Excision of Tarsal Coalitions
Steven L. Frick
PRESENTATION/INDICATIONS/CONTRAINDICATIONS
A tarsal coalition is the abnormal persistence of a connection or fusion of two bones in the hindfoot and/or midfoot. Coalitions represent a failure of segmentation of tarsal bones and most commonly occur between the talus and calcaneus or the calcaneus and navicular. They typically are asymptomatic until late childhood or early adolescence, when the cartilaginous connection begins to ossify. Mosca has described this as the transitional period from synchondrosis to synostosis. Pain typically occurs at the site of the coalition but may be present in other areas of the foot. Patients typically present complaining of pain with increased activity. Coalitions can occur bilaterally, and occasionally, there is more than one coalition in the same foot. Because the coalition causes a limitation in hindfoot and midfoot motion, patients may present complaining of recurrent ankle sprains, as stress that would normally be absorbed by subtalar motion is transferred to the ankle joint during activities (Figs. 28-1 and 28-2). Excision of a tarsal coalition is indicated when nonsurgical management fails to relieve pain. Nonsurgical management typically involves immobilization in a cast or walker boot for 4 to 6 weeks, followed by the use of supportive, cushioning orthotics. Some authors do not believe in nonsurgical management of symptomatic tarsal coalitions. Contraindications to excision are asymptomatic coalitions, extensive coalitions with inadequate articular surfaces to restore motion if excised, and coalitions associated with substantial articular degeneration. Relative contraindication is the presence of substantial associated deformity where the deformity is believed to be the cause of the pain.
PREOPERATIVE PLANNING
Preoperative assessment involves documentation of limited subtalar motion, noting the degree of deficiency compared to the contralateral foot in unilateral cases or estimating the percentage of lost motion from normal eversion and inversion of the subtalar joint for bilateral cases. As patients with tarsal coalitions may develop compensatory motion at adjacent joints, learning examination techniques to try to isolate evaluation of hindfoot motion from midfoot and forefoot motion is important but is difficult and imprecise because of the normal coupling or linkage of these motions. An important part of preoperative planning involves setting patient expectations for the postoperative outcome and should not involve promises that normal hindfoot and midfoot motion will be restored by excision. Based on available studies and reported surgeon experience, excision of calcaneonavicular coalitions seems to produce more improvement in motion than do talocalcaneal excisions, but the lack of a precise, reliable, and reproducible method of measuring motion limits our ability to state this conclusively. The goals of the surgery are to relieve symptoms and to improve but not normalize motion. At presentation, patients will typically be noted to have limited subtalar inversion and eversion, and some patients will have reflexive spasm of the peroneal muscles (“peroneal spastic flatfoot”), although muscle spasms are not universal. Mubarak has emphasized the underappreciated loss of foot plantar flexion motion seen in patients with calcaneonavicular coalitions.
Preoperative planning for calcaneonavicular coalitions involves a radiographic assessment of the foot to make sure that there are not other coalitions present. The lateral column oblique view will
best show the coalition (Fig. 28-3). On the lateral view, “beaking” of the anterior process of the calcaneus is often evident. An axial view of the hindfoot can be used to assess for an associated middle facet talocalcaneal coalition (Fig. 28-4), but typically, computed tomography or magnetic resonance imaging is preferred to assess the foot for a second coalition prior to surgical treatment.
best show the coalition (Fig. 28-3). On the lateral view, “beaking” of the anterior process of the calcaneus is often evident. An axial view of the hindfoot can be used to assess for an associated middle facet talocalcaneal coalition (Fig. 28-4), but typically, computed tomography or magnetic resonance imaging is preferred to assess the foot for a second coalition prior to surgical treatment.
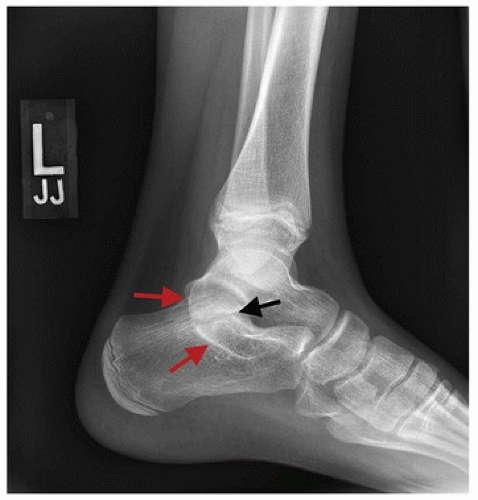
 FIGURE 28-2 Another patient with a history of recurrent ankle sprains found to have a nonunion of medial malleolus fracture associated with a calcaneonavicular coalition. |
 FIGURE 28-3 The lateral column oblique radiographic view shows the calcaneonavicular coalition best between the black arrows. |
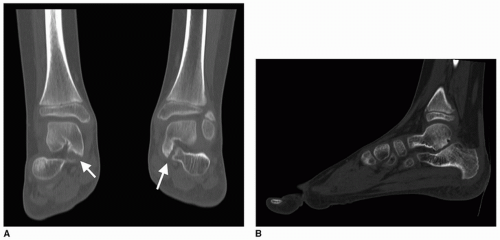
Plain radiography for talocalcaneal coalitions is helpful to evaluate foot alignment and suggest the diagnosis (Figs. 28-5A, B and 28-6). Advanced imaging is critical for preoperative planning of talocalcaneal tarsal coalition excision. Computed tomography is the favored imaging, as it allows for assessment of the foot for a second tarsal coalition and importantly provides an assessment of the extent of the tarsal coalition involvement of the middle and posterior facets (Fig. 28-7). It also allows for evaluation of the hindfoot and midfoot alignment, as well as the thickness and quality of the articular surfaces. In situations where there is not much normal-appearing articular cartilage in the posterior facet, or when the posterior facet is narrowed with subchondral irregularities and cysts, then arthrodesis may be preferred rather than coalition excision. The entire computed tomography series should be viewed, although the author finds the coronal reconstruction most helpful to evaluate the three CT imaging criteria listed by Torode as indications for isolated talocalcaneal coalition
resection: these are (a) size of the middle facet coalition less than 50% of the size of the posterior facet, (b) articular cartilage thickness of the posterior facet equal to the thickness of the tibiotalar articular thickness, and (c) less than 16 degrees of hindfoot valgus. Three-dimensional reconstructions can be helpful in preoperative planning to assess the width and position of the coalition (Fig. 28-8), with a classification outlined by Mubarak. Magnetic resonance imaging can also be used.
resection: these are (a) size of the middle facet coalition less than 50% of the size of the posterior facet, (b) articular cartilage thickness of the posterior facet equal to the thickness of the tibiotalar articular thickness, and (c) less than 16 degrees of hindfoot valgus. Three-dimensional reconstructions can be helpful in preoperative planning to assess the width and position of the coalition (Fig. 28-8), with a classification outlined by Mubarak. Magnetic resonance imaging can also be used.
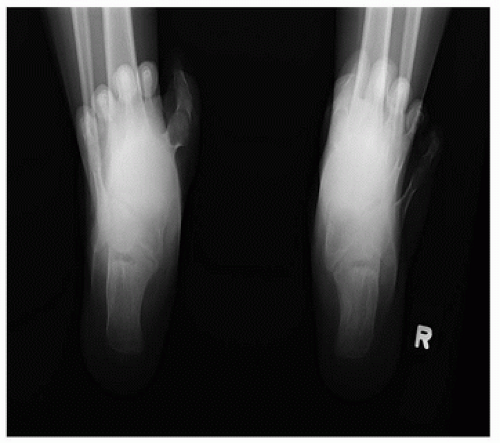
 FIGURE 28-5 A, B. Standing anteroposterior and lateral radiographs of patients with talocalcaneal coalitions often show flatfoot deformity. |
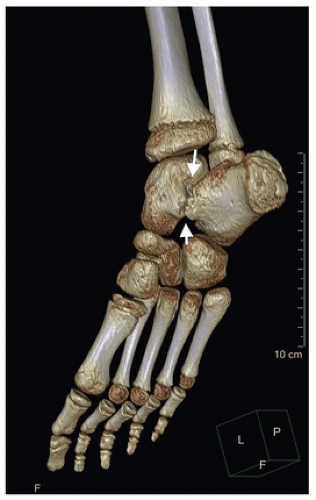 FIGURE 28-8 3D computed tomography allows for preoperative assessment of morphology and location of middle facet coalitions (white arrows). |
A controversial area in the assessment of tarsal coalitions is the degree of flatfoot deformity. Classically, tarsal coalitions are described as a potential cause of a rigid flatfoot deformity. In occasional patients, the flatfoot/eversion will be related to reflexive, protective spasm of the peroneal muscles holding the foot in maximal eversion, and the flatfoot deformity will be improved when
removing the symptomatic coalition results in resolution of spasm and return to a more neutral subtalar joint position. Much more commonly, the associated flatfoot deformity is established and structural and will persist after coalition resection unless a concomitant or staged deformity correction is performed. Whether or not tarsal coalition excision should be combined with a surgical procedure to correct flatfoot deformity is dependent on multiple factors, including the patient age, size, location of the patient’s pain, and particularly the degree of deformity (see Mosca, 2014). Assessment of the severity of flatfoot deformity is not standardized but typically includes clinical and radiographic analysis. Some authors have used computed tomography assessment of hindfoot valgus as a decisive method and recommend hindfoot reconstruction in patients with greater than 16 degrees of valgus on coronal computed tomography imaging. In the setting of severe flatfoot deformity and a tarsal coalition, some authors recommend staged procedures, with treatment of the tarsal coalition with excision as a first stage. Later, flatfoot reconstruction is performed if symptoms are not relieved by coalition excision. Other authors report simultaneous surgical treatment with excision of the tarsal coalition combined with flatfoot reconstructive surgery. An additional consideration is the potential for worsening of the flatfoot deformity after talocalcaneal coalition resection, as the coalition may be serving as a medial tether. Removal of the tether may result in further calcaneal eversion and valgus.
removing the symptomatic coalition results in resolution of spasm and return to a more neutral subtalar joint position. Much more commonly, the associated flatfoot deformity is established and structural and will persist after coalition resection unless a concomitant or staged deformity correction is performed. Whether or not tarsal coalition excision should be combined with a surgical procedure to correct flatfoot deformity is dependent on multiple factors, including the patient age, size, location of the patient’s pain, and particularly the degree of deformity (see Mosca, 2014). Assessment of the severity of flatfoot deformity is not standardized but typically includes clinical and radiographic analysis. Some authors have used computed tomography assessment of hindfoot valgus as a decisive method and recommend hindfoot reconstruction in patients with greater than 16 degrees of valgus on coronal computed tomography imaging. In the setting of severe flatfoot deformity and a tarsal coalition, some authors recommend staged procedures, with treatment of the tarsal coalition with excision as a first stage. Later, flatfoot reconstruction is performed if symptoms are not relieved by coalition excision. Other authors report simultaneous surgical treatment with excision of the tarsal coalition combined with flatfoot reconstructive surgery. An additional consideration is the potential for worsening of the flatfoot deformity after talocalcaneal coalition resection, as the coalition may be serving as a medial tether. Removal of the tether may result in further calcaneal eversion and valgus.
SURGICAL PROCEDURE
Excision of a Calcaneonavicular Coalition
Patient is positioned supine with a tourniquet on the thigh and a bump underneath the ipsilateral hip to internally rotate the lower extremity and allow access to the lateral foot.
The entire lower extremity is prepped and draped to include the buttock for harvest of interpositional fat graft from the buttock crease region via a transverse incision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree