Evaluation of Painful Total Hip Arthroplasty
Michael J. Archibeck
Joshua T. Carothers
Krishna R. Tripuraneni
Richard E. White Jr
Case of a Painful Total Hip Replacement
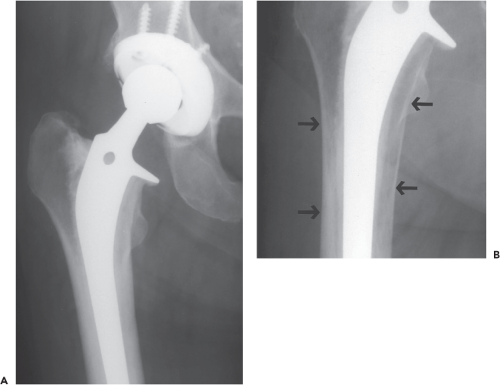
A 58-year-old male underwent metal-on-metal (MOM) total hip replacement 4 years ago and presents with worsening pain and a slowly progressive limp. The first 3 years after the replacement he was asymptomatic. He denies fever or chills. He walks with a slight Trendelenburg gait. He has mild pain on extremes of motion. There is a sense of fullness in the lateral aspect of the hip and the groin. Otherwise the examination is unremarkable. His radiographs demonstrate a normal appearing MOM total hip replacement (Fig. 81.1).
Further workup and findings are presented at the conclusion of the chapter.
Introduction
Pain is a very common complaint in patients with a total hip arthroplasty (THA). Kavanagh et al. (1) reported pain in 25% of patients at 1 year and 20% of patients at 5, 10, and 15 years after cemented total hip replacement. Patients with cementless total hip replacements also have a significant incidence of pain if questioned carefully (2). Although the pain is not always severe, it can be limiting in many patients to the extent that careful evaluation is required.
Intrinsic and Extrinsic Causes
The etiology of pain about a THA is generally categorized as arising from causes that are intrinsic or extrinsic to the arthroplasty. The intrinsic causes that are most commonly considered are mechanical loosening and sepsis. Other intrinsic causes of pain include prosthetic failure, particulate-induced synovitis, adverse local tissue reaction (ALTR) to metallic or corrosion particulates, occult fracture, and cementless femoral component thigh pain without loosening. Extrinsic causes of pain can include lumbar spine disease such as spinal stenosis (3), lumbar disc disease (4), trochanteric bursitis, trochanteric nonunion (5), claudication, abdominal aortic aneurysm, sciatic (6) or obturator nerve (7) impingement, abductor or iliopsoas tendonitis (8), stress fractures of the pubic ramus (9), and heterotopic bone, especially during the process of maturation (Table 81.1) (10).
A careful history and physical examination often contribute the most important information to making the appropriate diagnosis, being especially critical in differentiating extrinsic from intrinsic causes of pain. In addition to the history and physical examination, a thorough evaluation of the painful THA may include laboratory tests, plain radiographs,
aspiration for histologic, microbiologic and cell count, evaluation of the cross-sectional anatomy with ultrasound or metal artifact reduction sequence (MARS) MRI and occasionally nuclear medicine evaluations.
aspiration for histologic, microbiologic and cell count, evaluation of the cross-sectional anatomy with ultrasound or metal artifact reduction sequence (MARS) MRI and occasionally nuclear medicine evaluations.
Table 81.1 Classification of Potential Sources of Pain Following THA | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
History
The history gives valuable clues to the source of pain about a THA. The location, mode and timing of onset, severity, and character of the pain are all important variables. Both groin pain and deep buttock pain can be associated with acetabular or capsular sources of pain. Groin pain can also be caused by iliopsoas tendinitis or inflammation of surrounding soft tissues. Buttock pain is more commonly caused by arthritic changes of the lumbar spine or sacroiliac joint resulting in a radiculopathy. Femoral component issues usually present with anterior thigh pain. Posterior buttock and thigh pain, especially when associated with extension distal to the knee, is usually related to lumbar spine disease. Pain over the greater trochanter implicates trochanteric bursitis, abductor tendinitis or tear, trochanteric nonunion, or painful trochanteric hardware.
Temporal relationships may aid in the diagnosis as well. If there has been a pain-free period after the THA, the late onset of pain suggests loosening, wear-associated issues, or sepsis. Failure to achieve resolution of the preoperative symptoms after surgery suggests that an extrinsic source may be the source of the pain as the preoperative diagnosis of hip arthritis may have been incorrect.
If pain increases in severity with increased walking or standing and is relieved by rest, it is usually associated with loosening, but loosening is rarely associated with rest pain alone. This constellation of symptoms can also be caused by spinal claudication. Night pain, rest pain, or constant pain can be associated with sepsis or soft tissue inflammation such as trochanteric bursitis (11). Knowledge of the postoperative clinical course may assist in making the diagnosis. Delayed wound healing, the use of postoperative oral antibiotics for drainage, prolonged febrile course, or constant pain after surgery raise suspicion for sepsis.
Start-up pain, produced when starting to walk after having been seated or resting, is thought to be typical for loosening or significant micromotion in cementless THA, but it can also be caused by iliopsoas tendinitis or bursitis (if the pain is lateral or anterior) or lumbar spine disease (if the pain is posterior). Pain associated with loosening is often described as significant pain with the first several steps that improves slightly with further ambulation. However, it tends to worsen as the patients continue to ambulate.
The severity and character of the pain may contribute to determination of the diagnosis. Pain secondary to loosening may be severe but is always improved by rest. It rarely has a constant nature. Constant pain at rest points to sepsis or a neurologic cause. The lumbar spine should be investigated if the pain has neurologic features such as radiation below the knee, weakness, numbness, paresthesias, or dysesthesias. Lumbar spine disease is common in patients with hip arthritis and spinal stenosis, mechanical low back pain, radiculopathy, and neuropathy should be considered. Spinal stenosis symptoms may not have been evident before the surgery because walking was so limited and may only become symptomatic after total hip replacement (3). The contribution of the lumbar spine to the pain syndrome is the most difficult to quantify and the most easily missed diagnosis.
Physical Examination
A thorough physical examination of the hip is critical in the evaluation of the painful THA. The patient’s gait should be carefully evaluated. Limp and abductor weakness are common with the intrinsic causes of pain. The presence of a normal gait and a negative Trendelenburg test suggest that the source of pain is other than the THA. Neurologic abnormalities and leg-length discrepancies can cause or contribute to a gait abnormality. A leg-length discrepancy may be a true discrepancy or an apparent discrepancy related to abduction or adduction contracture, or to scoliosis of the lumbar spine.
Range of motion of the hip can be revealing. Pain with or inability to perform an active straight leg raise is suggestive of intrinsic pain. Pain throughout a passive range of motion suggests sepsis. Pain at extremes of motion suggests loosening. A gradual loss of internal rotation can be indicative of loosening as the femoral component often loosens into a retroverted position. Pain in certain reproducible positions suggests instability or impingement. The patient cannot always perceive subluxation but will avoid motions that cause pain from impingement against inflamed capsule or soft tissue structures. Trochanteric bursitis and tendinitis can often be diagnosed by direct palpation and resistive muscle testing. Careful muscle testing can clearly diagnose abductor or iliopsoas tendinitis. Firm compression or palpation of the pelvis, especially the pubic ramus, can detect sacroiliac disease or raise the possibility of pubic ramus stress fracture.
The physical examination should evaluate two important extrinsic causes of pain—the lumbar spine and the vascularity of the lower extremity. Neurologic sources of pain include the femoral, sciatic (6), and obturator nerves (7). Evaluation of peripheral pulses and skin temperature can usually adequately evaluate vascularity; imaging and
perfusion studies can give additional objective information in equivocal cases.
perfusion studies can give additional objective information in equivocal cases.
The evaluation of a painful MOM hip replacement or resurfacing requires some unique considerations. These include issues related to metallic and corrosive debris produced by the articular surface and modular interfaces. These issues are reviewed in detail below.
Loosening and Sepsis
Extrinsic causes of the painful THA are best eliminated by the history and physical examination. After these causes are excluded, loosening and sepsis must be considered as they are the most common cause of intrinsic pain following THA. The diagnosis of loosening is often obvious on radiographs, but in all cases radiographic evaluation is improved if radiographs of the implant before the problem began are available for review. It is important to know the fixation status of both components, as this may dramatically change the preoperative planning and the revision prosthesis requirements. In painful cases where sepsis is not suspected, controversy exists concerning the necessity for preoperative aspiration and the value of laboratory tests to rule out sepsis. Generally a C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are sufficient screening tests, as will be discussed below. If these are elevated, a hip aspiration is warranted (12). Revision total hip replacement in the face of undiagnosed, occult sepsis has a potentially disastrous result.
The diagnostic tools for evaluation of mechanical loosening include plain radiographs, nuclear medicine studies, and more recently, magnetic resonance imaging (MRI). The diagnostic tools available to evaluate the presence or absence of sepsis include laboratory tests, aspiration, and nuclear medicine studies. Newer methods of diagnosis are being studied and hold promise for more accurate and rapid diagnosis.
Loosening
Plain Radiographs—Cemented
In the evaluation of a painful cemented THA, critical examination of serial plain radiographs is the most accurate method of predicting the status of implant fixation. The reliability of plain radiographs and other diagnostic tools is difficult to determine because standard criteria for loosening have not been accepted by all investigators (12,13,14). The most widely accepted criteria have been proposed by O’Neill and Harris (12,15). This classification includes definite, probable, and possible loosening. Definite component loosening is determined by implant subsidence, a new prosthetic–cement radiolucency, cement mantle fracture, or implant fracture.
The two other categories of “probably loose” and “possibly loose” (15) are both based on the presence and extent of bone–cement radiolucencies. Recent studies question the implications of such a radiolucency. Radiolucent lines at the bone–cement interface around cemented total hip replacements may actually represent internal bone remodeling and not necessarily any weakness of the bone–cement interface (Fig. 81.1) (16,17). Therefore, it seems most logical to report a component as either loose or not loose. The diagnosis of loosening on plain radiographs should be based on (a) migration or subsidence and (b) cement or component fracture. Mohler et al. (18) reported that the development of a prosthesis–cement radiolucency may be nonprogressive and not necessarily an indication of impending failure. Unfortunately, these findings may be prosthetic design specific.
Hodgkinson et al. (19) made an important contribution to understanding the plain radiographic evaluation of the cemented acetabular component. In 200 cemented Charnley acetabular components, surgically identifiable loosening was found in 94% of components that had a complete radiolucent line regardless of width. If the radiolucent line involved two-thirds of the interface, 74% were loose. Therefore, the extent of the radiolucency around the acetabular bone–cement interface does in fact have a predictive value for loosening.
Plain Radiographs—Cementless
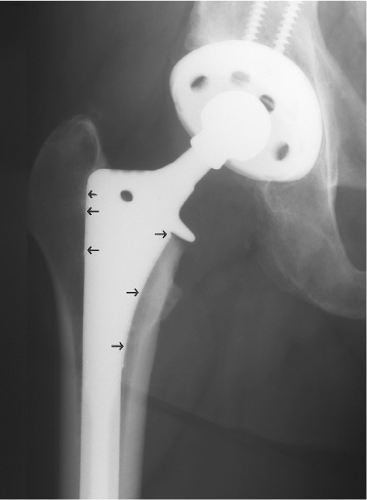
Evaluation of the fixation status of cementless components with plain radiographs involves different criteria. Migration or subsidence is the only reliable criterion for loosening of either component. The classification of Engh et al. (21) for femoral component stability has been widely accepted. Major signs of osseointegration are absence of reactive, radiodense lines around the porous portion of the implant and endosteal spot welds. Minor signs include osseous calcar atrophy, stable distal stem, and the absence of a pedestal (Fig. 81.2). Unfortunately, these signs are prosthesis dependent. Proximally porous-coated stems can have a different picture of osseointegration than extensively coated stems.
Radiodense, reactive lines are common around the smooth distal portion of the stem in proximally porous-coated implants (22). The stem has bone ingrowth stability proximally, but the more flexible femur will flex over the stiffer distal stem. The radiodense, reactive lines are more common the more distant from the point of proximal fixation and a partial pedestal may be present without the component being loose. Extensively coated stems have a more distal point of fixation and, therefore, will have fewer radiodense reactive lines than in a proximally porous-coated implant (21). Radiodense lines around a porous implant and radiolucent lines around a cemented implant have different causes and significances.
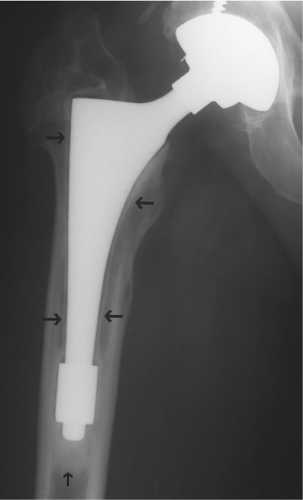
The two reliable criteria for loosening of a cementless femoral component are implant subsidence and/or radiolucency around the entire porous-coated portion of the implant (Figs. 81.3 and 81.4). Less reliable criteria are usually prosthesis dependent. Although complete radiolucencies can be suggestive, migration is the only accurate criterion for loosening of the cementless acetabular component. The determination of migration is critical to make the diagnosis of loosening in both cemented and cementless femoral and acetabular components. This requires meticulous comparison of sequential radiographs.
Standardization of radiographic views makes this determination more accurate. The use of reproducible anatomic or prosthetic landmarks is also helpful. The careful radiographic evaluation can usually determine the fixation status of each component.
Standardization of radiographic views makes this determination more accurate. The use of reproducible anatomic or prosthetic landmarks is also helpful. The careful radiographic evaluation can usually determine the fixation status of each component.
Monoblock acetabular components, as used commonly in MOM arthroplasties, present some unique challenges in determining the status of fixation. Failure of ingrowth has been reported to be more common in these designs likely secondary to the absence of supplemental fixation, the unique ingrowth surfaces, and the rigidity of the device (relative to titanium). These issues seem to be unique to monoblock cobalt-chrome components as tantalum acetabular components with embedded polyethylene have shown promising early to midterm results with minimal loosening since their introduction in the late 1990s (23,24,25,26). Titanium components have similarly excellent results (27,28). MOM articulations with monoblock acetabular components have a higher incidence of ingrowth failure. These components were designed to accommodate larger femoral heads, with the appeal of increased stability. Biomechanical studies have shown increased deformation of thin-walled acetabular components (29). Subhemispheric designs and thin walls have shown high revision rates ranging from 9.3% to 28.6% (30,31,32). One study, however, has demonstrated 98.3% survivorship at 10 years with a different acetabular design for resurfacing (33). The diagnosis of loosening in these components can be difficult as migration or radiolucencies may be absent. Bone scan can also be nondiagnostic. It is therefore important for the physician to be familiar with the symptoms of loosening and the higher-than-usual incidence of loosening in this setting.
Arthrography
Contrast and radionuclide arthrography have some support as an adjunct to the evaluation of loosening in the painful THA. When plain radiographs do not readily demonstrate loosening, arthrography may be helpful to rule out occult loosening. Determination of the accuracy of this diagnostic tool has been clouded by two problems. First, the lack of standardization of diagnostic criteria makes it very difficult to compare studies. Second, arthrography is very technique dependent. Because many techniques have been suggested to improve the accuracy of this test, the variability of the performance of the arthrography questions its accuracy. If contrast arthrography is to be of value, meticulous technique should include high injection pressure, postambulation films, and subtraction techniques (12,34,35).
Although this remains a diagnostic option in the evaluation of the painful THA, we no longer use contrast arthrography in the evaluation of the painful cemented total hip replacement. The unpredictable accuracy cannot justify the additional cost or potential patient discomfort.
Contrast arthrography has not been frequently studied in the evaluation of the painful cementless THA. Data to support the routine use of contrast arthrography in evaluation of the painful cementless THA is insufficient.
Nuclear Medicine Images—Cemented
Technetium-99m methylene diphosphonate (MDP) bone scintigraphy has frequently been used to assess the fixation of cemented components. MDP bone images are very sensitive indicators of bone turnover and activity, but they are not very specific. Increased radionuclide uptake can be caused by infection, loosening, heterotopic ossification, stress fracture, Paget disease, tumor, or reflex sympathetic dystrophy (36).
Our evaluation of loosening in painful cemented THA revealed that MDP bone images have the highest sensitivity, at 97% and 98%, for the femoral and acetabular components, respectively. However, the specificities were low, at 67% and 79%, for the two components. This inaccuracy was manifest by the frequent presence of false-positive bone images.
The MDP bone images are of greatest value in cases where loosening is uncertain from the plain radiographs. A negative or normal MDP bone image essentially excludes the diagnosis loosening. Observation should be recommended in these cases (37). The diagnosis of loosening should not be based solely on the presence of a positive MDP bone image (38). Jensen and Madsen (38) found MDP images less sensitive than plain radiography (0.77 vs. 0.97) and less specific (0.46 vs. 0.7) concluding that these imaging techniques were not complementary to plain radiography in their hands. If the plain radiographs do not reveal loosening, the MDP bone image should be considered a false positive.
Nuclear Medicine Images—Cementless
The interpretation of MDP bone images after cementless THA is very different from that of cemented THA. Bone remodeling occurs after cementless THA, but its characteristics are dependent on bone quality and prosthetic design. The sensitivity of MDP bone images makes this diagnostic tool seem attractive in evaluation of the cementless THA.
We reviewed 40 primary cementless total hip arthroplasties and 16 revision cementless THAs at routine follow-up
examinations through 5 years by MDP bone images. The grading system for the MDP bone images was as follows: 0, less than normal uptake; I, normal uptake; II, slight or moderate increased uptake; and III, intense increased uptake. The natural history of the MDP bone images after cementless THA followed a very consistent chronologic evolution of the radionuclide uptake. Between 2 and 6 weeks postoperatively, there was uniform increased tracer activity of either grade II or intense grade III activity around both components. This increased radionuclide uptake began to decrease toward normal, or to a stable state, between 6 and 12 months after surgery. Further resolution of increased tracer activity continued from 12 to 24 months after surgery. At 2 years, 66% of acetabular components but only 21% of femoral components had returned to a normal bone image. A more recent study cited 38% sensitivity and 73% specificity for detecting acetabular loosening (39).
examinations through 5 years by MDP bone images. The grading system for the MDP bone images was as follows: 0, less than normal uptake; I, normal uptake; II, slight or moderate increased uptake; and III, intense increased uptake. The natural history of the MDP bone images after cementless THA followed a very consistent chronologic evolution of the radionuclide uptake. Between 2 and 6 weeks postoperatively, there was uniform increased tracer activity of either grade II or intense grade III activity around both components. This increased radionuclide uptake began to decrease toward normal, or to a stable state, between 6 and 12 months after surgery. Further resolution of increased tracer activity continued from 12 to 24 months after surgery. At 2 years, 66% of acetabular components but only 21% of femoral components had returned to a normal bone image. A more recent study cited 38% sensitivity and 73% specificity for detecting acetabular loosening (39).
A single MDP bone image may not be helpful in the diagnosis of loosening of cementless THA unless it is negative or normal and associated with normal plain radiographs. This scenario is rare in our experience. An abnormal MDP bone image associated with well-fixed components on plain radiographs should not encourage operative intervention. This initial MDP bone image can be used as a baseline to compare further studies if symptoms persist and the cause is not determined.
Magnetic Resonance Imaging
Another imaging technique that has emerged to evaluate a painful THA is MRI with MARS techniques. MRI has been shown to be superior to CT and plain radiography in quantifying osteolysis around THA, with a sensitivity of 95%, 75%, and 52%, respectively (40,41). Cementless component loosening appears as increased circumferential signal intensity at the implant–bone interface with fat suppression techniques; with cemented components, at the cement–bone interface. Circumferential fibrous membrane formation may also indicate loosening (42,43). With its soft tissue detail and lack of radiation, MRI provides a noninvasive tool to view THAs in multiple orthogonal planes. We cannot encourage MRI to rule out loosening in every THA because of lack of current data; however, we feel that it provides sufficient detail to rule out adjacent soft tissue pathology with minimal drawbacks. MARS MRI also provides a valuable role in the evaluation of the painful or symptomatic MOM hip replacement as discussed below.
Evaluation of Sepsis
The evaluation and determination of periprosthetic infection can be difficult as testing can often be equivocal and the clinical picture unclear. However, every effort should be made to rule out this possibility in the painful THA especially when revision surgery is planned. The recent publication by the Workgroup of the Musculoskeletal Infection Society (MSIS) of the major and minor criteria for periprosthetic joint infection has been helpful to try to establish an agreed upon definition of this condition (44). According to these criteria, a periprosthetic infection is present when:
There is a sinus tract communicating with the prosthesis; or
A pathogen is isolated by culture from at least two separate tissue or fluid samples obtained from the affected prosthetic joint; or
Four of the following six criteria exist:
Elevated serum ESR and serum CRP concentration
Elevated synovial leukocyte count
Elevated synovial neutrophil percentage (PMN%)
Presence of purulence in the affected joint
Isolation of a microorganism in one culture of periprosthetic tissue or fluid, or
Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at x400 magnification
Despite these criteria, establishing the presence of infection can be challenging and infection can still be present even in the case where the above criteria are not fully met. Below we review the workup and testing available to determine the presence or absence of infection.
Plain Radiographs
Plain radiographs often do not reveal signs of sepsis. They may be indistinguishable from those showing a loose THA, because many septic THAs develop loosening. Several radiographic findings are highly suggestive of infection (14,45). Periostitis or periosteal new bone formation, endosteal scalloping, and extensive generalized lysis and osteopenia suggest sepsis. Within the first year, rapid development of a continuous wide radiolucency greater than 2 mm is highly suggestive of sepsis (46).
Laboratory Tests
White blood cell (WBC) count, ESR, and CRP are available to assist in the identification of the septic THA. As an isolated test, the WBC is felt to be of little value (47,48,49). It is frequently normal in septic cases and can be abnormal in aseptic cases, as there are many conditions that affect its value.
The ESR is a valuable tool to assist in identifying sepsis about a THA. It may be beneficial in patients without a known reason for ESR elevation (48). The ESR can be elevated for 6 months after THA. It has been found to have a sensitivity of 60% to 100%, a specificity of 65% to 94%, and an accuracy of 73% to 88% in the identification of infection about THA (50,51,52,53




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree