Extensor Tendon Centralization following Traumatic Subluxation at the Metacarpophalangeal Joint
Byung J. Lee
Ross J. Richer
Craig S. Phillips
DEFINITION
Instability of the extensor digitorum tendons at the metacarpophalangeal (MCP) joint has been subdivided into two categories: subluxation and dislocation.
Subluxation of the extensor digitorum tendons at the MCP joint is defined as lateral displacement of the tendon with its border reaching beyond the midline but remaining in contact with the condyle during full MCP joint flexion.
Dislocation describes the condition in which the extensor tendon is located in the groove between the metacarpal heads.14
Instability of the extensor digitorum tendons at the MCP joint usually occurs in patients with underlying inflammatory conditions (ie, rheumatoid arthritis).
Traumatic injury to the sagittal bands, particularly the radial sagittal band, can cause instability of the extensor tendon. Although ulnar-sided injuries have been reported, the overwhelming majority of injuries occur to the radial sagittal band.
Instability of the extensor tendon is relatively rare in nonrheumatoid patients.
The sagittal bands are sometimes referred to as the shroud ligament because of the way they cover, or wrap, the MCP joint.
Sagittal band injuries are classified as type I, II, or III, depending on the degree of extensor tendon instability.14
Traumatic extensor tendon subluxation at the MCP joint level is classified as type II injury; dislocation is type III. These injuries have been given the eponym “boxer’s knuckle.”6
Not all injuries to the sagittal bands result in extensor tendon subluxation. Clinical examination will identify those patients in which extensor tendon instability has occurred.
Factors influencing treatment include symptoms and time elapsed since injury.
ANATOMY
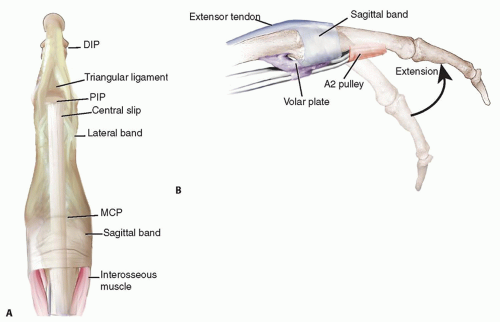
The digital extensor mechanism at the level of the MCP joint consists of the extensor tendon, sagittal bands, and volar plate. The sagittal bands are part of a complex extensor retinacular system that includes the triangular ligament between the lateral bands, the transverse retinacular ligament, and the oblique retinacular ligament at the proximal interphalangeal (PIP) joint level (FIG 1A).
The sagittal bands are dynamic structures that envelop the extensor tendons, centering them over the MCP joint during flexion, preventing bowstringing during hyperextension, and controlling tendon excursion. The sagittal bands insert onto the volar plate overlying the MCP joint (FIG 1B).15
The sagittal bands are the primary stabilizers of the extensor digitorum tendons at the MCP joints, and their integrity is essential for normal extensor tendon function.12,15,17,20
When the MCP joint is maintained in neutral extension, the sagittal bands are oriented perpendicular to the tendon.
The sagittal bands are anatomically and physiologically distinct from the deeper collateral ligaments.
The radial sagittal band is often thinner and longer than its ulnar counterpart.
The greatest tension on the sagittal bands occurs with wrist and MCP flexion and radioulnar deviation.
The lumbrical muscles function to flex the MCP joint and extend the interphalangeal (IP) joint through the lateral bands. They originate on the flexor digitorum profundus (FDP) tendon and traverse on the radial aspect of the digit inserting into the extensor expansion.
The intermetacarpal ligaments are stout ligaments that originate and insert on adjacent metacarpal necks. These ligaments pass dorsal to the lumbrical tendons and volar to the interosseous tendons.
PATHOGENESIS
The mechanism of sagittal band injury commonly involves a direct blow to a flexed MCP joint.
Injury may result indirectly from forced flexion or directly from shear forces across the sagittal band.
Other described mechanisms include forceful deviation of the digit against resistance, usually with the MCP joint extended.
In open injuries, the sagittal band is usually lacerated.
Sometimes, laceration of the junctura tendinum can also lead to extensor tendon subluxation.
Extensor tendon subluxation typically occurs with at least 50% disruption of the proximal sagittal band.20 The extensor tendon no longer remains centralized over the MCP joint through flexion but rather subluxates ulnarly.
It has been suggested that frequency of injury among the digits is related to the cross-sectional diameter of the sagittal band, the extent of distal attachment, and the length of the sagittal band.7,14,15 The long finger is most commonly injured.
It has been suggested that traumatic subluxation occurs when there is tearing of both the superficial and deep layers of the sagittal band enveloping the extensor tendon.8
When underlying inflammatory conditions are present, the sagittal bands become attenuated and atrophic, allowing for atraumatic subluxation of the extensor tendons into the troughs (usually ulnar) between metacarpal heads.
NATURAL HISTORY
Symptoms from acute injuries typically resolve within 3 weeks with appropriate treatment. However, pain can persist for up to 9 months before fully dissipating.6
When sagittal band injuries associated with discomfort, swelling, and subluxation are neglected, patients will experience ongoing symptoms that may worsen over time. The extensor tendon may become fixed in the valley between the metacarpal heads, leading to loss of MCP extension and deviation of the digit. These patients will require surgical treatment for resolution of their symptoms.7,14,16
PATIENT HISTORY AND PHYSICAL FINDINGS
This chapter deals with traumatic subluxation. Treatment protocols for inflammatory subluxation differ and are beyond the scope of this chapter.
A critical aspect of treatment involves understanding the circumstances surrounding the injury. This information will help identify those at risk for infection in open injuries (eg, clean laceration, fight bite) or the possibility of underlying systemic disease contributing to closed injuries caused by low-energy trauma.
Shortly after injury, soft tissue swelling may obscure the alignment of the tendon over the MCP joint.
Initially after traumatic injury to the sagittal bands with subsequent extensor tendon instability, symptoms and signs include the following:
Localized pain
Swelling over the involved MCP joint
Limited motion (FIG 2A)
Limited or deviated MCP joint extension or both (FIG 2B)
Weak MCP extension
A potentially painful snapping of the tendon over the MCP joint with active flexion (FIG 2C)
Ulnar deviation deformity and difficulty adducting (or abducting in the case of the index) the affected finger
Chronic cases of tendon instability often exhibit pain during MCP joint flexion, such as during grip, along with localized tenderness and swelling over the injured sagittal band.16
MCP extension can be actively maintained when the joint is passively placed into extension; however, difficulty is usually encountered when attempts are made to extend the MCP joint from flexion or when flexing the MCP joint from full extension.
Methods for examining extensor tendon instability over the MCP joint include the following:
Assess sagittal bands throughout MCP range of motion.
Assess swelling, open injuries, and so forth. Determine location of pathology.
Palpate over the MCP joints and in the groove between the metacarpal heads.
Sagittal band injuries will exhibit pain with superficial palpation. In contrast, pain associated with collateral ligament injury is usually deeper, within the groove between the metacarpal heads.
Perform tendon and ligament instability examination.
Ask the patient to flex the MCP joint and wrist. This position places the maximum amount of ulnar force on the extensor tendon at the MCP joint. This will help to determine the amount of instability.
Pain provocation test: With the distal and proximal IP joints extended and the MCP joint flexed, ask the patient to try to extend the MCP joint against resistance.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A standard radiographic series, including posteroanterior, lateral, and oblique views of the MCP joint.
These views will exclude any mechanical or bony pathology limiting extension of or predisposing the sagittal band to dislocate.
A Brewerton view (anteroposterior [AP] view with dorsal surface of the fingers touching the cassette and the MCP joints flexed 45 degrees) or stress views may be needed to rule out collateral ligament avulsion injury.
Magnetic resonance imaging (MRI) has been used with success to identify patients with sagittal band injuries, especially when the physical examination is obscured by swelling and patient discomfort.13 MRI with the injured MCP joint flexed facilitates the diagnosis.
Acute injuries demonstrate morphologic and signal intensity abnormalities within and around the sagittal bands on axial T1- and T2-weighted images, together with poor definition, focal discontinuity, and focal thickening.4
Dynamic ultrasound has been reported as a useful modality for diagnosis of extensor tendon subluxation when swelling obscures the physical examination.11
DIFFERENTIAL DIAGNOSIS
MCP joint collateral ligament injury
Trigger finger
Ulnar nerve palsy
Congenital sagittal band deficiency
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree