Flexion Intertrochanteric Osteotomy for Severe Slipped Capital Femoral Epiphysis
Young-Jo Kim
DEFINITION
Pistol grip deformity after slipped capital femoral epiphysis (SCFE) can cause anterior impingement leading to pain, cartilage and labral damage, and eventual osteoarthritis.1, 2, 8
Realignment of the proximal femur, as well as restoration of the anterior head-neck offset, has been shown to improve hip clinical outcomes.7
This technique can be used to correct anterior impingement after an SCFE that has healed with residual posterior displacement.
The first part of the procedure is a surgical hip dislocation approach with femoral head-neck osteoplasty.
If additional deformity correction is needed, the flexion intertrochanteric osteotomy is performed.
PATHOGENESIS
The true etiology of SCFE is unclear. However, because it occurs mainly in adolescent boys (80%), hormonal factors are thought to be involved.
Additionally, the orientation of the growth plate becomes more vertical in adolescents compared to the juvenile hip, leading to increased shear stress across the physis.
The transition from juvenile to adolescent is a period of rapid weight gain, leading to the stereotypical obese body habitus in the SCFE patient.
NATURAL HISTORY
Undetected SCFEs can lead to hip arthrosis. Murray4 suggests that up to 40% of hips with degenerative arthritis have a “tilt deformity” or other deformities that may be due to an undetected subclinical SCFE or other developmental problems.
A review by Aronson1 found that 15% to 20% of patients with SCFE had painful osteoarthritis by age 50 years. Additionally, 11% of patients with end-stage osteoarthritis had an SCFE.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients will complain of insidious-onset groin or knee pain that may have previously been diagnosed as a sprain.
They may walk with a limp, but typically they walk with an externally rotated foot progression angle, which may indicate chronic SCFE or femoral retroversion.
Pain is elicited with hip flexion, adduction, and internal rotation stress (impingement test).
The physical examination should include flexion and internal rotation range-of-motion tests. Normal, physiologic hip flexion needed for activities of daily living is at least 90 degrees.
Patients with a chronic SCFE and anterior impingement will have less than 90 degrees of true hip flexion.
Patients with impingement secondary to SCFE will have less internal rotation in flexion than extension and may have a compensatory external rotation of the hip as it is flexed (obligate external rotation).
IMAGING AND OTHER DIAGNOSTIC STUDIES
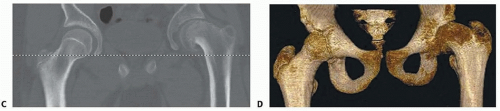
Plain radiographs include an anteroposterior (AP) and frog-leg lateral views of the pelvis or the involved hip (FIG 1A,B).
Computed tomography (CT) scans with two- and three-dimensional reconstructions are helpful for preoperative planning (FIG 1C,D).
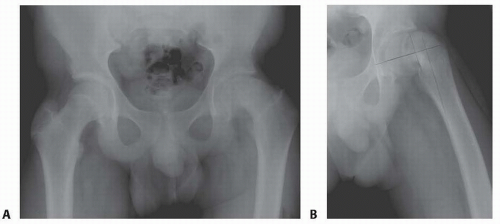
FIG 1 • Preoperative AP (A) and frog-leg lateral (B) radiographs of the left hip demonstrate a chronic, stable severe SCFE with greater than 70 degrees of posterior slippage. (continued)
DIFFERENTIAL DIAGNOSIS
Femoral or acetabular retroversion
Idiopathic femoroacetabular impingement
NONOPERATIVE MANAGEMENT
Nonoperative management includes cessation of aggravating activities and symptomatic treatment using nonsteroidal anti-inflammatories.
Physical therapy to strengthen the hip musculature does not address the mechanical impingement associated with an SCFE.
All SCFE should be stabilized surgically. Nonoperative management if for impingement symptoms.
SURGICAL MANAGEMENT
A chronic slip may be pinned in situ to prevent continued slippage. Remodeling of the SCFE deformity has been described in long-term follow-up studies.
Corrective osteotomies have been described through the femoral neck at the growth plate (cuneiform), at the base of the femoral neck, or intertrochantic or subtrochanteric.6
Preoperative Planning
The anterior head-shaft angle is measured on the AP pelvis radiograph on both the affected and normal sides. The difference is the amount of varus deformity on the slip side that can be addressed with a valgus-producing intertrochanteric osteotomy (FIG 2A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree