Injuries to the hip and pelvis among runners can be among the most challenging to treat. Advances in the understanding of running biomechanics as it pertains to the lumbopelvic and hip regions have improved the management of these conditions. Conservative management with an emphasis on activity modification and neuromuscular exercises should comprise the initial plan of care, with injection therapies used in a supportive manner.
Key points
- •
Running-related injuries of the hip and pelvis can be particularly challenging to treat, often involving a prolonged period of recovery.
- •
Treatment decision-making is enhanced by corroboration of the history, symptoms, physical examination, and diagnostic imaging (when warranted), and decisions based on isolated tests or imaging are not recommended.
- •
Painful or aggravating activities such as running should be temporarily avoided or modified to reduce the mechanical load to the injured tissues.
- •
Treatment for hip-related tendinopathies should include an initial period to reduce tendon irritability, followed by a progressive loading program.
- •
Symptoms resulting from hip articular injuries, such as femoroacetabular impingement, labral tear, and osteoarthritis, can respond well to conservative management, including modification of running form to minimized loading to the hip joint.
Introduction
Injuries to the hip or pelvis comprise approximately 11% of running-related injuries and can be among the most challenging to successfully treat, often involving a prolonged period of recovery. Unique risk factors that may predispose an individual to hip or pelvis injury during running have not been clearly identified, although some evidence suggests women are at a greater risk. The biomechanics of the hip and pelvis during running, including the muscular demands, have been characterized and provide useful insights into appropriate rehabilitation strategies to maximize recovery and return to full running. The purpose of this article is to review the more common running-related injuries to the hip and pelvis, with consideration of the cause, clinical presentation, and management.
Introduction
Injuries to the hip or pelvis comprise approximately 11% of running-related injuries and can be among the most challenging to successfully treat, often involving a prolonged period of recovery. Unique risk factors that may predispose an individual to hip or pelvis injury during running have not been clearly identified, although some evidence suggests women are at a greater risk. The biomechanics of the hip and pelvis during running, including the muscular demands, have been characterized and provide useful insights into appropriate rehabilitation strategies to maximize recovery and return to full running. The purpose of this article is to review the more common running-related injuries to the hip and pelvis, with consideration of the cause, clinical presentation, and management.
Injuries
Despite each injury having unique presentation and examination characteristics, certain aspects of the management strategy are common to all. For example, it is imperative that the irritability of the condition be controlled during the initial treatment stages using a variety of options including ice, non-steroidal anti-inflammatory drugs (NSAIDs), and activity modification. Running may need to be stopped temporarily or modified to reduce mechanical load to the injured area, such as decreased volume or intensity, avoiding hills, or using a higher step rate. Body weight–supported running or deep water running may also be substituted. Once symptoms are controlled and injured tissues are able to tolerate the demands of running, a progressive return is required to reacclimate to the mechanical loads of running. Retraining of running gait may be warranted to correct any pathomechanics in addition to a progressive return-to-running program to reduce the risk of reinjury. Also common to the management of all running-related hip and pelvis injuries is consideration of lumbopelvic dysfunction that can refer symptoms to, and affect function of, the primary area of injury. Lumbopelvic dysfunction, including myofascial trigger points ( Fig. 1 ), joint and neurodynamic dysfunction, often occurs concurrently with hip and pelvis conditions and can affect the patient’s presentation and rehabilitation. Hip mobility deficits are commonly observed in running-related hip and pelvis injuries and are amenable to mobilization procedures ( Fig. 2 ).


Proximal Hamstring Tendinopathy
Proximal hamstring tendinopathy is a challenging injury owing to the prolonged course of treatment typically required to successfully return to full level of performance. Distinct from a hamstring strain injury, this condition often involves a progressive onset of symptoms localized near the ischial tuberosity, possibly involving the ischial bursa. Histologic evaluation frequently indicates a chronic tendinopathy with fibrosis, and occasional hyaline degeneration at the insertion site. In severe cases, MRI examination will reveal an associated stress reaction with marrow edema in the ischial tuberosity.
Presentation
- •
Deep buttock pain is present near the ischial tuberosity and is aggravated when accelerating or running uphill, or with direct pressure on the injured area, including prolonged sitting. Pain is provoked near end-range hip flexion and with resisted hip extension in a hip flexed position.
- •
Pain provocation tests include the bent-knee stretch test, modified bent-knee stretch test, and Puranen-Orava test ( Table 1 ). All have been found to be reliable and valid, with the modified bent-knee stretch test having the highest values.
Table 1
Clinical examination tests for hip and pelvis conditions
Test
Description of Positive Test
Reference Standard
Sensitivity (95% CI)
Specificity (95% CI)
+ Likelihood Ratio (95% CI)
− Likelihood Ratio (95% CI)
Proximal hamstring tendinopathy
Bent-knee stretch test
Pain with slow extension of the knee from a position of maximum hip flexion in supine
Pain in lower gluteal region, ischial tuberosity tenderness, and increased MRI signal intensity of proximal hamstring tendons
0.84 (0.71, 0.93)
0.87 (0.73, 0.95)
6.5 (3.1, 13.8) a
0.18 (0.09, 0.35) a
Modified bent-knee stretch test
Pain with rapid extension of the knee from a position of maximum hip flexion in supine
0.89 (0.76, 0.96)
0.91 (0.79, 0.97)
10.3 (4, 26.3) a
0.12 (0.05, 0.27) a
Puranen-Orava test
Pain with hamstring stretch in standing with foot supported so that hip is flexed 90° and knee is fully extended
0.76 (0.61, 0.87)
0.82 (0.68, 0.92)
4.4 (2.3, 8.4) a
0.29 (0.17, 0.49) a
GTPS
Resisted external derotation test
Pain when the patient internally rotates and extends the hip against examiner resistance from 90° hip flexion and full external rotation
MRI evidence of gluteus minimus or medius tendonitis, tendinosis, tear, or bursitis
0.88 b (0.66, 0.97) a
0.97 b (0.87, 1) a
33.5 a , b (4.8, 233.7)
0.12 a , b (0.03, 0.45)
Trendelenburg sign
When standing unilaterally on the involved leg, patient unable to elevate and hold contralateral pelvis for 30 s
0.23 (0.05, 0.57)
0.94 (0.53, 1)
3.64 (0.2, 65.9)
0.82 (0.59, 1.15)
Resisted hip abduction
1. Pain with resisted side-lying hip abduction up to 25° with the hip flexed 0°, 45°, and 90°
0.71 b (0.47, 0.87) a
0.95 b (0.83, 0.99) a
13.4 a , b (3.4, 53.5)
0.31 a , b (0.15, 0.65)
2. Pain with resisted side-lying hip abduction with the hip 0° flexed and neutral rotation
0.47 (0.22, 0.73)
0.86 (0.42, 0.99)
3.27 (0.5, 21.7)
0.62 (0.4, 1)
FABER
Lateral hip pain with the involved leg crossed (lateral malleolus just superior to the opposite patella) in supine and downward pressure applied to the medial knee and contralateral anterior superior iliac spine to externally rotate and abduct the leg toward the table.
Differentiation between GTPS and OA
0.83 (0.68, 0.93)
0.9 (0.68, 0.99)
8.3 a (2.2, 31.1)
0.19 a (0.1, 0.38)
Piriformis syndrome
Test item cluster
Two of the following 3: (1) pain at the intersection of the sciatic nerve and piriformis in side-lying FAIR position, (2) tenderness with palpation of the sciatic nerve and piriformis intersection, or (3) straight-leg raise <65° or 15° less than unaffected side
Delayed H-reflex between anatomic supine and side-lying FAIR position
0.92 (0.90, 0.94) a
0.85 (0.78, 0.90) a
6.1 a (4.0, 9.3)
0.01 a (0.07, 0.12)
Chronic groin pain
Bilateral adductor test
Groin pain with bilateral resisted hip adduction with both hips flexed 30°, slight hip internal rotation, and knees extended
MRI evidence of pubic bone marrow edema
0.54 (0.4, 0.68)
0.93 (0.81, 0.98)
7.8 (2.5, 23.9)
0.49 (0.35, 0.68)
Single adductor test
Ipsilateral or contralateral groin pain with unilateral resisted hip adduction in supine with tested hip flexed 30° and knee extended; opposite hip is flat on the table in 0° hip flexion
0.30 (0.19, 0.45)
0.91 (0.78, 0.96)
3.3 (1.2, 9.2)
0.77 (0.62, 0.95)
Squeeze test
Groin pain when patient maximally contracts adductors in supine with 45° hip flexion and 90° knee flexion and examiners fist between knees
0.43 (0.30, 0.58)
0.91 (0.78, 0.96)
4.7 (1.7, 12.6)
0.62 (0.48, 0.82)
FAI/labral tear
FADIR
Pain when hip is flexed 90° and then adducted and internally rotated with patient supine
Evidence of FAI or labral tear during surgery
0.99 c (0.98, 1)
0.05 c (0.01, 0.18)
1.04 c (0.97, 1.12)
0.14 c (0.02, 0.93)
FlexIR
Pain when hip is flexed 90° and then internally rotated with patient supine
0.96 c (0.81, 0.99)
0.25 c (0.01, 0.81)
1.28 c (0.72, 2.27)
0.15 c (0.01, 1.99)
Squat test
Pain when performing a maximum squat with feet shoulder width apart and arms held parallel to the floor
MRI evidence of cam-type FAI
0.75 (0.57, 0.89)
0.41 (0.27, 0.57)
1.3 (0.9, 1.7)
0.6 (0.3, 1.2)
Labral tear
THIRD test
Pain during hip compression and internal rotation that is absent or reduced with hip distraction and internal rotation with patient supine and hip flexed 90° and adducted 10°
Operative reports indicating labral tear
0.98 (0.93, 0.99)
0.75 (0.3, 0.95)
3.9 (0.7, 21.4)
0.03 (0, 0.12)
OA
Sutlive et al, test item cluster
- 1.
Patient reports squatting aggravates symptoms
- 2.
Pain in the groin or lateral hip during adduction of the scour test
- 3.
Lateral hip pain with active hip flexion
- 4.
Hip pain during active hip extension
- 5.
Passive prone hip internal rotation ≤25°
Kellgren and Lawrence score of 2 or higher via radiographs
4/5 tests positive
0.48 (0.26, 0.70)
0.98 (0.88, 1)
24.3 (4.4, 142.1)
0.53 (0.35, 0.8)
3/5 tests positive
0.71 (0.48, 0.88)
0.86 (0.73, 0.94)
5.2 (2.6, 10.9)
0.33 (0.17, 0.66)
American College of Rheumatology test item cluster
Positive in presence of either of the following test clusters:
Evidence of at least mild arthritis via radiographs
0.86 (0.78, 0.91) a
0.75 (0.65, 0.83) a
3.4 a (2.4, 4.9)
0.19 a (0.12, 0.3)
- 1.
Hip pain
- 2.
Hip internal rotation ≤15°
- 3.
Hip flexion ≤115°
- 1.
Hip internal rotation ≤25° with pain
- 2.
Morning hip stiffness lasting ≤60 min
- 3.
Age >50 y
a Calculated by the authors of this article.
b Calculated from case control design. Sensitivity calculated from cases and MRI; Specificity calculated from control participants without use of MRI as the reference standard.
- 1.
- •
For cases that fail conservative management or are slow to progress, MRI may reveal a partial tendon tear.
- •
If symptoms extend into the posterior thigh, contribution from the lumbar spine should also be ruled out and irritation of the sciatic or posterior femoral cutaneous nerves should be considered (slump test).
- •
Differential diagnosis includes sacroiliac dysfunction, ischiogluteal bursitis, obturator internus bursitis, ischifemoral impingement, piriformis syndrome, lumbopelvic dysfunction, acetabular labral tear, and stress fracture of the pelvis and femoral head.
Management
- •
Early treatment should include correction of lumbopelvic joint dysfunction and soft tissue mobilization to the involved tendon and adjacent muscles, avoiding direct pressure over the ischial tuberosity.
- •
Progressive loading guidelines ( Table 2 ) should be followed with care to minimize tendon compression against the ischial tuberosity during the early stages of recovery.
Table 2
Tendinopathy management recommendations based on Kountouris and Cook
Purpose
Treatment
Pain management and tendon load reduction
- •
Pain management
- ○
Ice and NSAIDs
- ○
Isometric exercises of the involved tendon: 30–60-s holds, 3–5 repetitions, 1–3 times; start with a lower frequency, repetition, and duration if tendon is highly reactive/irritable
- ○
Corticosteroid injections may be considered for reactive tendons in early disrepair
- ○
- •
Reduce tendon load
- ○
Reduce running volume and load (increase step rate, avoid hills) to avoid exacerbation of symptoms
- ○
May need to temporarily avoid over-ground running and substitute other exercise options (cycling, deep water running, or body-weight–assisted treadmill)
- ○
Address local and adjacent impairments including trigger points, joint mobility, and posture
- ○
Tendon load adaptation
- •
Step 1: Improve muscle strength (higher load, 3 sets of 8–15 repetitions, 3–4 d/wk) and endurance (lower load, 3 sets of 20–30 repetitions, 5–7 d/wk) based on individual impairments and needs
- ○
Continue isometric exercises and ice for pain management
- ○
Consider non-weight-bearing exercise for lower load training and progress to weight-bearing exercises for higher load training that more closely reflect the demands of running
- ○
Emphasis on the eccentric phase initially but not exclusively
- ○
Consider neuromuscular control training of lumbopelvic region
- ○
- •
Step 2: Improve muscle power
- ○
Increase speed of weight-bearing exercises
- ○
Progress to plyometric training, such as jump squats, skipping, jumping rope, double-leg progressing to single-leg hopping
- ○
30–60-s repetitions, 4–6 sets with 60 s rest between sets, 2–3 d/wk
- ○
Progression should consider (1) pain behavior for 24 hours following the exercise to assess tendon irritability, and (2) similar performance between involved and uninvolved limbs with exercises and pain provocation tests.
Data from Kountouris A, Cook J. Rehabilitation of Achilles and patellar tendinopathies. Best Pract Res Clin Rheumatol 2007;21:295–316.
- •
- •
Neuromuscular control exercises for the lumbopelvic region are recommended, with a particular focus on gluteal muscle activation. Additional strengthening of the hamstrings with eccentric exercises may be considered once the tendon is less reactive; however, hip flexion angle may need to be initially constrained to prevent aggravation of the condition due to tendon wrapping around the ischial tuberosity.
- •
Corticosteroid injection under ultrasound guidance into the peritendinous soft tissues may be necessary in some more acute cases to enable performance of progressive loading program.
- •
Platelet-rich plasma injections may be useful in promoting symptom reduction and tissue recovery, although research is limited. Limited evidence on shockwave therapy has shown promising benefits.
- •
When pain persists despite multiple attempts of conservative management, surgery may be considered to relieve adhesions and facilitate normal sliding mechanics of the involved tissues. The proximal tendinous structures of the hamstrings are typically divided without releasing the muscle from the ischial tuberosity. Neurolysis may be performed if sciatic nerve compression is observed.
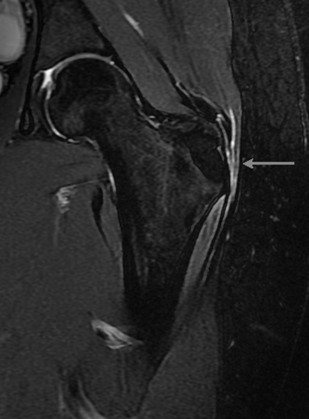
Greater Trochanteric Pain Syndrome
Greater trochanteric pain syndrome (GTPS) is lateral hip pain that may occur due to a variety of disorders, including trochanteric and gluteus medius bursa irritation, external snapping hip (coxa sultans), and gluteus medius and minimus tendon tears and tendinopathy ( Fig. 3 ). GTPS accounts for 5% of all running injuries, affecting women up to 5 times more than men. Consideration of peak muscle forces primarily of the gluteus medius and minimus during the loading response of running is important in the cause and rehabilitation of the runner with GTPS.
Presentation
- •
Onset is often insidious but may be related to a change in running volume or intensity, running on a cambered surface, and excessive peak hip adduction during stance phase.
- •
Pain is localized near the greater trochanter and may extend down the thigh in a nondermatomal pattern. Pain is exacerbated when lying on the affected side, sitting with legs crossed, unilateral standing, stair climbing, walking, or running, and can be reproduced with resisted hip abduction.
- •
Pain with resisted internal rotation from 90° of flexion and maximal hip external rotation implicates gluteal tendinopathy, whereas a positive Trendelenburg test suggests a gluteal tear (see Table 1 ).
- •
Hip internal or external rotation may be limited or painful; however, restricted motion in multiple directions is suggestive of an intra-articular disorder. In contrast to patients with hip osteoarthritis (OA), those with GTPS are able to localize lateral hip pain, have a FABER (flexion, abduction, external rotation) test provoking lateral hip pain (see Table 1 ), and do not have difficulty manipulating shoes and socks.
- •
Prior or concurrent lumbar symptoms are common and warrant evaluation. Trigger points of the spinal muscles, quadratus lumborum, gluteal muscles, piriformis, and tensor fascia latae may refer to the lateral hip (see Fig. 1 ).
- •
With external snapping hip, the anterior gluteus maximus and iliotibial band snaps audibly when moved posterior to anterior over the greater trochanter during hip flexion from an extended position. Manual compression just proximal to the trochanter may alleviate the snapping.
- •
MRI is typically reserved for recalcitrant cases to assess integrity of the gluteal tendons, bursa, and intra-articular structures.
Management
- •
Early treatment includes mobilization of adjacent soft tissues, hip (see Fig. 2 ), and lumbopelvic mobilization to include sacroiliac manipulation, and the use of pillows to offload the hip when sleeping in side-lying.
- •
Progressive resistance training of the hip abductors and external rotators should be emphasized, starting with isometric activities and progressing to movements that maximize gluteus medius activity ( Figs. 4 , 5 B, 6 , and 7 , Table 3 ).
Fig. 4
Hip abduction exercise: In side-lying with the target hip on top and lower leg flexed at the hip and knee, the top hip is abducted with slight external rotation while the pelvis is stabilized perpendicular to the table. Additional internal or external rotation of the hip does not significantly change gluteus medius to tensor fascia latae ratio, but stabilization of the pelvis perpendicular to the table is important to improve gluteus medius activation. The back and heel can be placed at a wall to assure the pelvis remains perpendicular and to avoid compensatory hip flexion during abduction. An ankle weight can be used for additional resistance or a belt to achieve an isometric contraction. This can be progressed to a weight-bearing exercise by performing a side plank.
Fig. 5
Stabilization of lumbopelvic and hip regions through muscle performance training: ( A ) supine bridge to target gluteal muscles starting with bilateral bridge (not pictured) that can be progressed by adding a resistance band to emphasize hip abduction/external rotation and then a unilateral bridge; rotation of the pelvis is avoided via feedback from a dowel held on the front of the pelvis; ( B ) lateral side plank to target hip abductors that can be initiated from the knees (not pictured) and progressed to the feet, and then, by lifting the top leg, emphasis is placed on adequate abduction without rotation of the pelvis; ( C ) medial side plank to target hip adductors, emphasis is placed on adequate hip adduction without rotation of the pelvis; ( D ) prone plank that can be initiated with feet on the floor (not pictured) and progressed to both legs on a stability ball (placing ball closer to knees for less difficulty or closer to toes for greater difficulty), and by lifting one leg, emphasis is placed on a neutral spine (using a board or half foam roll for feedback) and avoidance of pelvic rotation.
Fig. 6
Clam exercise: In side-lying position with the target hip on top in 30° of flexion, the hip is externally rotated and abducted. A resistance band can be added for greater difficulty or a belt used to perform an isometric contraction. This exercise targets the posterior fibers of the gluteus medius and minimus in addition to the piriformis, which are most active between 30° of hip flexion and 15° of hip extension during running.
Fig. 7
Squat training: ( A ) bilateral squat or position to perform side-stepping and ( B ) unilateral squat. Emphasis is placed on avoidance of dynamic knee valgus (via hip internal rotation and adduction, and foot pronation). A band can be placed around the distal thigh to encourage the patient to react against the band using hip abductors and external rotators. A mirror is also encouraged initially for visual feedback of form.
- •
Corticosteroid injection or extracorporeal shock-wave therapy may provide moderate improvement in symptoms and function in the short term that equals the response to exercise in the long term.
- •
Surgical treatment may be considered if symptoms persist after 6 months of conservative management. Procedures include open or arthroscopic gluteal tendon repair or reconstruction, bursectomy, or iliotibial band release or lengthening.
Piriformis Syndrome
Piriformis syndrome is a neuromuscular disorder involving the sciatic nerve and piriformis muscle. Lack of consensus on the definition of piriformis syndrome and valid diagnostic criteria make it difficult to determine the true incidence. Piriformis syndrome is estimated to be the source of symptoms in 6% to 8% of individuals presenting with low back pain and sciatica. During running, the piriformis has a similar activation pattern as the gluteal muscles, being most active during the loading response of stance, initially working eccentrically and then concentrically.
Presentation
- •
Pain in the buttock is presented that may refer down the back of the leg in a sciatic distribution and is aggravated with sitting. Onset is typically insidious but may involve a traumatic impact, such as a fall. Tenderness is localized to the intersection of the sciatic nerve and piriformis in side-lying with hip flexed 60°, adducted, and internally rotated (FAIR), and supine straight leg raise is often limited (see Table 1 ).
- •
External rotation of the hip may be observed in standing or sitting. In supine with legs extended, increased external rotation of the involved leg may be present (Piriformis sign) and painful with forced internal rotation (Freiberg test).
- •
During the loading response of walking or running, or during a single-leg step down test, excessive hip adduction and internal rotation may be observed, suggesting impaired eccentric piriformis function.
- •
In side-lying FAIR position, pain may be provoked with resisted abduction/external rotation (Pace test), or simply abducting the hip with neutral rotation (Beatty test). Diagnostic accuracy of these tests is unknown, and false positives are likely if symptom centralization occurs with lumbar movement testing.
- •
Differential diagnosis includes lumbar radiculopathy, sacoiliac joint dysfunction, intra-articular hip pathologic abnormality, proximal hamstring tendinopathy, greater trochanter pain syndrome, and referral from the gluteus medius or quadratus lumborum.
Management
- •
Mobilization of soft tissue restrictions and trigger points is useful for the piriformis, gluteals, and lumbosacral region. Aggressive piriformis stretching should be avoided when symptoms are irritable.
- •
Hip and lumbosacral mobilizations may also useful if restricted motion is observed (see Fig. 2 ).
- •
Neuromuscular training using rotational exercises may start with isometrics if symptom irritability is observed and progress to isotonics, with eventual progression into weight-bearing movements.
- •
Image-guided injections (corticosteroid, anesthetic, or botulinum toxin A) may be used in combination with the above for refractory cases to obtain short-term relief and determine potential surgical benefit.
- •
A pelvic neurogram is recommended in refractory cases to better assess for anomalous sciatic nerve anatomy causing piriformis syndrome. There are 6 commonly described anatomic relationships, the most common being the sciatic nerve passing below the piriformis muscle.
Iliopsoas Syndrome
The iliopsoas muscle functions eccentrically during the terminal stance phase of running to control hip extension and then acts concentrically during the initial swing to advance the thigh forward. The iliopsoas tendon may be irritated by snapping over the anterior inferior iliac spine, the iliopectineal eminence, or the lesser trochanter (internal coxa saltans). Iliopsoas impingement has also been described due to pressure, friction, or adhesions between the iliopsoas and the femoral head and anterior labrum. Because iliopsoas tendinopathy, iliopsoas bursitis, and iliopsoas impingement may be hard to discriminate and can occur together, collectively, these conditions are called iliopsoas syndrome.
Presentation
- •
Onset is usually insidious but may involve increased uphill running. Pain is typically present in the anterior hip, and possibly the ipsilateral lower back ( Fig. 1 C). Tenderness may be present over the anterior hip joint; however, this may also indicate femoroacetabular impingement (FAI) or labral pathologic abnormality.
- •
Pain is elicited with resistance of hip flexion, slight abduction, and external rotation in the supine position or when stabilizing with the involved leg in the prone plank position ( Fig. 5 D).
- •
Internal snapping can be reproduced with motion of the hip from flexion/abduction/external rotation to extension/adduction/internal rotation.
- •
Iliopsoas tightness may be present, contributing to impingement. Iliopsoas impingement may be reproduced with supine hip flexion, adduction, and internal rotation (FADIR test) (see Table 1 ).
- •
Imaging is typically reserved for cases that are unresponsive to conservative management. Radiographs may identify calcifications or femoroacetabular abnormalities associated with tendon or bursa irritation. MRI can provide further evidence of labral, tendon, and bursa pathologic abnormality.
Management
- •
General guidelines for tendon rehabilitation apply, including specific considerations for the iliopsoas muscle function and activities that load the tendon.
- •
Soft tissue mobilization, treatment of trigger points, and stretching of impairments identified in the iliopsoas should be emphasized with consideration of adjacent regions. Joint mobilization of the hip (see Fig. 2 ) and lumbosacral region may be considered.
- •
Once initial symptom irritability is managed, the tendon can be progressively loaded (see Table 2 ) complemented by hip strengthening (side-lying clam [see Fig. 6 ], seated hip internal and external rotation, and single-leg mini–wall squats [see Fig. 7 B]) and lumbopelvic stabilization exercises (see Fig. 5 ).
- •
Ultrasound-guided injections may be used in refractory cases to obtain short-term relief and coupled with conservative treatments indicated above. Endoscopic release or lengthening of iliopsoas may be considered if the patient continues to be unresponsive to conservative care.
Chronic Groin Pain
Chronic groin pain has been attributed to a variety of sources, such as intra-abdominal, genitourinary, and musculoskeletal, with no clear consensus on definition or diagnostic criteria. Involvement of the proximal adductor tendons is commonly recognized and often the focus of treatment programs. Rectus femoris and rectus abdominus have also been implicated, and the presence of athletic pubalgia (sports hernia) should be considered. Common in sports requiring high-speed cutting (ie, soccer, hockey, and American football), chronic groin pain is less frequent among distance runners, although female runners during and after pregnancy may be at particular risk considering the structural and neuromuscular changes to the lumbopelvic region. For the runner, intra-articular hip pathologic abnormality and femoral neck or lesser trochanteric bone stress injury needs to be ruled out.
Presentation
- •
Physical examination findings are often not specific enough to clearly differentiate between adductor tendinopathy, osteitis pubis ( Fig. 8 ), and athletic pubalgia. Imaging techniques such as ultrasonography or MRI may prove useful during the diagnostic process.









