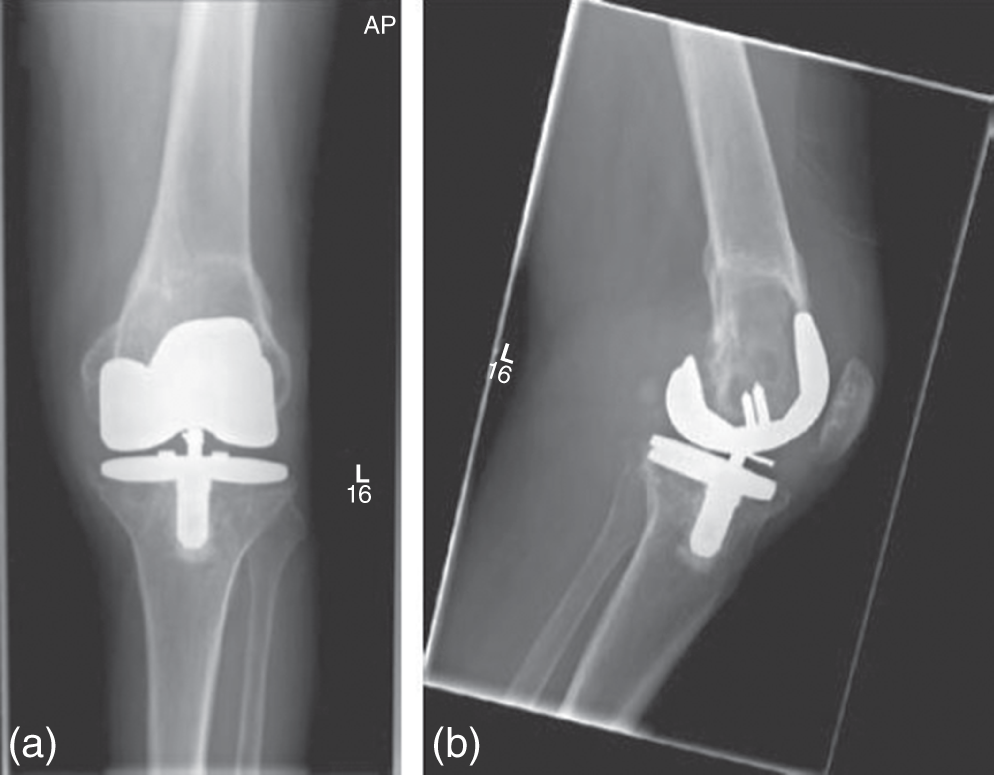
Adam Katchky MD MSc FRCSC1 and David J. Backstein MEd MD FRCSC2 1Niagara Health System, Welland, ON, Canada 2Mount Sinai Hospital, University of Toronto, ON, Canada One challenge of revision total knee arthroplasty (RTKA) is assessment and restoration of bony defects. Bone loss is often classified according to the Anderson Orthopaedic Research Institute (AORI) Bone Defect Classification.1 Defects may be characterized as contained or uncontained. Contained defects may be cavitary, representing loss of cancellous bone with intact cortical rim. By contrast, uncontained defects represent cancellous bone loss in addition to significant loss of surrounding supportive cortical bone. Uncontained defects may be segmental involving the medial or lateral side of the femur or circumferential, involving the entire bone.2 In 2008, Lawrence et al. estimated that clinical osteoarthritis affects up to 27 million adults in the US, with 18 million affected by knee osteoarthritis.3 For patients with end‐stage knee arthritis, TKA is a common and successful procedure with over 95% survivorship at 10 years4–6 and 90% survivorship at more than 15 years follow‐up.7–10 In spite of the relative success of this procedure, increasing TKA utilization has carried with it increasing rates of RTKA. Increased RTKA costs are driven by longer operating times, costlier implants, additional materials, longer hospital stays, and longer periods of convalescence.11 Therefore, any treatment modality which can reconstruct bone defects in an efficient manner, while allowing for immediate weight bearing and mobilization, is preferable in the opinion of the authors. Unfortunately, outcomes and success rates of RTKA are not comparable with primary TKA.12,13 Structural bone defects commonly contribute to the complexity of RTKA.14,15 The major etiologies of bone loss include implant wear and osteolysis, aseptic loosening, infection, and stress shielding.16,17 A detailed understanding of the location and extent of osteolysis/bone loss, and the quality/quantity of remaining distal femoral bone, is essential for proper planning and management. This is particularly important for surgeons operating in a facility which does not have the equipment and implants necessary to all modalities of reconstruction readily available. A thorough clinical assessment is essential prior to knee revision surgery to evaluate the patient’s health status with possible consultation from internal medicine and anesthesia. The operative site is assessed for previous incisions and potential wound complications and workup for infection is performed using blood tests, imaging, and possibly joint aspirate for culture. The reason(s) for TKA failure should be established and a management plan formulated. Component position, stability, and degree and location of bone loss should be assessed with x‐rays and CT. Adequate assessment of these aspects of the clinical scenario will allow the surgeon to plan the reconstructive technique and ensure availability of all necessary equipment. Multiple studies help address this question, including one prospective study,18 two retrospective studies,19–21 and one cadaveric study.22 Overall quality of evidence is moderate. Figure 57.1 Representative radiographs of 69‐year‐old man with osteolysis around TKA implants. (a) Anteroposterior and (b) lateral radiographs of TKA with femoral bone loss secondary to osteolysis. Assessment of bone loss using routine x‐rays has been shown to lead to underestimation, and further imaging should be obtained including oblique views or CT scan to achieve reasonable prediction of defect size (Figure 57.1 and 57.2).18–20,22 Agreement between plain x‐ray and intraoperative assessment of bone loss has been shown to be fair based on the AORI classification.22 Also, analysis of 31 patients who had osteolytic lesions confirmed by multidetector CT, plain radiography detected only 17% of lesions.21 Figure 57.2 CT scan showing femoral bone loss due to osteolysis on cross‐sectional imaging in the same 69‐year‐old patient. Representative (a) sagittal, (b) coronal, and (c) axial images showing degree of bone loss. While smaller contained defects are simpler to manage, larger structural defects often require the use of advanced reconstructive strategies. Multiple reconstructive techniques have been proposed to manage these defects, with the goal of optimizing patient outcomes following this technically demanding procedure. Small, contained defects can be filled with cement23,24 or with impacted morselized bone graft. Cement has been shown to provide inferior load transfer with poor fatigue properties,25–27 and bone grafting may be preferred due to its biological advantage.28,29 Smaller uncontained defects may be treated successfully with metallic block augments.30,31 Large defects with metaphyseal bone loss must be reconstructed to achieve implant stability, and may require augmentation with allograft or synthetic materials. Traditionally, these defects have been managed with structural and/or morselized allograft in the setting of RTKA. Similar to smaller defects, allograft reconstruction of large bone defects has the advantage of restoring bone stock. Advances in material science and the development of highly porous metal reconstructive augments (titanium sleeves, tantalum cones) has created new strategies for managing femoral defects, which avoid some of the pitfalls of allograft implantation (disease transmission, graft resorption, poor availability). Both metallic options represent somewhat different philosophies. Tantalum cones are nonlinked to the prosthesis. The preparation of the bone bed for cones is more demanding as precise bone contouring is required while sleeves utilize a simple broaching technique. Sleeves are directly linked to the prosthesis in order to form a single unit, while cones require cement for connection to the TKA prosthesis. No studies were identified which directly compare the results of these reconstructive approaches. Four retrospective case series32–35 (level IV evidence) report outcomes following reconstruction with tantalum cones, while a further two prospective36,37 and three retrospective studies38–40 report outcomes using porous titanium sleeves. Outcomes of structural allograft reconstruction are reported in one prospective cohort,41 two cross‐sectional studies,42,43 and five retrospective case series.2,44–47 Overall quality of evidence is moderate due to heterogeneity of patient population, reconstructive techniques, and outcome measures reported. A single comparative study was identified comparing reconstruction with and without structural allograft;43 however, the population is heterogeneous, as are the techniques utilized in the nonstructural allograft group. As a result, conclusions which address this question are difficult to draw. The Knee Society knee and functional scores (KSS) are the most commonly reported patient‐reported outcome measures (PROMs)2,32,36,37,40,41,44,45 and scores appear to be highest in titanium sleeve reconstruction (81.0, 78.8) than with tantalum cones (66.0, 61.1) or structural allograft (79.3, 60.0); however, the clinical and statistical significance of this difference is unknown.
57
Femoral Bone Defects in Revision Total Knee Arthroplasty
Clinical scenario
Introduction
Top three questions
Question 1: In patients with periprosthetic distal femoral bone defects, does computed tomography (CT) scan more accurately estimate defect size when compared to x‐ray?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Resolution of clinical scenario

Question 2: In large contained distal femoral defects with metaphyseal compromise, does metallic reconstruction (cones/sleeves) yield improved survivorship compared to structural allograft reconstruction?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





