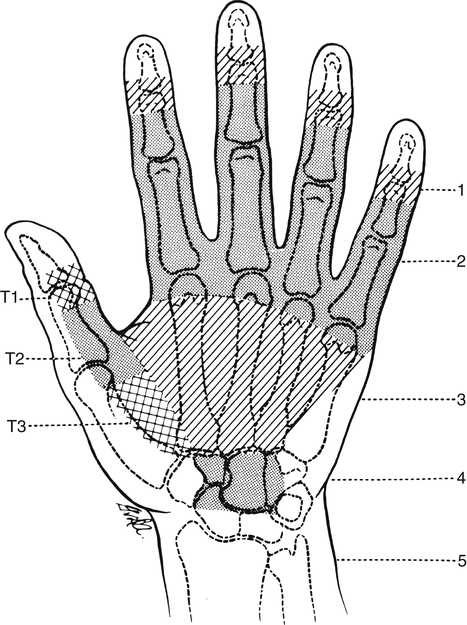
Postoperatively, flexor tendon rehabilitation poses a challenge to rehabilitation due to dense flexor tendon adhesions that occur within the flexor pulley system of the digit in zones 1 and 2. Flexor tendon zones of the hand are reviewed in Fig. 30-6. Three basic approaches to rehabilitation of the repaired flexor tendon in the hand are 1) immobilization, 2) immediate passive motion in the direction of the repaired tendon, and 3) immediate active motion in the direction of the repaired tendon. The main difference in these approaches is within the early phase, or first month, of tendon rehabilitation. All flexor tendon approaches protect the flexor tendon repair with some version of a dorsal blocking orthosis that flexes the wrist and/or MP joints to protect the repaired tendon from excessive stretch through approximately 6 weeks postoperatively. Box 30-1 summarizes the orthoses used in the early phase of rehabilitation within the various approaches following flexor tendon repair. The orthoses and exercises for each phase of healing are located in Tables 30-1 through 30-3.
TABLE 30-1
Immobilization Protocol Following Flexor Tendon Repair
| Early Phase | Intermediate Phase | Late Phase | |
| Orthosis | Dorsal blocking cast or orthosis | ||
| Exercises | Add the following: |
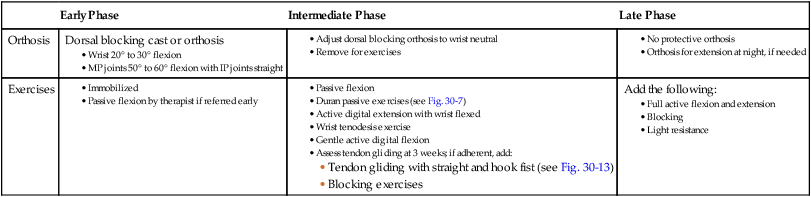
TABLE 30-2
Immediate Passive Flexion Protocols Following Flexor Tendon Repair
| Early Phase | Intermediate Phase | Late Phase | |
| Static positioning orthosis | Dorsal blocking orthosis (see Fig. 30-8): | ||
| Elastic traction orthosis | |||
| Exercises | Remove orthosis, and add the following: | Add the following: |
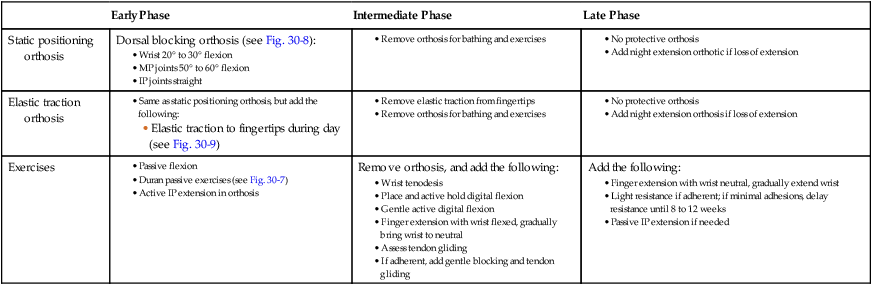
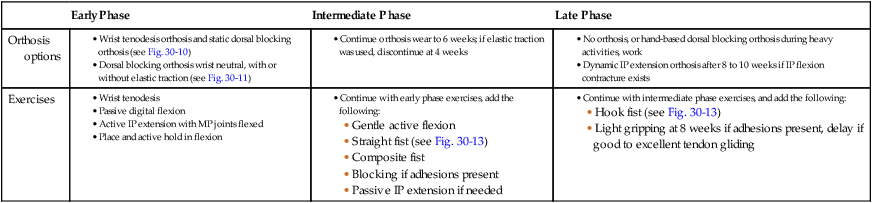
TABLE 30-3
Immediate Active Flexion Protocols Following Flexor Tendon Repair
| Early Phase | Intermediate Phase | Late Phase | |
| Orthosis options | |||
| Exercises |
Approaches of Rehabilitation in the Early Phase of Flexor Tendon Healing
An immobilization approach12,13 is rarely applied following repair of the flexor tendon in the digit, but there are certain situations for which it is appropriate. Children younger than age 12 are most often placed in immobilization for the first 3 to 4 weeks, but evaluate each child related to their maturity level and ability to comply with the exercises and precautions of other approaches. Other individuals who may be placed in immobilization after a flexor tendon repair are those who have cognitive limitations, such as Alzheimer’s and noncompliant clients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




