Flexor and Extensor Tenosynovectomy
Kyle P. Kokko
John T. Capo
Sanjiv Naidu
Jay T. Bridgeman
DEFINITION
Synovium lines the joint spaces and tendon sheaths and secretes a lubricant (hyaluronan and synovial fluid constituents from type B synoviocytes) needed for tendon gliding and reduces friction in synovial joint motion.
Tendons may be both extra- and intrasynovial.
Flexor tendons in the carpal tunnel have the added feature of subsynovial connective tissue, which can become inflamed.
Tenosynovitis is defined as the inflammation of tendon sheaths in extrasynovial tendons and the inflammation of the synovial lining in intrasynovial tendons.4
ANATOMY
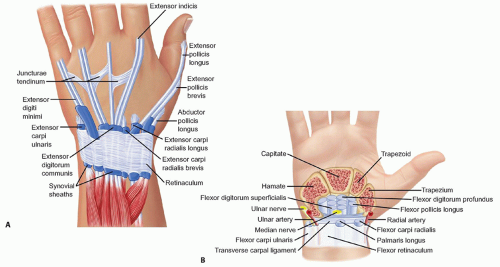
The extensor tendons lie under the dorsal retinaculum in six separate extensor (or dorsal) compartments. They are numbered in succession from one to six, beginning radially and ending ulnarly. The portions of the extensor tendons that lie under the dorsal retinaculum are lined with synovial sheaths (FIG 1A).
The extensor tendons that occupy the first dorsal compartment are the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB). They originate as “outcropper” muscles from the distal third of the forearm and cross over the second dorsal compartment tendons—the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB)—distally at the level of the wrist approximately 4 cm proximal to the radial styloid.
The extensor pollicis longus (EPL) in the third extensor compartment makes an acute angle at the Lister tubercle at the level of the wrist and crosses superficial to the second dorsal compartment.
The fourth extensor compartment tendons—the extensor digitorum communis (EDC) and the extensor indicis proprius (EIP)—lie under a broad retinaculum. The posterior interosseous nerve (PIN) lies in the floor of the fourth extensor compartment deep to the EDC and EIP tendons on the radial aspect of the compartment.
The extensor digitorum quinti (EDQ) in the fifth extensor compartment often is the only tendon to motor the small finger metacarpophalangeal (MCP) joint in the act of extension.
The extensor carpi ulnaris (ECU) tendon in the sixth dorsal compartment lies in a fibro-osseous tunnel and is intimately held in the ulnar groove by a subsheath that is critical for distal radioulnar joint stability and is a component of the triangular fibrocartilage complex (TFCC).
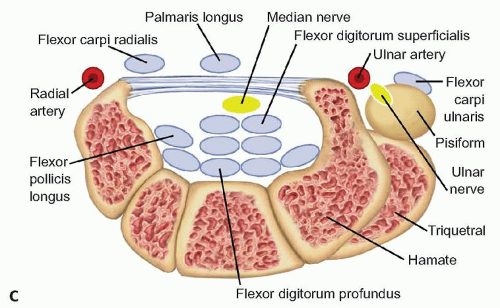
The wrist flexor tendons—the flexor carpi radialis (FCR), the palmaris longus (PL), and the flexor carpi ulnaris (FCU)—are extrasynovial tendons.
The FCR passes through a tight fibro-osseous tunnel in the trapezium before inserting on the base of the second metacarpal (FIG 1B,C). Whereas the FCU, attaches first on the pisiform bone that functions as a sesamoid bone and then has distal attachments to the base of the fifth metacarpal.
The digital flexor tendons lie under the transverse carpal ligament in the carpal tunnel. Unlike digital extensor tendons, flexor tendons are almost entirely intrasynovial.
The flexor tendons in the digits lie in a fibro-osseous canal formed by the annular and cruciate ligaments.3
PATHOGENESIS
Rheumatoid arthritis is a disease of synovial tissue that can lead to inflammatory tensosynovitis. However, proliferative extensor tenosynovitis has been described in the absence of rheumatoid arthritis.2
Flexor and extensor tenosynovitis is commonly a sequelae of rheumatoid arthritis.
Rheumatoid arthritis causes formation of hypertrophic synovium in the joint spaces, thereby destabilizing joints. The hypertrophic synovium invades the tendon sheaths and synovial lining of all tendons.4
NATURAL HISTORY
Inflammatory tenosynovitis usually is painless and can be the first sign of rheumatoid arthritis.
The dorsal and volar wrist, as well as the volar digits, are most commonly affected.
The synovial tissue proliferates in the tendon sheath and eventually may invade the tendon.
The end result can be weakening and rupture of the tendon.4
PATIENT HISTORY AND PHYSICAL FINDINGS
Tenosynovitis of the first extensor compartment (de Quervain tenosynovitis) reveals thickening of the EPB and APL tendon sheaths at the radial styloid. This thickening can produce a positive Finkelstein test: pain elicited along course of the APL and EPB with ulnar wrist deviation with the thumb cupped within the loose grasp of the index, middle, and ring fingers.
Second compartment extensor tenosynovitis (intersection syndrome) often presents with painless swelling of the dorsum of the wrist 4 cm proximal to the radial styloid. There is focal tenderness to palpation with swelling and positive Tinel sign of the sensory branch of the radial nerve.
Third extensor compartment tenosynovitis usually presents with rupture of the EPL tendon. This results in inability to raise the thumb (thumb retropulsion) when the hand is placed flat on a table.
Chronic fourth extensor compartment tenosynovitis often presents with focal swelling in extensor zone 7 along with multiple tendon ruptures (FIG 2).
Fifth extensor compartment tenosynovitis usually is accompanied by dorsal distal ulna instability and tendon rupture.
Sixth extensor compartment tenosynovitis is manifested as ECU instability in addition to significant intrasynovial inflammation at the level of the ulnar styloid.
Pain at the wrist indicates that the radiocarpal or radioulnar joint is affected.
Flexor tenosynovitis at the wrist can cause median nerve compression in the carpal tunnel as well as decreased active and passive range of motion of the fingers.
Flexor tenosynovitis of the digits can cause triggering.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree