Extended Trochanteric Osteotomy
Neil Sheth
P. Maxwell Courtney
Wayne G. Paprosky
BACKGROUND
Removal of well-fixed femoral components has long been a challenge for the orthopedic surgeon in revision total hip arthroplasty (THA). Disrupting the bone-implant interface using standard techniques can be time consuming and potentially result in damage to the proximal femur. Wagner (1) first described in 1989 an anterior trochanteric osteotomy to facilitate removal of the femoral component. His reported technique involved making an extended anterior osteotomy of the greater trochanter, reflecting the anterior half of the abductors in continuity with the anterior aspect of the proximal femur. A modification of this technique, popularized by Younger and Paprosky, involved making a lateral trochanteric osteotomy and reflecting the abductors and vastus lateralis soft tissue attachments as a single continuous sleeve with the proximal lateral third of the femur (2). The extended trochanteric osteotomy (ETO) has become the workhorse for providing adequate surgical exposure for both revision and complex primary THA (3,4,5).
INDICATIONS
The ETO results in a controlled fracture of the proximal femur. The most common indication for utilization of the ETO is to facilitate removal of a well-fixed, extensively porous coated or diaphyseal fitting stem. The ETO is also a useful adjunct for removing a well-fixed proximal fitting stem when disruption of the bone-implant interface cannot be achieved adequately from the shoulder of the prosthesis or the calcar region adjacent to the prosthesis. Occasionally, proximal fitting prostheses may also exhibit bone ongrowth onto the distal titanium portion of the stem, making removal very challenging without the use of an ETO.
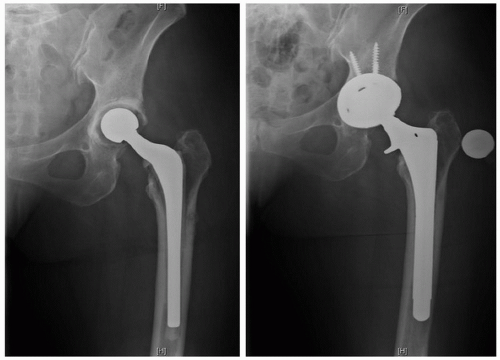
Indications also include removal of cement following extraction of a cemented femoral stem, removal of a well-fixed stem in the setting of periprosthetic infection, treatment of periprosthetic femur fractures treated with femoral component revision, and directly accessing the diaphysis for reconstruction in the setting of proximal varus femoral remodeling where stem placement without an ETO may fracture the greater trochanter or result in varus stem position (6,7,8). Figure 5-1 demonstrates the radiographs of a patient who underwent revision THA after periprosthetic infection. Using an ETO could have prevented the revision stem from being placed into varus. When compared with more limited approaches, the ETO has a lower rate of femoral (shaft) fracture, inadvertent femoral perforation, and cement retention (9).
In cases of complex primary THA, the ETO can also be performed prophylactically in cases with significant proximal femoral deformity allowing for protection of the greater trochanter in a controlled manner. In addition, more enhanced acetabular exposure can be obtained in both the primary and revision setting with an ETO (10).
Relative contraindications to use of an ETO include severe osteolysis of the proximal femur and implantation of a cemented stem, whether or not it is in conjunction with impaction grafting. Limited clinical data suggest a higher nonunion rate in patients who undergo impaction grafting after ETO, secondary to cement extrusion at the osteotomy site preventing bony union (11).
PREOPERATIVE PLANNING
Preoperative planning is essential for successful outcomes in both the setting of primary and revision THA. The surgeon should include as part of the preoperative plan the likelihood of requiring an ETO and at what step of the procedure it will be performed (before or after hip dislocation). If an osteotomy is planned as part of the operative procedure, the length of the osteotomy must be carefully predetermined. There are conflicting goals to be considered when planning the length of the osteotomy. The goal should be to select an osteotomy length that allows for adequate visualization and performance of the task at the hand (e.g., removal of a well-extensively porous-coated stem) while at the same time leaving enough intact diaphysis for stem fixation. The chosen length of the osteotomy should render at least 4 to 6 cm of isthmic diaphyseal fit for the revision femoral component chosen for reconstruction especially if the revising stem planned is an extensively
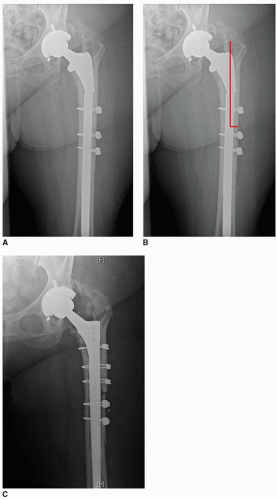
porous-coated cylindrical distal body stem. Tapered distal body revision stems require less diaphysis for fixation (12). The osteotomy length is usually at least 10 cm long, with most femoral revision osteotomies measuring between 12 and 15 cm in length (13). The length of the osteotomy should be measured from the tip of the greater trochanter. The osteotomized fragment should be long enough to provide enough distance over which two cerclage cables can be utilized for fixation (Fig. 5-2).
porous-coated cylindrical distal body stem. Tapered distal body revision stems require less diaphysis for fixation (12). The osteotomy length is usually at least 10 cm long, with most femoral revision osteotomies measuring between 12 and 15 cm in length (13). The length of the osteotomy should be measured from the tip of the greater trochanter. The osteotomized fragment should be long enough to provide enough distance over which two cerclage cables can be utilized for fixation (Fig. 5-2).
While most osteotomies are performed following THA dislocation, patients with periprosthetic fractures, femoral component subsidence, or significant heterotopic ossification about the proximal femur may benefit from undergoing the osteotomy prior to dislocation. The osteotomy can be performed either before or after stem removal. While it is technically most facile to perform the ETO after the stem has been removed, it is often not possible if the component is well fixed.
SURGICAL TECHNIQUE
Prepping, Draping, and Patient Positioning
Most commonly, preoperative general anesthesia is administered for these procedures since they can be lengthy in nature. A Foley catheter is placed prior to final patient positioning. Patients undergoing an ETO are typically placed in the lateral decubitus position in order to access the hip through a posterior approach. However, an ETO through an anterolateral approach has also been described (14).
A series of positioners are used to maintain the patient’s lateral position, making sure to keep the pelvis level, without excessive flexion or extension and without excessive anterior or posterior rotation. Foam padding is placed under the down leg to protect all bony prominences (fibular head and lateral malleolus), and the down leg should be taped down in order to use the heels and the knees as a reference for leg length following reconstruction (Fig. 5-3). The operative limb is elevated and held in position until it is properly prepped with a soap solution and then with chlorhexidine.
Following sterile prepping, the operative limb is draped in standard fashion using a series of stockinettes, Cobaan, U-drapes, and sterile hip drapes, making sure to leave a widely prepped area to allow for adequate surgical exposure. Iodine-impregnated sheets (Ioban) are typically used to cover the exposed skin of the operative hip making sure to avoid any exposed skin while mobilizing the limb during the procedure.
Surgical Approach—Posterior Approach
An incision is marked out over the posterior one-third of the greater trochanter with a slight posterior curve as it extends proximally beyond the tip of the greater trochanter (Fig. 5-4). A previous incision may be incorporated; however, a new incision can be made if necessary without compromising the blood supply to the soft tissue sleeve due to vascular redundancy and robust anastomoses surrounding the hip. Sharp dissection is taken down to the fascia, and a fascial incision is made in line with fibers of the fascia and the underlying gluteus maximus. A Charnley retractor is placed making sure that the posterior blade is not too deep, which may put the sciatic nerve at risk of injury. The gluteus maximus femoral insertion is identified (Fig. 5-5) and recessed in the setting of revision THA to minimize posterior tethering of the femur. A posterior capsular approach is performed following the posterior border of the vastus lateralis and the posterior border of the gluteus medius, along the capsular and short external rotator attachment to the posterior greater trochanter/piriformis fossa (Fig. 5-6). The capsule is tagged with a series of no. 5 caliber suture (e.g., Ethibond). The hip is dislocated in a controlled manner using a bone hook after adequate scar excision has been performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree