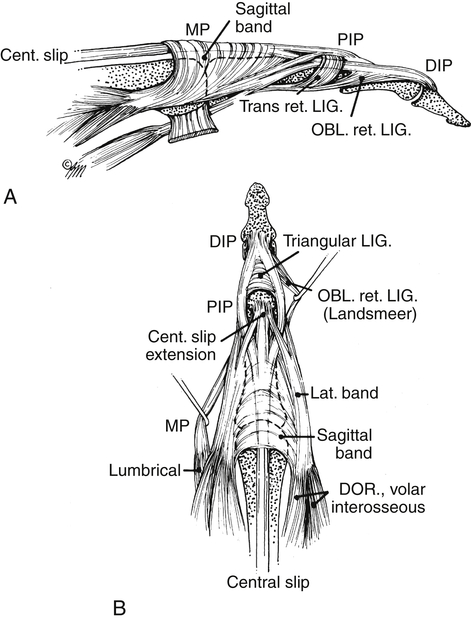
Extensor tendon injuries have long been considered to be less complex than flexor tendon injuries with fewer complications and better results. Numerous authors reflect that complications caused by extensor tendon injuries can be just as frustrating and result in significant loss of motion and function of the injured digit and hand.1–3 According to Rosenthal and Elhassan, “The extensor muscles to the digits are weaker, their capacity for work and their amplitude of glide are less than their flexor antagonists, yet they require a latitude of motion that is not necessary for flexor function”.1 Extensor tendons are more thin and broad than flexor tendons. They are superficial in comparison with the flexor tendons, allowing adhesion to the fascial layers and skin. Over the proximal phalanx, the extensor tendon has a broad tendon to bone interface that can result in dense adhesions. Shortening of the extensor tendon as a result of surgery may result in difficulty regaining full flexion. Dorsal swelling may prevent the tendons from gliding. Recreating the normal balance between the intrinsic and extrinsic muscle/tendon units can be a difficult task for the surgeon and therapist following extensor tendon injury. Common functional complications include loss of flexion, extensor lag, and decreased grip strength.2 To prevent these complications, extensor tendon approaches, similar to flexor tendon approaches, have evolved to include controlled passive and active mobilization immediately following surgery. Results, especially in the first 12 weeks, show improved outcome over immobilization.3–11 The goal of this chapter is for the reader to understand the anatomy, pathology, healing process, and rehabilitation approaches for the differing zones of the extensor tendon to achieve maximal function with minimal complications for the client following extensor tendon repair. Less attention has been given to the types of surgical repair for extensor tendons than flexor tendons. However, the strength of repair of an extensor tendon is important in preventing gapping or rupture when motion is initiated. A number of suture techniques for extensor tendons exists.1,2,12,13 Newport notes that because extensor tendons are smaller and flatter than flexor tendons and have less cross linking, performing a stronger, multi-strand repair in the extensor tendon is more difficult. The same repair technique performed in an extensor tendon is approximately 50% as strong as if it was performed in a flexor tendon due to the smaller size of the tendon and lack of collagen cross linking.1,13 The type of suture performed on the lacerated extensor tendon is largely dependent on the area the tendon was injured. The thinner area of extensor tendon (such as, in the digit) will not tolerate multiple strands required for stronger repair.1 The therapy protocols discussed in this chapter for extensor tendon injury are not dependent on the type of surgical technique used. Healing of tendons occurs from direct blood supply and synovial diffusion. The blood supply to the extensor tendons is through vascular mesenteries, which travel through the fascia to the tendons from the radial and ulnar arteries and deep palmar arch. Nutrition from synovial diffusion to the extensor tendons occurs from the deep fascial layer in the dorsum of the hand and the extensor retinaculum.1 Extrinsic extensor tendons to the digits include the extensor digitorum communis (EDC), extensor indicis proprius (EIP), EDM, EPL, extensor pollicis brevis (EPB), and abductor pollicis longus (APL). Each of these tendons crosses the wrist dorsally, passing under the extensor retinaculum, which is separated into six compartments to maximize mechanical efficiency of the extensor tendons as they cross the wrist, preventing bowstringing (Fig. 31-1). Extension of the finger PIP and distal interphalangeal (DIP) joints is performed primarily by the lateral bands, which consist of portions of the lumbrical and interossei tendons with contributions from the EDC (Fig. 31-2). The lateral bands on both sides of the fingers pass dorsal to the axis of motion at the PIP and DIP joints and merge over the DIP joint to form the terminal extensor tendon. Extension at the PIP and DIP joints is delicately balanced by a combination of tendon fibers and ligamentous support in an uninjured finger to prevent excessive dorsal or volar migration (subluxation) of the lateral bands. The transverse retinacular ligament (TRL) supports the lateral bands volarly, and the triangular ligament supports the lateral bands dorsally. The oblique retinacular ligaments (ORLs) run along the sides of the finger and cross the PIP and DIP joints volar to the PIP axis of motion and dorsal to the DIP axis of motion. Thus when the PIP joint extends, it places tension on, or stretches, the ORL. This causes the ligament to tighten across the DIP joint, placing a passive extension assist on the DIP joint by this tenodesis effect. Injuries to the extensor tendon are discussed in relation to the zone of injury, for there are different protocols following repair of the extensor tendon for each set of zones. Extensor tendon zones are reviewed in Fig. 31-3. Orthoses used for extensor tendon repairs in the early phase of tendon healing are reviewed in Table 31-1. TABLE 31-1 Overview of Orthoses Used for Extensor Tendon Repairs in the Early Phase of Tendon Healing
Extensor Tendon Injury
Surgical Repair of Extensor Tendons
Timelines and Healing
Anatomy
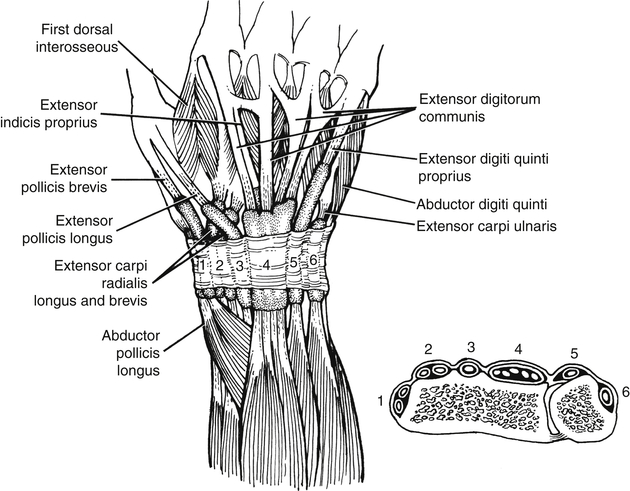
The extensor retinaculum acts as a pulley to maintain the mechanical efficiency of the extrinsic extensor tendons and prevent bowstringing. It also assists in extensor tendon nutrition via synovial diffusion. (From Fess EE: Hand and upper extremity splinting: principles and methods, ed 3, St Louis, 2005, Mosby.)
Zone of Injury
Immobilization
Immediate Passive Extension
Immediate Active Extension
I and II
III and IV
V, VI, and VII
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
