CHAPTER 18 Evaluation and Management of Failed Rotator Cuff Surgery
Rotator cuff tears are a common cause of shoulder pain and disability. Surgical repair can provide successful clinical results.1,2 However, complications leading to poor outcomes do occur. Mansat and colleagues published a review of 40 articles evaluating outcomes of open rotator cuff repairs and found a complication rate of 10.5%.3
Both intrinsic and extrinsic pathologic processes were implicated as causes, including failed tendon repair, infection, deltoid avulsion, postoperative stiffness, and reflex sympathetic dystrophy. A study by Brislin and coworkers showed that the complication rate after arthroscopic rotator cuff repair (10.6%) is similar to the rate associated with open repairs; however, the types of complications typically encountered are different.4 Arthroscopic rotator cuff repair allows improved glenohumeral joint assessment and avoidance of deltoid attachment, which makes missed intra-articular pathology (e.g., labral tears, biceps tendinitis) or deltoid avulsions much less likely as causes of pain after surgery. Despite the advancement to all-arthroscopic rotator cuff surgery, open or mini-open surgeries can still be useful if one is contemplating concomitant removal of hardware or internal fixation of a fracture.
We define failure after rotator cuff surgery as a lack of improvement relative to the preoperative condition secondary to decreased function, persistent pain, or both. As both of the above-mentioned studies imply, retear of the rotator cuff is only one of the many factors that can lead to failed rotator cuff surgery. Intrinsic and extrinsic pathologic processes have both been implicated as causes of failure (Box 18-1).5 A detailed knowledge of the possible complications is necessary to thoroughly evaluate patients with persistent pain or dysfunction after rotator cuff surgery. Treatment options are then individualized based on patient characteristics and the type of complication suffered. Typically, the results of revision surgery are inferior to the expected outcomes of primary rotator cuff surgeries.1,6–9 However, when the source of failure is correctly identified and treated appropriately, functional and symptomatic improvement can be expected. This chapter details the more common causes of failed rotator cuff surgery, with particular attention given to revision repairs. Chapter 23 focuses on anterosuperior escape and the use of the reverse shoulder prosthesis.
BOX 18-1 Common Causes of Persistent Pain After Rotator Cuff Surgery
Adapted from Williams GR: Painful shoulder after rotator cuff surgery. J Am Acad Orthop Surg 5:97-108, 1997.
DIAGNOSIS
In many cases, a detailed history, physical examination, and standard shoulder radiographs enable the physician to narrow the extensive differential diagnosis associated with pain after rotator cuff repair. In general, failed surgery can be classified as weakness, stiffness, instability, arthritis, surgical complication, or pain without apparent cause. In terms of establishing a diagnosis, we find it useful to group pathologies into one of two etiologies: intrinsic causes and extrinsic causes (see Box 18-1).5 In certain cases, extrinsic and intrinsic factors both contribute to persistent disability. Successful treatment of patients requires identifying all contributing pathologic entities.
The patient history should document preoperative symptoms, previous steroid injections, details of the initial surgery (when, where, technique used, associated procedures), medical comorbidities, and nicotine use. A copy of the initial operative report should be obtained, as should postoperative physical therapy notes. It is important to distinguish between patients who did well until a specific acute event and those who never did well after surgery. Documenting the amount of force and mechanism of an acute event, when possible, can be helpful. New symptoms, including pain, weakness, night pain, stiffness, fevers, chills, and wound problems, must be documented.
Physical examination includes strength and range-of-motion testing of both upper extremities. Tests for stability and impingement should be performed. Atrophy of the infraspinatus and supraspinatus or of the infraspinatus alone can indicate suprascapular neuropathy. Though scapular winging is a rare cause of persistent pain after rotator cuff surgery, scapulothoracic and scapulohumeral motion should be observed in all patients.5 In patients with severe dysfunction and winging, electromyography (EMG) can confirm long thoracic or spinal accessory nerve lesions. Examination of the cervical spine and a detailed neurovascular examination of the entire extremity are essential components of the work-up. Cervical radiculopathy involving the fifth or sixth cervical root is one of the most common extrinsic causes of persistent shoulder pain.5 When indicated, magnetic resonance imaging (MRI) and EMG can confirm the diagnosis.
Adjunctive studies can help make or confirm diagnoses. Standard radiographs should be used in all cases, because they can reveal entities such as glenohumeral arthritis, acromial stress fractures, heterotopic ossification, and supraspinatus outlet narrowing. Previous studies have confirmed the utility of MRI for evaluation of patients who have pain and loss of function after surgery for rotator cuff disease.10,11 Gaenslen and colleagues found MRI to be 84% sensitive and 91% specific for diagnosing full-thickness rotator cuff tears in this patient population and 83% sensitive and specific for diagnosing partial-thickness rotator cuff tears.11 Diagnostic arthroscopy can also be a useful tool for evaluating intrinsic causes of persistent pain after rotator cuff repair.
FAILED REPAIRS
Etiology
Recurrent or persistent rotator cuff tears have been reported to occur in 12% to 90% of cases.12–19 Advances in surgical instrumentation and repair biomechanics have improved healing rates, but the most significant factor determining the success of healing continues to be the size of the tear.14,16,17,20 Massive tears have a much higher retear rate than single tendon tears, and posterosuperior massive tears have the worst prognosis.14,21,22 Other associated risk factors include advanced age, chronic tears with poor tendon quality and muscle atrophy, diabetes, smoking, steroid injections, inappropriate rehabilitation, increased tension on the repair, and insufficient subacromial decompression.6,15,23–25
In general, rotator cuff repair is associated with satisfactory pain relief; however, the success rates do not correlate well with tendon healing.12,14,16,24 Harryman and coauthors used ultrasound to document the integrity of rotator cuff repairs in 105 shoulders.16 The tendon was intact in 80% of isolated supraspinatus tears. If more than one tendon was involved, healing rates went down to less than 50%. Patients who had an intact repair had better function, motion, and pain relief than those with recurrent tears. Despite this, overall, more than 90% of the patients were satisfied with the surgery, and this result did not correlate with repair integrity. Other studies have corroborated these findings.
Galatz and colleagues studied large and massive rotator cuff tears treated with arthroscopic repair.14 Seventeen of 18 patients showed evidence of a recurrent tear via ultrasound. Patient satisfaction, however, remained high: 16 of 18 reported decreased pain and increased function at 1 year after surgery. By 2 years after surgery, there was a decrease in functional outcomes, but all patients were satisfied with the result.
Jost and colleagues found a similar lack of correlation between rotator cuff integrity and patient satisfaction.26,27 They assessed 20 patients with documented reruptures of the rotator cuff after surgical repair at an average of 3.2 years and again at 7.6 years. In the short-term study, they found that despite progression of atrophy, fatty degeneration, and glenohumeral arthritis in all patients, 17 of the 20 were satisfied with the procedure. At longer term follow-up, satisfaction increased, and 19 of 20 patients were satisfied or very satisfied with the outcome.27 They found that reruptures present at 3.2 years did not increase in size, and supraspinatus reruptures smaller than 400 mm2 had the potential to heal.
In Bigliani’s large series of failed rotator cuff repairs, persistent impingement, based on radiographs and operative visualization, was the most common identifiable factor.1 Inadequate decompression was associated with a retear of the tendon in 90% of the cases. Additionally, they found that 15 of 31 patients had inadequate tissue mobilization at the time of initial repair. In addition to eliminating a source of external impingement, acromioplasty and subacromial decompression can improve visualization in the subacromial space, making the technical aspects of the repair easier.
Rotator cuff tendon repair technique is an important factor in tendon healing. The most common mode of failure involves suture pulling through the tendon.28 Gerber and coworkers showed that a modified Mason–Allen stitch provides superior pullout strength, and possibly a more secure repair, than simple or mattress sutures.29 Arthroscopically, the massive cuff stitch acts in a similar fashion.30,31 Strength of fixation is also related to the pullout strength of anchoring devices, number of anchors, and quality of both the bone and tendon tissue. Many studies have elucidated the biomechanical benefits of double-row suture anchor repairs.32–37 Theoretically, these repairs better re-create the three-dimensional anatomic footprint of the rotator cuff insertion over the tuberosity while providing increased pullout strength and ultimate load to failure.37–39 Clinically, the results are promising as well.20 If repair site biomechanics, knot stability, quality of repair tissue, and repair tension were not optimized at the time of initial surgery, then revision surgery, in which these issues are addressed, can provide patients with improved outcomes. Despite meticulous surgical technique, healing can be compromised by poor patient compliance with postoperative activity restrictions and physical therapy.
Evaluation
Physical findings vary based upon size and location of the tear. Concomitant soft tissue contracture makes the findings on rotator cuff examination less reliable. The physical examination of the rotator cuff complex is discussed in detail in Chapter 17. Briefly, weakness with the arm abducted in the scapular plane with the elbow extended and the humerus internally rotated can indicate a recurrent tear in the supraspinatus. Recurrent defects in the supraspinatus and upper infraspinatus tendons may manifest by weakness of arm abduction and weakness of external rotation with the arm at the side.40 In these tears, the weakness resolves as the arm is elevated to 90 degrees in the scapular plane. This is in contradistinction to tears that involve the inferior infraspinatus and teres minor tendons, which demonstrate weakness in external rotation with the arm at the side as well as in 90 degrees of elevation. A positive external rotation lag sign is present when the arm cannot be actively held after maximum passive external rotation. This indicates a substantial tear involving the infraspinatus tendon.41 Weakness of terminal internal rotation and increased passive external rotation indicate subscapularis insufficiency. The lift-off test is sensitive for detecting subscapularis dysfunction, as well.42 Suspected recurrent rotator cuff tears are confirmed by imaging studies.
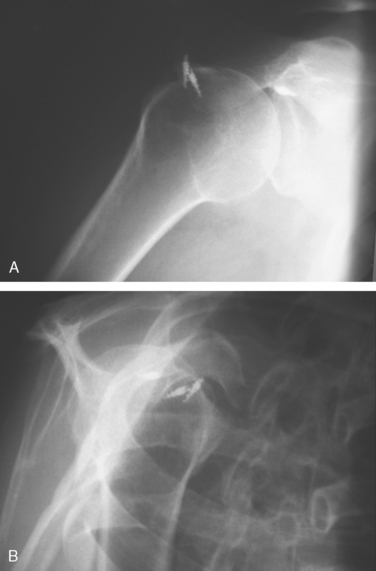
Standard radiographs, including an anteroposterior, an axillary lateral, and an outlet view should be obtained to assess for joint space narrowing, subacromial spurs, acromial fracture, and implant positioning. Displaced suture anchors may be seen in cases of recurrent rotator cuff tears (Fig. 18-1). Superior migration of the humeral head is associated with chronic large and massive tendon tears. Some postulate that when the acromial–humeral distance is less than 7 mm, the tear is irreparable or, at best, has a low chance to heal.
Ultrasound has been used to effectively evaluate the rotator cuff. Specificity has been reported to range from 86% to 100%.43,44
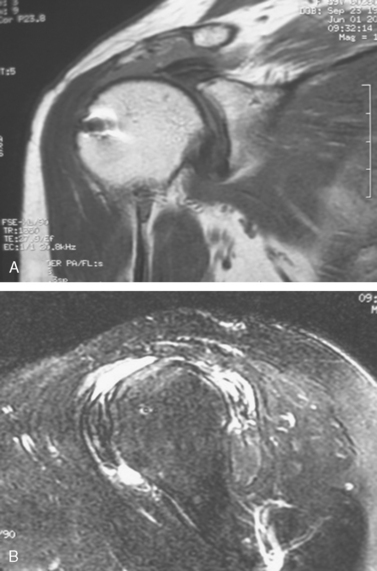
MRI scans are very useful in the postoperative setting to evaluate both the cuff and other intra-articular structures (Fig. 18-2).11 In Gaenslen’s study,11 they diagnosed articular cartilage damage as well as a ganglion cyst in the supraspinatus muscle. Neither of these findings would have been evident on ultrasound. Muscle atrophy and tendon retraction, as visualized on MRI, can give a surgeon a good idea of the type of tissue quality that can be expected at the time of surgery.
Treatment and Outcomes
Physical therapy and activity modification, débridement, anatomic repair, partial repair, augmentation with biological materials, and tendon transfer have all been used with varying degrees of success to treat recurrent rotator cuff repairs.6,21,45–49 Patient factors such as age, medical condition, activity level, and degree of functional impairment influence specific treatment recommendations. In general, however, given the relatively inferior outcomes of revision acromioplasty and rotator cuff repair, a trial of nonoperative treatment is warranted.1,6,7,9 Physical therapy is the hallmark of nonsurgical treatment, but attention should be given to activity modification. If the patient fails this course of conservative management and has realistic expectations regarding function after surgery, revision rotator cuff surgery is indicated.
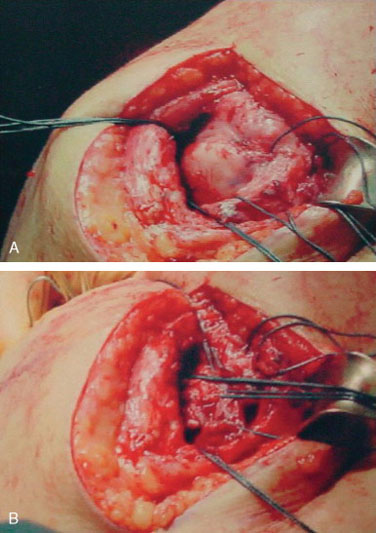
When the entire defect is not reparable, partial repair has been shown to decrease strain at the free margins, resulting in improved function.50 Additionally, if necessary, tendon transfer can be used to treat the residual defect. Latissimus dorsi transfer is used for patients with posterosuperior tears with weak external rotation (Fig. 18-3).21,22,51,52 When done in conjunction with primary repair of a massive cuff tear, the transfer is effective in stabilizing external rotation function to the degree necessary to allow active elevation to 90 degrees.53 In revision cases, even in the hands of experienced shoulder surgeons, the results of this salvage procedure have been variable. Pectoralis major transfers can be considered in cases of anterior cuff insufficiency or for loss of the subscapularis tendon.54,55 Tendon transfers should be viewed as salvage procedures. These are technically demanding procedures that provide mixed outcomes, at best.56
Much work has focused on the use of biologicals to enhance or augment rotator cuff healing. Theoretically, augmentation devices, such as small intestine submucosa patches, provide an absorbable scaffold to reinforce the repair and to stimulate healing.48,57,58 Recent literature does not support their use, however, given the significant inflammatory reactions that can occur combined with the lack of clinical benefit.47,59 Walton and colleagues compared a group of patients undergoing standard rotator cuff repair to a group undergoing repair augmented by xenograft (Restore Orthobiologic Implant).47 At 2 years after surgical repair, patients with xenograft had no recognizable benefit compared to the control group, and 4 of 10 patients treated with the xenograft had severe inflammatory reactions requiring second surgeries. At this point, there is not enough supporting evidence to recommend use of these products in revision rotator cuff repair cases. Ongoing research using growth factors to enhance the tendon healing process might prove valuable in the revision setting; however, clinical trials are necessary before their potential roles can be delineated.60–62
After revision rotator cuff repair, patients should be placed in a sling with an abduction pillow that places the arm in about 15 degrees of abduction, for 6 weeks. During this time, stiffness is avoided by allowing passive motion, including nonprovocative pendulums and circles and saws. After the initial period of limited mobilization, the patient may begin active assisted range of motion and isometric exercises. Weights and resistive exercises should be avoided for the first 3 months.18 After this period, light elastic band–resisted exercises may be performed at below shoulder level. Patients are progressed slowly, realizing that adequate rehabilitation after revision rotator cuff repair usually takes about 9 months.
Appropriate diagnosis, surgical technique, and postoperative rehabilitation are all critical to give patients the best chance for a successful outcome; however, the results of revision rotator cuff repair are less predictable than primary repair outcomes. DeOrio and Cofield were the first to publish results on revision rotator cuff repairs.6 They followed up patients at a minimum of 2 years after surgery. Only 4 of 27 patients were considered to have a good result. Seven required a second revision rotator cuff repair, and 3 of these 7 eventually required a glenohumeral arthrodesis. They did find that 76% of the patients had reduced pain. Bigliani and associates reported better results in their series. Nineteen percent of patients had excellent results, 32% had good results, 23% reported fair outcomes, and 26% had poor results.1 Worse results were associated with previous lateral acromionectomy, detachment of the deltoid origin, and poor tendon quality at the time of re-repair.
Neviaser and colleagues performed revision rotator cuff repairs in 50 patients.9 They critically evaluated range of motion and found that more than 50% of patients gained motion and had decreased pain after revision surgery. Djurasovic and coworkers reported on the largest series of revision rotator cuff repairs.7 Of the 80 patients with retears, initial tear size was classified as massive in 22, large in 28, medium in 10, and small in 13. At the time of revision, 45% of the cases required interval slides, and 24 patients required deltoid repair to the acromion. Overall results of revision repairs were excellent in 33%, good in 25%, fair in 9%, and poor in 31%. An intact deltoid origin was a good prognostic indicator, because 78% of the patients with such a finding had a satisfactory outcome compared to only 57% satisfaction in patients with a deltoid injury. Djurasovic and colleagues also found that poor tendon quality, decreased preoperative active range of motion, and an increased number of prior procedures were all associated with poor outcomes.
Lo and Burkhart were the first to report on the results of arthroscopic revision rotator cuff repairs.8 They revised 11 massive tears, 1 large tear, and 2 medium-sized tears. It was a small mixed series of patients, including 7 involved in workers’ compensation claims and 5 with superior migration of the humeral head. Five of the patients had concomitant pathology, including persistent acromial spurs, SLAP (superior labrum anterior and posterior) lesions, and biceps tendinopathies. Overall, there were 4 excellent, 5 good, 4 fair, and 1 poor result. They concluded that arthroscopic revision is a viable method for treating these complex problems.
Authors’ Preferred Treatment
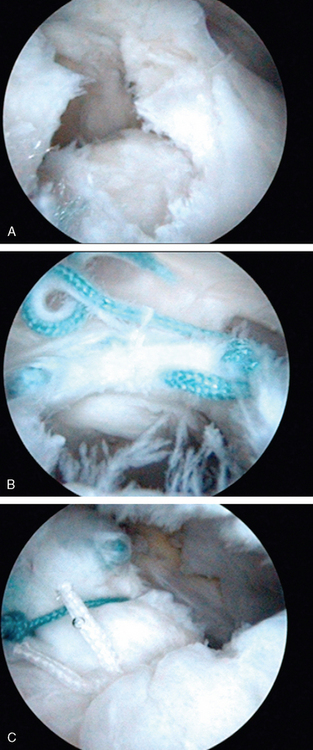
In cases where tear configuration precludes direct repair to the tuberosity, the tear shape must be recognized, and appropriate interval repairs or margin conversions must be carried out using heavy nonabsorbable suture. This is achieved with any of the available arthroscopic suture-passing instruments and appropriate knot-tying techniques. Arthroscopic techniques facilitate this type of closure. Even in cases where the surgeon wishes to use a mini-open technique, this part of the procedure is facilitated by the arthroscopic observation and techniques that can be used. In some cases, this is all that can be done. However, if after the side-to-side repair is performed, the tendon can be advanced to the footprint, we then proceed with suture anchor repair (Fig. 18-4).
In most revision cases, when possible, we use a double-row technique. Arthroscopic advances using transosseousequivalent repairs provide a nice tool to re-establish the rotator cuff footprint.37 Double-row repairs are particularly useful in cases when the index procedure was fixed with one row of anchors. In the revision setting, we commonly put a row of anchors medial to the previous fixation site and a row lateral to the site. This creates a strong construct that spans the previous site of fixation, enabling us to avoid putting more anchors in what is most likely poor-tuberosity bone stock.
PERSISTENT SUBACROMIAL IMPINGEMENT
Etiology
In several studies, inadequate supraspinatus outlet decompression has been implicated as a cause of failed rotator cuff repairs.1,7,63–66 It can be the result of residual anterior acromial spurring, regrowth or persistence of the coracoacromial ligament, subacromial calcification, or inferiorly projecting acromioclavicular osteophytes.63,65–70 Persistent impingement syndrome as a cause of pain after rotator cuff surgery has been reported in 18% to 79% of patients with failed acromioplasty.63–66 The true incidence of inadequate decompression or persistent impingement, however, is unknown.
There is still debate surrounding the surgical indications, technique, and optimal amount of acromioplasty to relieve supraspinatus outlet narrowing.71,72 Gartsman and colleagues performed a randomized study on the efficacy of concomitant subacromial decompression during rotator cuff repair.72 The study was limited to patients with full-thickness supraspinatus tears and type II acromial morphology. At an average of 2 years after surgery, there was no statistically significant difference in mean American Shoulder and Elbow Surgeons (ASES) scores of the decompression group compared to the repair group without decompression. Other studies support the association between type III acromial morphology and rotator cuff tear size.73
Despite the differing opinions, a couple of studies on failed rotator cuff repairs have implicated inadequate acromioplasties as at least part of the reason for the failures.1,7 Bigliani noted that 5 of the 31 patients in his series did not undergo acromioplasty during the initial rotator cuff repair, and the remaining patients needed revision acromioplasty during their subsequent rotator cuff surgery.1 Another study reported on the results of revision rotator cuff repair in 80 patients.7 Of this group, 53 patients (66%) required acromioplasty at the time of revision, either because of inadequate bone resection during the index procedure or because of failure to address the acromial morphology during the initial repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree