Epiphysiodesis
William C. Warner Jr
David D. Spence
INDICATIONS/CONTRAINDICATIONS
Epiphysiodesis is a technique used to stop the growth of an open growth plate or physis. The indications for epiphysiodesis, either complete or partial, are treatment of a leg-length inequality, correction of angular deformities, or prevention of progressive limb-length inequality in a growing child. Several methods have been described to treat limb-length inequalities (Fig. 31-1). These methods range from a simple shoe lift to limb lengthening or limb shortening (1, 2, 3). Although limb shortening can consist of an acute shortening of the femur or tibia, the most common method is slowing or stopping the growth of the longer extremity by epiphysiodesis.
Phemister (4) is credited with the first description of the epiphysiodesis technique. With the Phemister technique, a 1-cm rectangular bone block is removed from the lateral and medial aspects of the bone, with the bone block centered on the physis. The physis is curetted, and the bone block is reinserted after being rotated 180 degrees. White and Stubbins (5) described a technique using an osteotome or mortising chisel to remove intact a 1-in.-deep cube of bone containing the physis. A large portion of the remaining physis is removed with curettes. After the physis is curetted, the cube of bone is rotated 90 degrees and replaced in its original bed. Blount and Clarke (6) described the use of staples to obtain an epiphysiodesis, noting that three staples on each side (medial and/or lateral) were needed to stop growth of the physis. When one staple was used, the staple would break; when two staples were used, the staples would bend, leading to separation of the staple prongs. Staples have the theoretical advantage of resumption of normal growth once the hardware is removed; however, indications for this technique have narrowed because of complications related to loosening or breakage of the staples and the often-unpredictable arrest of growth. Tension-band plating is an alternative to stapling as a means of obtaining growth arrest with the potential for resumption of normal growth upon removal of the implants, but Stewart et al. (7) demonstrated that tension-band plating was not as effective as was physeal ablation in obtaining desired correction. Metaizeau et al. (8) described a technique for performing epiphysiodesis using screws placed percutaneously with fluoroscopic imaging across the physis in a diagonal or longitudinal fashion. This technique may be used selectively when protective weight bearing is not a viable option but has also been shown to have a delayed effect in physeal closure compared with physeal ablation, making the timing less predictable. Song et al. (9) and Ilharreborde et al. (10) noted that epiphysiodesis with the percutaneous screw technique may have a delayed effect of 6 months to 1 year. Therefore, if this method is used, it should be performed 6 months to 1 year earlier than predictions suggest.
The open Phemister method has been the standard technique to obtain growth arrest of the physis but has largely been replaced by percutaneous techniques. Canale and Christian (11), Ogilvie and King (12), and Timperlake et al. (13) described percutaneous techniques for epiphysiodesis that are attractive alternatives to traditional open procedures and have become the technique of choice in our institution for definitive physeal closure. Percutaneous epiphysiodesis has the advantages of reliable results, little morbidity, and small incisions that produce a better cosmetic result (14, 15). The percutaneous epiphysiodesis method has been performed using a single-incision technique instead of the usual double-incision technique; however, increased complications have been noted with the single-incision technique, and it is not recommended (16).
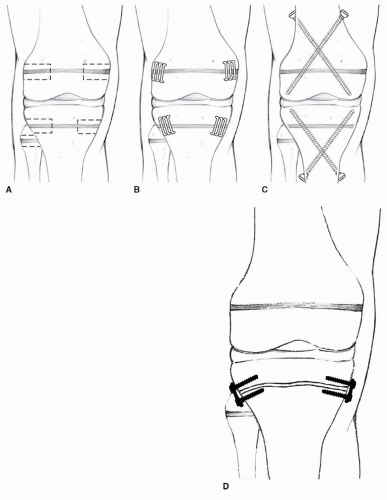 FIGURE 31-1 Epiphysiodesis can be done by several techniques. A. Phemister technique. B. Blount staples. C. Metaizeau technique. D. Tension-band plating. |
Preoperative Planning
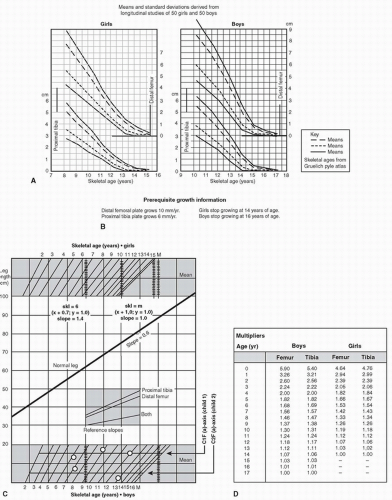
Several authors have reported that errors in timing remain the primary problem with using epiphysiodesis for limb equalization (17, 18, 19, 20, 21). The treating surgeon must be able to accurately predict the expected leg-length discrepancy at maturity. Remaining growth in the long leg and the short leg must be predicted accurately, and any growth inhibition in the involved extremity must be accounted for to ensure a successful result. Moseley (2) described three steps that must be done before recommending treatment for a leg-length discrepancy: (a) assessment of past growth, (b) prediction of future growth, and (c) prediction of the effect of surgery (22). Several methods can be used to predict the growth remaining in the lower extremities. The four most accepted methods of predicting the final leg-length discrepancy at maturity are (Fig. 31-2) (a) the growth-remaining charts of Anderson et al. (22, 23), (b) the arithmetic method reported by Menelaus (24) and Westh and Menelaus (25), (c) the Moseley straight-line graph (26, 27), and (d) the multiplier method described by Aguilar et al. (28) and Paley et al. (29).
Potential inaccuracies certainly exist in the calculation of growth remaining, and timing of an epiphysiodesis can affect the final outcome obtained from surgery. The two most common sources of error are predictions of the exact date of skeletal maturity and the presence of any significant growth inhibition in the involved extremity. Skeletal maturity or determination of the time that growth in the lower extremities will cease has been based on chronologic age or skeletal bone age as assessed radiographically. The inaccuracies of using only the chronologic age become obvious when one considers the treatment of two 12-year-old girls. One 12-year-old girl can have a bone age of 14 years and be postmenarchal with little growth remaining in the lower extremities, while another can have a bone age of 10 years and be premenarchal, with significant growth left in the lower extremities. Using the skeletal age as determined by a left hand and wrist radiograph for bone age based on the Greulich and Pyle’s atlas of standards (30) may improve the accuracy of determining skeletal maturity (31), although this is still somewhat of an approximation. Menelaus (24) suggested that if the bone age is within 1 year of the chronologic age, then the chronologic age would give an accurate assessment of skeletal maturity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree