Extra-Articular Proximal Tibial Fractures: Submuscular Locked Plating
Mark A. Lee
Brad Yoo
INTRODUCTION
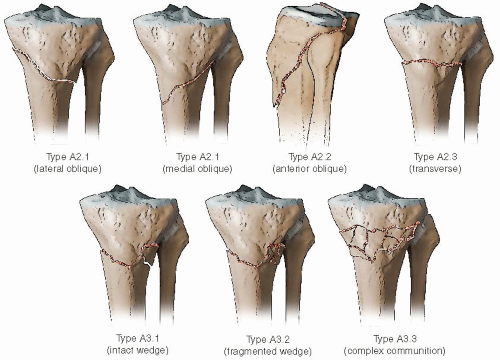
Extra-articular fractures of the proximal tibial metadiaphyseal region are uncommon injuries and are typically extensions of tibial plateau fractures. These fractures are technically challenging to treat due to the short proximal fragment and significant muscular deforming forces. In the AO/OTA classification, these fractures are classified as 31 and are geographically localized within a trapezoidal shaped area, whose dimensions equal the epiphyseal width at its widest point and narrow distally (Fig. 28.1). These fractures are usually the result of high-energy trauma such as motorcycle or pedestrian motor vehicle accidents in younger patients and fragility fractures in the elderly. With high-energy trauma, associated soft-tissue injuries are common, and with displaced and comminuted fracture patterns, the popliteal artery or trifurcation is at risk.
The management of extra-articular fractures of the proximal tibia depends upon a combination of patient-and surgeon-dependent factors. Some issues to consider are the extent of the soft-tissue injury, the fracture pattern, significant medical comorbidities or concomitant injuries, as well as the surgeon’s level of expertise and the hospital’s ability to care for critically injured patients. A patient with a minimally displaced isolated transverse fracture should be considered separately from the multiply injured patient with an open comminuted proximal tibial injury (Fig. 28.2A,B).
INDICATIONS AND CONTRAINDICATIONS
There are three absolute indications for surgery, which include an open fracture, a concomitant compartment syndrome, and fractures associated with a vascular injury. Furthermore, there are several relative indications for surgery and include residual angulation >5 degrees in the coronal plane and 7 degrees in the sagittal plane (1), patients with an ipsilateral femoral patellar or ankle fracture, and multiply injured patients. Other indications for surgery include patients that would not tolerate prolonged immobilization of the knee or ankle if treated nonoperatively.
Contraindications to internal fixation of an extra-articular proximal tibia fracture include a compromised soft-tissue envelope acutely in closed fractures or contaminated wounds in open fractures. In these cases, temporary bridging external fixation followed by delayed internal fixation has been shown to decrease the rate of deep infection (2). Additional contraindications include active infection in the extremity and a subgroup of patients with severe medical comorbidities that preclude a surgical procedure.
 FIGURE 28.2 Proximal extra-articular fractures demonstrate extreme variability from high energy, highly displaced (A) to lower energy, minimally displaced patterns (B). |
History and Physical Examination
In the cooperative patient, a detailed history may provide important information regarding the mechanism of injury, and important medical comorbidities such as diabetes, cancer, or autoimmune diseases should be noted.
The patient’s medication list should be examined for items such as anticoagulants or immunosuppressive agents. A history of prior fracture or previous orthopedic interventions is also important in preoperative planning.
The evaluation of the injured patient begins with the advanced trauma life support protocols, which proceeds systematically with airway management, cardiopulmonary resuscitation, and spine precautions. Once life-threatening issues have been addressed, a secondary survey of the musculoskeletal system is completed. Although this evaluation includes an assessment of the spine, pelvis, and all four extremities, only the evaluation of the lower extremity will be discussed.
The patient is fully exposed, and a visual inspection of the limb for open wounds, limb deformity, and degree of soft-tissue damage is performed. Pulses are palpated, with particular attention to asymmetry between sides. The posterior cortex of the proximal tibia is in close proximity with the popliteal artery and tibioperoneal trunk, and displaced fractures in this region may cause a laceration, thrombosis, or traction injury to these structures (Fig. 28.3). If pulses are absent or asymmetric, gross realignment of the limb with gentle traction frequently improves perfusion. Measurement of an ankle-brachial index (ABI) provides a rapid, objective assessment of vascular impairment. An ABI lower than 0.9 alerts the surgeon to a potential vascular injury (3). If further investigation of the arterial supply is warranted, angiography or computed tomography (CT) angiography should be performed. A detailed neurological examination should also be performed and documented.
High-energy proximal tibial fractures are associated with an increased risk of compartment syndrome. Hallmark signs include pain out of proportion to the injury, pain with passive stretch of the muscles within the compartment, and a tense swollen leg. In some instances, an assessment of the patient’s pain is not possible due to sedation, intoxication, or a head injury. In these circumstances, direct measurement of intracompartmental pressures should be performed. A difference of 30 mm Hg between the measured compartment pressure and the diastolic pressure (delta p) has been shown to correlate closely with the need for fasciotomy (4). Since muscle damage occurs as early as 2 hours, prompt diagnosis and surgical intervention may prevent long-term functional disability. Displaced fractures in the proximal tibia are associated with an increased rate of compartment syndromes, since most of the lower legs muscle mass is located proximally (5).
Because of the subcutaneous location of the tibia, open fractures are common and require timely operative débridement and irrigation (6). Sterile dressings and a long leg splint or knee immobilizer should be applied until an operating room becomes available. Both tetanus toxoid and a first-generation cephalosporin are indicated, with the addition of penicillin in grossly contaminated wounds to prevent a clostridial infection. When the soft tissues have absorbed a high amount of kinetic injury following fracture, microvascular damage and leg swelling rapidly occur. This often results in serious or hemorrhagic fracture blisters (7). Surgical intervention should proceed only after the soft tissues have recovered, heralded by the appearance of fine skin wrinkles as well as improved mobility of the skin over the deeper dermal layers. Surgical intervention prior to soft-tissue recovery has been associated with higher rates of wound complications and deep sepsis (8).
Imaging Studies
Orthogonal anteroposterior (AP) and lateral radiographs are the basis for fracture characterization. High-quality x-rays should be obtained of the tibia-fibula as well as separate films centered over both the knee and ankle joints. The clarity of the image is greatly enhanced when the overlying splint material is removed. Traction radiographs can help elucidate fragment morphology, and the quality of reduction performed through indirect means; however, this maneuver is painful in the conscious patient. CT scans may detect the presence of an intra-articular fracture but give detailed information about fragment morphology. While the presence of concomitant injury to intra-articular soft-tissue structures (ACL, PCL) has been described in high-energy proximal tibia fracture variants, these are usually addressed on a delayed basis after fracture reduction and fixation. Exceptions are injuries to the cruciate or collateral ligaments with large bony avulsions. Magnetic resonance imaging scan may be helpful in some patients with rim avulsion fractures or fracture dislocations of the knee.
Surgical Timing
In patients with displaced proximal tibial fractures and an acceptable soft-tissue envelope, definitive internal fixation within 24 to 48 hours is safe and effective. In patients with higher energy injuries with significant softtissue swelling and blistering are admitted for further evaluation and treatment. Immediate internal fixation in this group of patients is ill advised because of the risk of wound problems and deep sepsis. In these patients, if the fracture is not comminuted and length stable, a long leg splint or knee immobilizer can be used as temporary stabilization while waiting for soft-tissue recovery. When fine skin wrinkles return, soft-tissue swelling resolves, and the skin is mobile on the deeper structures, surgery can be performed. In many patients, this takes several weeks. On the other hand, in patients with fracture blisters or severe open wounds or the fracture is comminuted and unstable, application of a bridging external fixation is indicated. A spanning external fixator is used to maintain length and permit circumferential soft-tissue care.
Surgical Tactic
The size of the proximal segment and the amount and location of fracture comminution influence the type of implant and the method of insertion. There are two internal fixation devices that can be utilized for definitive treatment of an extra-articular tibial fracture and include plate osteosynthesis or an intramedullary nail. There are advantages and disadvantages with each of these implants, and the use of one device over another varies among surgeons as there is little level I or II evidence supporting a specific technique.
Intramedullary nailing of proximal tibial fractures is a technically difficult procedure (10). Standard tibial nailing often leads to a malreduction in valgus with an anterior apex. Semiextended or suprapatellar approaches have been used to improve fracture alignment but the impact of these techniques on the periarticular soft tissues and articular cartilage is not clear. The use of blocking screws has also been shown to minimize deformities with nailing proximal fractures. When using an intramedullary nail, modern implants that provide multiple proximal axial fixation options are important.
In the past decade, anatomically designed periarticular plates have been developed specifically for the proximal tibia. These plates combine the use of conventional and locking screws with the ability for submuscular placement. The enlarged upper end of the plate allows multiple screws to be placed in the short proximal segment. The plate remains extra-articular minimizing a potential source of postoperative knee pain (Figs.28.4 and 28.5). Plate length should be determined before surgery as part of the preoperative plan. For fractures with significant comminution, long plates may be required, and these may not be part of the normal inventory. It is important to use preoperative conventional or digital templating to ensure that the plate will achieve three to four bicortical points of fixation distal to the fracture.
SURGICAL TECHNIQUE
Operating Room Setup
Preoperative planning and proper operating room setup improve the surgical procedure. The patient is positioned supine on a fully radiolucent table. The fluoroscopy machine is placed on the side opposite of the injury. A bump is placed under the ipsilateral hip to internally rotate the knee to a neutral position, and a tourniquet
is place on the thigh. The leg is prepped from tourniquet to toes (Fig. 28.6). Except for very simple fracture patterns, fluoroscopic images of the contralateral tibia are obtained and saved as these radiographs are important for verifying length and rotation on the injured side. In comminuted fracture patterns with metadiaphyseal extension or in cases with bone loss, we routinely drape both extremities into the surgical field to allow for intraoperative determination of limb length.
is place on the thigh. The leg is prepped from tourniquet to toes (Fig. 28.6). Except for very simple fracture patterns, fluoroscopic images of the contralateral tibia are obtained and saved as these radiographs are important for verifying length and rotation on the injured side. In comminuted fracture patterns with metadiaphyseal extension or in cases with bone loss, we routinely drape both extremities into the surgical field to allow for intraoperative determination of limb length.
 FIGURE 28.4 Some implants are contoured lower on the metaphyseal flare and are best suited for fractures with larger proximal segments. |
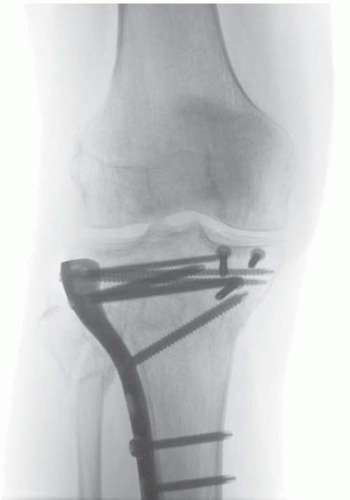 FIGURE 28.5 Fracture implants designed to fit closer to the joint line are better for small proximal fracture segments, especially when there are articular fracture extensions. |
 FIGURE 28.6 The patient is placed supine with the leg draped free. The C-arm is placed on the opposite side of the table. |
Common Intraoperative Challenges
Restoration of length and rotational reduction are challenging in comminuted fracture patterns. One simple technique is to position a cautery cord along the anatomic axis of noninjured tibia and to apply clamps at easily reproducible proximal and distal radiographic landmarks. The clamped cord segment is maintained on the sterile field until provisional reduction of the injured tibia is completed (Figs. 28.3B and 28.7A,B). The clamp and cord construct are then placed along the anatomic axis of the injured tibia and aligned against the previously utilized radiographic landmarks to determine correct restoration of length.
The lateral radiograph is more accurate for determining length intraoperatively and eliminates differences related to the amount of knee flexion seen on the AP image. Lateral imaging is critical to accurately judge fracture reduction but is frequently obstructed by the uninjured leg with single leg draping. The use of an elevated platform below the injured extremity allows for unimpeded lateral imaging and allows the extremity to remain stable during provisional reduction attempts (Fig. 28.8A-C).
Anesthesia
For acute fractures, general anesthesia is preferred to provide maximal muscle relaxation for fracture reduction and evaluate the postoperative neurovascular status. In the absence of other severe injuries, arterial lines and central venous pressure monitoring are not required. A cephalosporin antibiotic is administrated within 30 to 45 minutes of the skin incision and continued for 24 hours in closed fractures and longer in open injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree