Extra-articular Reconstructive Techniques for the Distal Radioulnar and Ulnocarpal Joints
Christopher J. Dy
E. Anne Ouellette
Anna-Lena Makowski
DEFINITION
The diagnostic and therapeutic challenge presented by instability of the ulnocarpal joint reflects the inherent biomechanical and anatomic incongruity of the articulation.
The triangular fibrocartilage complex (TFCC) provides the majority of anatomic and functional stability of the distal radioulnar and ulnocarpal joints.1,17
As expected, the consequences of TFCC lesions reflect a disruption of its normal function.3 The Hui-Linscheid procedure and the modified Herbert reconstruction are two approaches to achieve surgical stabilization of the distal radioulnar joint (DRUJ). The Hui-Linscheid reconstruction stabilizes the DRUJ by augmenting function of the ulnocarpal ligament,7 whereas the modified Herbert reconstruction restores the radioulnar and ulnocarpal functions of the TFCC by ligamentotaxic constraint of the ulnar carpus.4
ANATOMY
The ulnar carpus does not directly articulate with the distal ulna; instead, the ulnar carpus is suspended from the ulnar head by the TFCC.
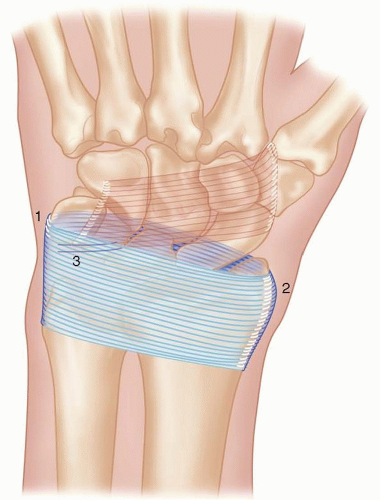
The TFCC is a collection of soft tissue structures that stabilizes the radial-ulnar-carpal unit (FIG 1). It consists of fibers originating from the subsheath of the extensor carpi ulnaris, the ulnocarpal ligaments, the dorsal and palmar radioulnar ligaments, and the triangular fibrocartilage proper.
The TFCC provides a continuous gliding surface that spans the distal surfaces of the radius and ulna, allowing carpal movements and acting as a dynamic stabilizer of the forearm during pronation and supination.13,19 In addition to its radioulnar function, the TFCC stabilizes the ulnar side of the carpus, aids in load transference from the ulnar carpus to the ulna, and cushions ulnocarpal forces.17
The dorsal and volar distal radioulnar ligaments, which are often referred to as the marginal ligaments, help to stabilize the radioulnar joint through its extremes of motion.
Although controversy exists concerning the exact role of each marginal ligament, several authors have agreed that the ligaments act in concert to stabilize the DRUJ during pronosupination.
The extensor retinaculum is a thick fibrous band of tissue that holds the extensor tendons against the distal radius and ulna to prevent bowstringing and displacement of the tendons (FIG 2). It is continuous with the palmar carpal ligament and shares connecting fibers with the flexor retinaculum just proximal to the pisiform. The extensor retinaculum attaches to the pisiform and triquetrum medially and to the lateral margin of the radius laterally. It is positioned from a proximal-radial to distal-ulnar direction.16,20
PATHOGENESIS
Injuries to the TFCC can occur secondary to trauma, such as a fall on the outstretched hand, or from degenerative changes caused by repetitive loading, especially in patients with rheumatoid arthritis. Palmer has classified TFCC abnormalities by differentiating between traumatic and degenerative pathologies, with further specification within each group.12
Dorsal subluxation of the ulnar head, with or without supination deformity of the radiocarpal complex and ulnocarpal instability, can occur with attenuation or tears of the dorsal radioulnar ligaments.17,19 The Hui-Linscheid reconstruction repairs these defects through augmentation of ulnocarpal ligament function and an optional imbrication of the attenuated dorsal radioulnar ligament.5,7
Ulnocarpal instability may also result from incompetence of the ulnocarpal ligaments, either secondary to acute trauma or from accumulative attrition.1,8 The modified Herbert reconstruction addresses ulnocarpal instability by using ligamentotaxis to stabilize both the ulnocarpal and radioulnar aspects of the DRUJ.4,14
NATURAL HISTORY
Ulnocarpal instability is a relatively common finding in the general population. Approximately, two-thirds of asymptomatic volunteers were found to have some form of ulnocarpal instability on physical examination.11 Medical or surgical intervention is necessary if symptoms are present or are worsening.
The unstable ulnocarpal joint uses the radiocarpal joint as a pivot. The abnormal rotation in this pathologic state leads to increased pain, weakness, and loss of function during wrist supination. In addition, an ulnar-sided supination deformity may be present.
PATIENT HISTORY AND PHYSICAL FINDINGS
In both acute and chronic cases, the clinical presentation of the ulnocarpal instability consists of ulnar-sided wrist pain with or without clicking, especially with forearm pronation-supination activities, such as putting topspin on a tennis ball with a forehand shot.
There may be demonstrable laxity during supination and weakness in passive or active pronation-supination movements. These symptoms may hinder range of motion and function of the wrist.
On physical examination, patients often localize tenderness to the ulnar carpus on palpation.
The examiner should palpate the ulnar styloid.
The examiner should palpate between the ulnar styloid and triquetrum.
Visual inspection of the ulnocarpal area is important, looking for swelling and alignment of the carpal area in relation to the ulna. Swelling may be the result of acute injury. Position of tissues indicates stability or instability.
In the absence of concomitant pathology, provocative maneuvers such as Watson and Shuck tests are negative.
Watson test: Pain and movement of the scaphoid despite blocking its normal capacity to flex in radial deviation is an indication of scapholunate tear or laxity.
The Shuck test is performed to evaluate lunotriquetral instabilities.
A positive piano key test indicates a complete peripheral tear of the TFCC and/or dorsal radioulnar ligament tear.
Midcarpal instability can be ruled out with a negative wrist pivot shift test, as first described by Lichtman et al.10
In patients with ulnocarpal instability, the wrist assumes an ulnar-sided supination deformity similar to that seen in rheumatoid arthritis.
A key to diagnosing ulnocarpal instability is the supination test, which is a diagnostic maneuver developed by the first author. This examination is performed by stabilizing the affected DRUJ with a firm grasp while stressing the wrist in supination and volar translation.
When the wrist is loaded axially and returned through neutral in ulnar deviation, the patient’s pain is reproduced. The wrist may also “clunk” back into reduction.
The contralateral wrist is also tested for comparison.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard posteroanterior and lateral radiographs have poor diagnostic value for ulnocarpal joint instabilities but can be used to rule out scapholunate interosseous ligament (SLIL) and lunotriquetral interosseous ligament (LTIL) tears. On a pure lateral view, if there is DRUJ instability, the ulna will be dorsally positioned relative to the radius instead of being seen superimposed on the radius.
Computed tomography is useful for visualizing joint congruity and fractures as well as subluxation or dislocation of the DRUJ.
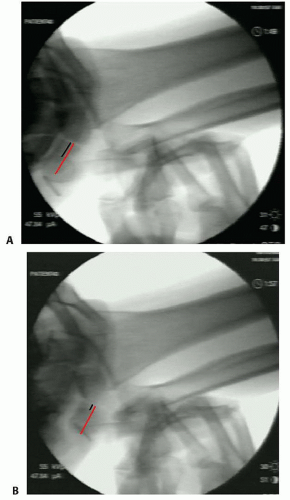
Live fluoroscopy during the supination test allows the examiner to evaluate and visualize the presence and amount of ulnocarpal joint instability (FIG 3).
The changing appearance of the triquetrum, demonstrated by its decreased length while in a position of supination, indicates ulnocarpal instability.
The pisiform’s location in relation to the triquetrum may also indicate the type of ligamentous tear or laxity by either moving together with the triquetrum during the supination test or appearing to be stationary as the triquetrum is moving.6
Triple-injection arthrography of the midcarpal row, radiocarpal joint, and DRUJ can be useful in showing SLIL or LTIL tears, TFCC tears, and ulnar-sided TFCC tears, respectively.