Fractures that occur above or around the femoral component of a total knee arthroplasty (TKA).
The rates of periprosthetic fractures for TKA vary.
The incidence is reported to be 0.3% to 5.5% after primary TKA and up to 30% after revision TKA.3, 5, 6, 13
Supracondylar femur fractures are the most common type and the most widely reported with an incidence of 0.3% to 2.5% for primary TKA and 1.6% to 38% for revision TKA.5, 6, 8, 13
Can occur in the setting of a stable prosthesis or an unstable prosthesis
Periprosthetic fractures can create substantial difficulty with regard to management and outcome.
Reduction and fixation of these fractures is a complex undertaking, primarily as a result of the preexisting implants that can obstruct reduction and placement of fixation devices.2
The distal femur is a trapezoidal shape.
The lateral distal femur is larger in the anteroposterior (AP) diameter than the medial distal femur.
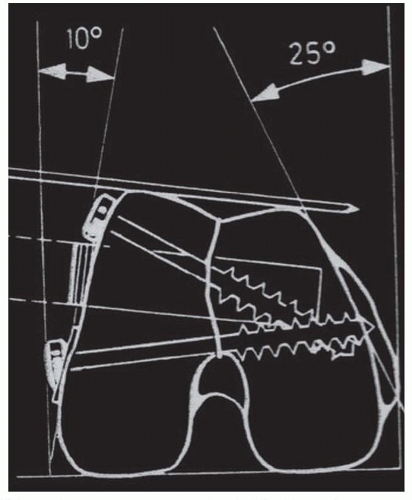
FIG 1 • Schematic representation of axial of distal femoral anatomy. Note the trapezoidal shape and angular differential on lateral versus medial side.
The lateral femoral condyle has a 10-degree slope.
The medial femoral condyle has a 25-degree slope (FIG 1).
The origin of the gastrocnemius on the distal femur acts as a deforming force leading to a recurvatum deformity.
The insertion of the adductors on the distal femur acts as a deforming force leading to a varus deformity (FIG 2).
Most periprosthetic femur fractures typically result from a low-energy fall in the elderly or a high-energy trauma in a young person.1
Multiple risk factors have been identified.
Metabolic issues such as osteoporosis are known risk factors for the development of periprosthetic fractures about a TKA.
Many studies have demonstrated a decrease bone mineral density after TKA.11
Surgical technique has also been implicated, specifically notching of the distal femur.
Violation of the anterior cortex of the distal femur has been thought to be an important risk factor for periprosthetic distal femur fracture after TKA.
There is a theoretical increased risk due to the change of the geometry of the femur and the decrease radius of curvature leading to higher stresses on the distal femur.
The goals of treatment, whether surgical or nonsurgical, are fracture healing, restoration and maintenance of knee range of motion, and pain-free function.
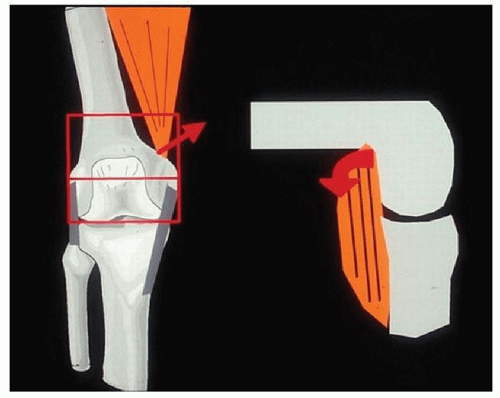
FIG 2 • Schematic representation of main muscular deforming forces to distal femoral fractures (adductors and gastrocnemius, respectively).
A good result is a minimum of 90 degrees of knee motion, fracture shortening less than or equal to 2 cm, varus/valgus malalignment less than or equal to 5 degrees, and flexion/extension malalignment less than or equal to 10 degrees.14
Nonsurgical management using skeletal traction, casting, or cast bracing has been used in primary fractures; however, due to the prolonged immobility and risks associated, surgical intervention is preferred unless the patient is too sick to undergo the procedure.
It is important to get a history and try to elicit any preexisting symptoms that may indicate whether or not an implant is loose, such as pain or instability.
Medical records are helpful to identify surgical approach as well as type of implants.
If there is suspicion for infection based on preexisting symptoms or preinjury films demonstrating loosening, further investigation should take place to include complete blood count (CBC), erythrocyte sedimentation rate (ESR), and noncardiac C-reactive protein (CRP).
If the infection workup is suspicious, then intraoperative biopsy or staged procedures should be planned.
Following a general medical examination, a comprehensive examination of the affected limb should be performed.
The condition of the skin and neurovascular status should be documented.
Specifically, ankle-brachial index (ABI) should be performed and documented.
An ABI less than 0.90 warrants further investigation.9
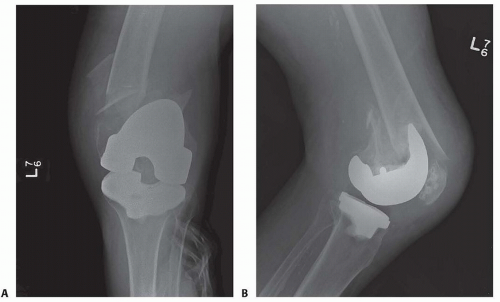
Standard AP and lateral of the affected extremity should be obtained (FIG 3).
It is also routine practice to get images of the joint above and below the injury.
Mechanical axis series can also be beneficial in certain instances.
Advance imaging can be helpful to determine bone stock but are not routinely required (FIG 4).
Loose TKA
Infected TKA
Periprosthetic tibial fracture
Periprosthetic patellar fracture
Periprosthetic fracture around a total hip arthroplasty (THA)
Indication for nonoperative management include truly nondisplaced fractures with a stable prosthesis or a patient that is too medically unstable for surgery.
Nonsurgical management includes skeletal traction, casting, or cast bracing.
Nonsurgical management does eliminate the surgical risks such as bleeding, infection, loss of fixation, and anesthetic complications.
With nonsurgical management, the extremity should be kept immobilized in extension for 4 to 6 weeks and the patient kept non-weight bearing.
Once surgical management has been decided, it is crucial to determine if the implant is stable or not.
Fractures about a stable femoral component are typically treated with intramedullary nailing (IMN) or laterally based locked plating.
Retrograde IMN represents a good option when there is adequate bone stock and an “open box” TKA femoral component.
Locked plates represent a significant advance in the treatment of periprosthetic fractures of the distal femur.
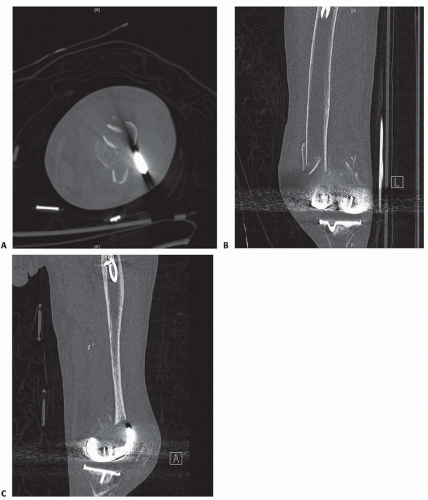
FIG 4 • Axial (A), coronal (B), and sagittal (C) CT scan of distal femoral periprosthetic fracture that shows location and comminution.
Advantages of locked plating include the ability for multiple fixed-angle points of fixation in osteoporotic bone, increased biomechanical strength over conventional plates, and the ability for insertion in minimally invasive techniques.10
When minimally invasive techniques are used, it is crucial to avoid the typical malalignment of valgus and hyperextension of the distal fragment.4
When periprosthetic fractures above a TKA are associated with a loose component, revision arthroplasty is the treatment of choice.
The history and physical is reviewed.
Preinjury radiographs are reviewed if available to determine if there was any evidence of loosening or infection.
Evidence of infection requires further workup as mentioned earlier.
Prior operative reports are obtained and reviewed specifically looking for type of implant to determine if the femoral component is an open box or not (Table 1).
Injury films are reviewed and classified (Table 2).
Key factors in decision-making process for operative treatment:
Is the bone stock adequate?
Does the implant have an open or closed box?
Is the implant loose or stable?
If the implant is stable and there is adequate bone stock, then open reduction and internal fixation (ORIF) is treatment of choice:
If implant has open box, then IMN versus laterally based locked plate
If implant has closed box, then laterally based locked plate
If the implant is loose, then revision arthroplasty
Table 1 Chart of Common Manufacturers and Implants with Representative Intercondylar Width That Limits Nail Size Usage for Retrograde Intramedullary Nailing of Distal Femoral Periprosthetic Fracture | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree