Evaluation and Management of the Unstable Total Hip Arthroplasty
John J. Callaghan
Craig J. Della Valle
Ong-Art Phruetthiphat
Daniel J. Berry
Case Presentation
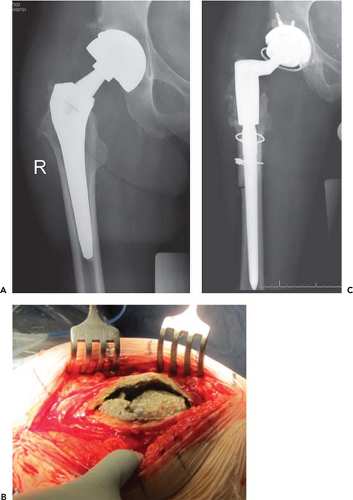
An active, 50-year-old male, gym teacher, who had undergone total hip replacement 4 years previously, presented with a history of increasing limp, one dislocation, and episodes of subluxation in his right hip. Physical examination demonstrated a positive Trendelenburg sign and abductor lurch on walking. ROM was normal compared to the uninvolved left side. Patient had weak to nonexistent abductor strength when testing in the left lateral decubitus position. Preoperative radiograph is demonstrated in Figure 82.1A. Intraoperative findings demonstrated muscle necrosis and avulsion of the gluteus medius from the greater trochanter and the typical appearance of adverse local tissue response (ALTR) (Fig. 82.1B). The hip was reconstructed with a constrained liner and a modular tapered stem to prevent further instability (Fig. 82.1C). Attempt was made at the time of surgery to tenodese the medius muscle into the iliotibial band.
Introduction
Not only is there physical trauma from dislocation following total hip replacement, there is also psychological trauma to both the patient and the surgeon. Historical review of dislocation before the new millennium demonstrated reports of dislocation following primary arthroplasty to range between 0% and 10% depending on the series and depending on the diagnoses at the time of surgery with rates following total hip replacement for fracture of the femoral neck among the highest (1,2,3). In revision surgery, the rates of dislocation following the procedure ranged from 3% to 20% (4). Although there have been many additional options (techniques and devices) for the surgeon to potentially decrease the incidence of the occurrence of dislocation (including larger heads, better head neck ratios with smaller modular tapers, anteverted and modular neck and femoral body designs), the rates of dislocation remain substantial. Evaluation of the 1998 to 2007 Medical National Sample (5%) database demonstrated 3.92% early dislocations and 1.15% late dislocations. Encouraging is the fact that the rate of early dislocation decreased from 4.2% in 1998 to 2.14% in 2007 and dislocation risk was lower by 35% for early dislocation between 2004 to 2007 and 1998 to 2003 as well as by 43% for late dislocations (5). The revision burden for the treatment of dislocation is also substantial. Bozic et al. (6) reported that revision for dislocation and instability was the most common reason for revision at 22.5% versus 19.7% for mechanical loosening, 14.8% for infection, 6.6% for periprosthetic osteolysis, and 6.2% for periprosthetic fracture. Fortunately, two-thirds of the dislocations can be treated closed (3), but the cost for the treatment of dislocation is also substantial. The cost of a closed reduction is 19% of the cost of a primary procedure and the cost of revision for dislocation is 148% of the cost of a primary procedure (7). Finally in this regard, revision for dislocation is not always successful with 39% failure reported by Daly and Morrey (8) and 15% failure in more recent series (9).
There is also a cumulative risk of dislocation with time (10). It is important for both the surgeon and the patient to be aware of this phenomenon. Twenty percent to 30% of dislocations occur late, after 2 to 5 years depending on the study (1,11), with an increased prevalence of 1% every 5 years and 7% after 25 years. It is also related to head size with a cumulative risk of 3.0% and 6.9% for 28-mm heads through the anterolateral and posterior approach, respectively, and 2.4% and 3.6% for 32-mm heads (12).
Prevention of Dislocation
Understanding the epidemiology of the occurrence and treatment of dislocation outlined in the introduction of this chapter allows for those of us performing total hip replacements to recognize that prevention is better than treatment (Fig. 82.2). To prevent the occurrence, the surgeon needs to understand the causes of dislocation. Dorr outlined the reasons for dislocation to include patient compliance issues, soft tissue tensioning issues, component positioning
issues, and impingement issues both of components and bone (13,14,15).
issues, and impingement issues both of components and bone (13,14,15).
Concerning patient-specific issues, the most anecdotal issues are related to alcohol and drug abuse, as well as dementia. Kelley et al. (16,17) have documented the relationship of alcohol abuse and dislocation and the studies of total hip replacement for hip fracture allude to the dementia issue (2). Other diagnoses such as Parkinsonism (18) have been reported to have higher rates of dislocation in some studies but not others. Recognition of patients in these high-risk groups should prompt the surgeon and the hip replacement team to add appropriate counseling, preoperative teaching, and documentation of the increasing risk in these groups. The surgeon may modify the approach and the prostheses in some of these situations.
The issues related to soft tissue tensioning, impingement, and component positioning will be addressed under various aspects of prevention discussed below.
Preoperative Considerations in Prevention
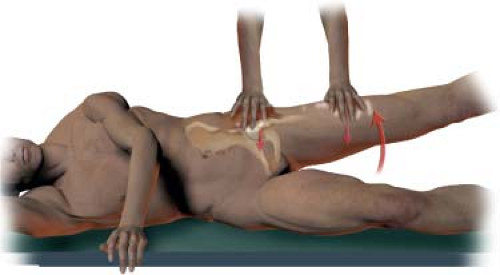
After considering the issues related to patient selection and counseling, thorough physical examination and preoperative planning can require special considerations in regard to preventing dislocation. Important aspects in the physical examination (especially in revision) include evaluation for abductor function of the hip. We do this by testing abduction strength with the patient on their side (Fig. 82.3). As will be discussed later, this may be an overwhelming determinant in regard to successful surgical treatment of recurrent dislocation.
Evaluating spine mobility is also important. There are special considerations for stiff hypolordotic lumbar spines, flexible hyperlordotic spines, as well as pelvic obliquity. These are still being better defined. Finally, preoperative templating and planning can alert the surgeon as to special techniques and devices necessary to provide the most stable construct including stems with increased offset to accommodate femurs with varus neck shaft angles and medially placed center of the femoral head.
Intraoperative Considerations
Patient Positioning
Intraoperative considerations begin with the patient positioning on the operating room table. A definite benefit of the anterior approach is the supine positioning of the patient. The patient is definitely less likely to change positioning of his or her pelvis in this position. If surgery is performed in the lateral decubitus position, which is by far the most common approach in the United States today, the surgeon must use a positioning device that locks the pelvis firmly in the lateral decubitus position. The tendency is for the pelvis to rotate forward as the femoral shaft is retracted forward, leaving the surgeon with the perception that the acetabular component is more anteverted than it is (Fig. 82.4) (3).
Soft Tissue Preservation and Reconstruction
It is now well established that in the surgical soft tissue dissection and reconstruction, the surgeon must preserve the muscles, tendons, and capsule whenever possible. Avulsion or destruction of the gluteus medius is definitely associated with an increased incidence of dislocation (19). Reconstruction of the posterior capsule and tendons has led to a marked decrease in rate of dislocation, to the 0% to 2% range reported with anterior and anterolateral approaches performed by experienced surgeons (20,21,22,23,24,25). The concept is no different than in the era when transtrochanteric approach was commonly utilized and the occurrence of nonunion with escape proximally of the greater trochanter was associated with higher rates of dislocation. Preservation of the posterior capsule and soft tissues has been associated with a decreased dislocation rate in the revision as well as the primary situation (Fig. 82.5) (20). In regard to the greater trochanter, its advancement can aid in stability of the hip construct in the initial construct, primary or revision, as well as in treatment of dislocation (26).
Component Positioning
Today, over half of a century since the inception of the operation, optimal component positioning to avoid dislocation and provide durability of the bearing surface is not completely defined. In fact component positioning to optimize stability may compromise optimization in terms of wear and vice versa (27). Much has been learned from the failures of metal on metal and the development of better mechanical models in this regard (27,28). In addition, optimal component positioning is dependent on the alignment and flexibility of the spine. Understanding these limitations, there are still standards in component positioning,
especially in the acetabular construct that provide stability in most cases. Lewinnek et al. (29) defined the safe zone as 45 degrees ± 10 degrees of abduction and 15 degrees ± 10 degrees of anteversion. Obtaining this position requires identification of bony landmarks including the lateral lip of the acetabulum, the anterior medial aspect of the pubis, and the lateral aspect of the ischium. Osteophytes can make these landmarks difficult to appreciate. Archbold et al. have identified the transverse acetabular ligament as a reproducible soft tissue landmark to position the acetabular component in the safe zone for stability (30). Appropriate anteversion can be obtained by placing the component parallel or collinear to the ligament and the inferior edge in contact with the superior aspect of the ligament (Fig. 82.6). The Beverland group has also identified the need to place the component positioner in 13 degrees less lateral opening than the perpendicular (45 degrees of most positioners) to obtain a position of 40 degrees if operating in the lateral decubitus position (31). It is now recognized that combined anteversion of the acetabular and femoral component is more important than previously understood (27



especially in the acetabular construct that provide stability in most cases. Lewinnek et al. (29) defined the safe zone as 45 degrees ± 10 degrees of abduction and 15 degrees ± 10 degrees of anteversion. Obtaining this position requires identification of bony landmarks including the lateral lip of the acetabulum, the anterior medial aspect of the pubis, and the lateral aspect of the ischium. Osteophytes can make these landmarks difficult to appreciate. Archbold et al. have identified the transverse acetabular ligament as a reproducible soft tissue landmark to position the acetabular component in the safe zone for stability (30). Appropriate anteversion can be obtained by placing the component parallel or collinear to the ligament and the inferior edge in contact with the superior aspect of the ligament (Fig. 82.6). The Beverland group has also identified the need to place the component positioner in 13 degrees less lateral opening than the perpendicular (45 degrees of most positioners) to obtain a position of 40 degrees if operating in the lateral decubitus position (31). It is now recognized that combined anteversion of the acetabular and femoral component is more important than previously understood (27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree