First Dorsal Metacarpal Artery Island Flap
Günter Germann
Katrin Palm-Bröking
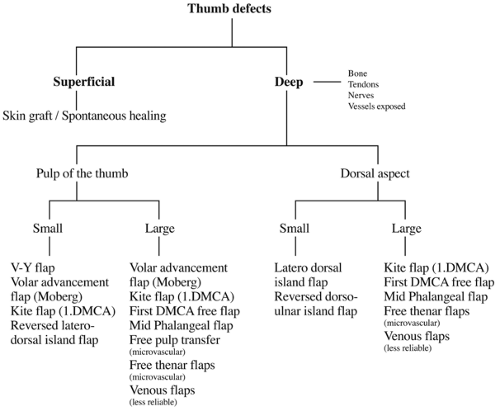
Soft tissue defects in the hand, and particularly in the thumb, frequently present difficult reconstructive problems because of the restricted availability of local tissue. Although local skin flaps have been employed and time-proven over decades, the philosophy of immediate wound closure of complex defects with exposure of tendon, bone, or joints has stimulated interest in anatomic research and the development of refined reconstructive techniques (10).
Traditional flaps have many disadvantages such as two-stage operations (i.e., cross-finger flap [17,24]), tedious dissections with considerable donor-site morbidity and loss of discriminative power (i.e., Littler flap [27,28]), or limited arc of rotation and mobility (i.e., transposition flaps [7] and the Moberg flap [1,8]). On the other hand, more recent microsurgical reconstructions such as the free pulp flap (7) require a significant amount of time and a familiarity with microsurgical technique. The first dorsal metacarpal artery island flap overcomes the disadvantages of traditional hand flaps and can provide a moderate-sized skin paddle on a long consistent vascular leash, allowing one-stage reconstruction for thumb and dorsal hand wounds without the need for microsurgical anastomosis.
The first dorsal metacarpal artery island flap was originally described by Hilgenfeldt in 1950 (16) and subsequently refined by Paneva-Holevic in 1968 and finally described as a pure island flap (“kite flap”) by Foucher and Braun in 1979 (8). Many variations of the flap have since been described and established in daily clinical use based on the consistent anatomy of the dorsal metacarpal arterial arcade (3,4,5,6,7,9,10,11,12,19,20). The majority of the flaps in recently published reports are raised from the dorsal aspect of the hand with only a few being found on the palmar surface (2,13,14).
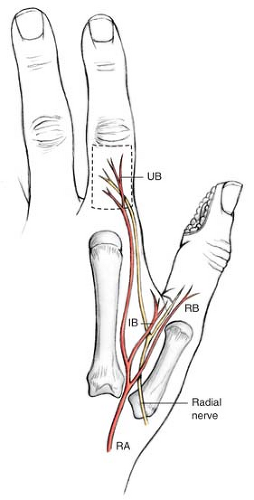
The dorsum of the hand is supplied by the network of dorsal metacarpal arteries which are fed from the main forearm vessels: the radial, ulnar, and interosseus arteries. The first dorsal metacarpal artery (FDMA) consistently arises from the radial artery or the princeps pollicis artery and runs distally to the fascia of the interosseus muscle, frequently embedded in a fascial pocket. In most cases the first dorsal metacarpal artery divides in the middle of the second metacarpal into three terminal branches (18,22,24,30). The radial branch of the first dorsal metacarpal artery goes to the thumb, while the intermediate branch runs to the first web space. Distally the ulnar branch usually terminates at the level of the metacarpo-phalangeal joint and then arborizes into the dorsal skin of the index finger after giving off a perforating branch at the level of the metacarpal neck.
The exact location of the artery with respect to the first dorsal interosseous muscle may vary. Kuhlmann and de Frenne found the artery to run superficial to the muscle in 75% of specimens, while the FDMA was found within the muscle in 15% of specimens; in 10% of specimens the artery ran within and on top of the muscle during its course. Dautel and Merle identified a superficial course of the FDMA in 36% of specimens, a supra-fascial course in 23% of specimens, and a deep, intramuscular course in 56%. Despite its exact location all authors agree on the consistency of a FDMA (11,13,18,22,24,30) (Fig. 23-1).
Indications/Contraindications
Indications
Indications for the first dorsal metacarpal artery flap (“kite flap”) are based on the following criteria:
Etiology, location, size, and condition of the defect
Availability of the flap (i.e., previous injuries that may compromise the vascular pedicle)
Suitability of the flap for the defect (e.g., size, arc of rotation)
Inclusion of other tissue components (i.e., tendon, bony segment)
Patient’s wishes (donor site morbidity, aesthetic appearance)
Surgeon’s familiarity with the technique
Based on these decision-making criteria, the flap is indicated for primary or secondary reconstructions of:
The dorsal aspect of the thumb
Restoration of sensibility with pulp reconstruction in the thumb
Skin defects at the dorsal aspect of the hand within the arc of rotation of the antegrade kite flap
Palmar defects of the index finger
Defects of the web space
Defects around the wrist
Defects at the base of the thumb or the middle finger (“retrograde kite flap”)
Complex flaps including various tissue components
Microvascular flap transfer based on the vascular pedicle in the snuff box
The list of indications demonstrates the versatility of the flap: however, reconstruction of the thumb takes precedence as the main indication in most centers.
Following the pioneer work of Tränkle et al, the flap has replaced other sensate neurovascular island flaps for restoration of sensibility in the thumb (10




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree