CHAPTER 106 Epidural Adhesiolysis
INTRODUCTION
Chances are each of us will experience low back pain at some point in our lives. The usual course is rapid improvement, but 5–10% of patients develop persistent symptoms.1 In 1997, the total impact of low back pain on industry in the United States was estimated at US$171 billion.2 The medical treatment of low back pain in 1990 amounted to US$13 billion.3 Treatment varies from conservative therapy with medication and physical therapy to minimally and highly invasive pain management interventions. Surgery is sometimes required in those patients who have progressive neurological deficits or those who have failed other therapies. Surgery is successful in the majority of patients, but an unlucky few continue to have pain and neurological symptoms. A quandary arises as to whether a repeat surgery should be attempted or an alternative intervention should be sought. This is the exact quandary that the epidural adhesiolysis procedure was designed to address. It was developed to break down scar formation, deliver site-specific corticosteroids and local anesthetic drugs directly to the target, and reduce edema with hypertonic saline. Epidural adhesiolysis has afforded patients reduction in pain and neurological symptoms without the expense and sometimes long recovery period associated with repeat surgery, and often prevents the need for surgical intervention.
PATHOPHYSIOLOGY OF EPIDURAL FIBROSIS (SCAR TISSUE) AS A CAUSE OF LOW BACK PAIN WITH RADICULOPATHY
The etiology of low back pain with radiculopathy is not well understood. Kuslich and colleagues addressed this issue when they performed 193 lumbar spine operations on patients given local anesthesia. Their study revealed that sciatica could only be produced by stimulation of a swollen, stretched, restricted (i.e. scarred) or compressed nerve root.4 Back pain could be produced by stimulation of several lumbar tissues, but the most common tissue of origin was the outer layer of the anulus fibrosus and posterior longitudinal ligament. Stimulation for pain generation of the facet joint capsule rarely generated low back pain, and facet synovium and cartilage surfaces of the facet or muscles were never tender.5
The contribution of fibrosis (scar tissue) to the etiology of low back pain has been debated.6–8 There are many possible etiologies of epidural fibrosis, including surgical trauma, an annular tear, infection, hematoma, or intrathecal contrast material.9 These etiologies are well documented in the literature. LaRocca and Macnab10 demonstrated the invasion of fibrous connective tissue into postoperative hematoma as a cause of epidural fibrosis, while Cooper and colleagues11 reported periradicular fibrosis and vascular abnormalities occurring with herniated intervertebral discs. McCarron et al.12 investigated the irritative effect of nucleus pulposus upon the dural sac, adjacent nerve roots, and nerve root sleeves independent of the influence of direct compression upon these structures. Evidence of an inflammatory reaction was identified by gross inspection and microscopic analysis of spinal cord sections after homogenized autogenous nucleus pulposus was injected into the lumbar epidural space of four dogs. In the control group consisting of four dogs injected with normal saline, the spinal cord sections were grossly normal. Parke and Watanabe showed significant evidence of adhesions in cadavers with lumbar disc herniation.13
It is widely accepted that postoperative scar renders the nerve susceptible to injury via compressive phenomena.8 It is natural for connective tissue or any kind of tissue to form fibrous layers (scar tissue) as a part of the process that transpires after disruption of the intact milieu.14 Scar tissue is generally found in three components of the epidural space. Dorsal epidural scar tissue is formed by resorption of surgical hematoma and may be involved in pain generation.15 In the ventral epidural space, dense scar tissue is formed by ventral defects in the disc, which may persist despite surgical treatment and continue to produce low back pain/radiculopathy past the surgical healing phase.16 The lateral epidural space includes epiradicular structures outside the root canals, known as the lateral recess or ‘sleeves’ containing the exiting nerve root and dorsal root ganglia, which are susceptible to lateral disc defects, facet overgrowth, and neuroforaminal stenosis.17
Although scar tissue itself is not tender, an entrapped nerve root is. Kuslich et al.4 surmised that the presence of scar tissue compounded pain associated with the nerve root by fixing it in one position and thus increasing the susceptibility of the nerve root to tension or compression. They also concluded that no other tissues in the spine are capable of producing leg pain. In a study of the relationship between peridural scar evaluated by magnetic resonance imaging (MRI) and radicular pain after lumbar discectomy, Ross et al. demonstrated that subjects with extensive peridural scarring were 3.2 times more likely to experience recurrent radicular pain.18
RADIOLOGIC DIAGNOSIS OF EPIDURAL FIBROSIS
Magnetic resonance imaging and computed tomography (CT) scanning are diagnostic tools with 50% and 70% sensitivity and specificity, respectively.14 CT-myelography may also be helpful. None of these imaging techniques can identify epidural fibrosis with 100% reliability. In contrast, epidurography is a technique used with considerable success and it is believed that epidural fibrosis is best diagnosed by performing an epidurogram.19–22 It can detect filling defects in good correlation with a patient’s symptoms in a real-time manner.22 A combination of more than one of these techniques will undoubtedly increase the ability to identify epidural fibrosis.
INDICATIONS FOR EPIDURAL ADHESIOLYSIS
Although originally designed to treat radiculopathy secondary to epidural fibrosis following surgery, the use of epidural adhesiolysis has been expanded to treat a multitude of pain etiologies. These include:23
Contraindications to epidural adhesiolysis include the following absolute contraindications:
Anticoagulant medication
Medications that prolong bleeding parameters should be withheld prior to performing epidural adhesiolysis. The length of time varies depending on the medication taken. A consultation with the patient’s primary physician should be obtained prior to stopping any of these medications. Nonsteroidal antiinflammatory drugs (NSAIDs) and aspirin should be withheld 4 days and 7–10 days prior to the procedure, respectively. Although there is much debate regarding these medications and neuraxial procedures, the authors tend to be on the conservative side. Clopidogrel (Plavix®) should be stopped 7 days prior to the adhesiolysis while ticlopidine (Ticlid®) is held 10–14 days prior.24 The warfarin (Coumadin®) withholding period is patient variable, but 5 days is usually adequate.24 Subcutaneous heparin administration should be stopped at a minimum of 12 hours prior to the procedure, while low molecular weight heparin requires a minimum of 24 hours.24 Over-the-counter medications that prolong bleeding parameters should also be withheld. These include vitamin E, gingko biloba, garlic, ginseng, and St. John’s Wort. In addition, a prothrombin time, a partial thromboplastin time, and a platelet function assay or a bleeding time is obtained to check for coagulation abnormalities. Any elevated value warrants further investigation and postponement of the procedure until those studies are complete.
TECHNIQUE
Caudal approach
An epidurogram is performed using 10 mL of a non-ionic, water-soluble contrast agent. Confirm a negative aspiration for blood or cerebrospinal fluid (CSF) prior to any injection of contrast or medication. Omnipaque® and Isovue® are the agents most frequently used and are suitable for myelography.25,26 Do not use ionic, non-water-soluble contrast agents such as Hypaque® or Renagraffin® or ionic, water-soluble agents such as Conray®.27,28 These agents are not indicated for myelography. Accidental subarachnoid injections can lead to serious untoward events such as seizure and possible death. Slowly inject the contrast agent and observe for filling defects. A normal epidurogram will have a Christmas-tree pattern with the central channel being the trunk and the outline of the nerve roots making up the branches. An abnormal epidurogram will have areas where the contrast does not fill. These are the areas of presumed scarring and typically correspond to the patient’s back and radicular complaints. If vascular uptake is observed, the needle needs to be redirected.
After turning the distal opening of the needle ventrolaterally, insert a TunL Kath™ or TunL-XL™ (stiffer) catheter (Epimed International®) with a bend on the distal tip through the needle. The bend should be 2.5 cm from the tip of the catheter and at a 30° angle. The bend will enable the catheter to be steered to the target level. Under continuous AP fluoroscopic guidance, advance the tip of the catheter towards the ventrolateral epidural space of the desired level. The catheter can be steered by gently twisting the catheter in a clockwise or counterclockwise direction. Avoid ‘propellering’ the tip, i.e. twisting the tip in circles, as this makes it more difficult to direct the catheter. Do not advance the catheter up the middle of the sacrum as this makes guiding the catheter to the ventrolateral epidural space more difficult. Ideal location of the tip of the catheter in the AP projection is in the foramen just below the midportion of the pedicle shadow (Fig. 106.1A). Check a lateral projection to confirm that the catheter tip is in the ventral epidural space (Fig. 106.1B).
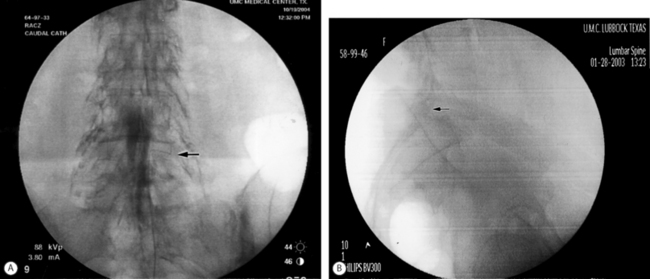
Fig. 106.1 (A) Catheter tip at the left L4–5 foramen. (B) Catheter in the ventral epidural space at L5–S1.
A 20 minute period should elapse between the last injection of the LA/S solution and the start of the hypertonic (10%) saline infusion. This is necessary to ensure that a subdural injection of the local anesthetic/steroid solution has not occurred. A subdural block can mimic a subarachnoid block but takes longer to establish. If the patient develops a subarachnoid or subdural block at any point during the procedure, the catheter should be removed and the remainder of the adhesiolysis canceled. The patient needs to be observed to document the resolution of the motor and sensory block and to document the absence of bladder/bowel dysfunction. Ten milliliters of hypertonic saline is then infused through the catheter over 30 minutes. If the patient complains of discomfort, the infusion is stopped and an additional 2–3 mL of 0.2% ropivacaine is injected and the infusion is restarted. Alternatively, 50–100 mg of fentanyl can be injected epidurally in lieu of the local anesthetic. After completion of the hypertonic saline infusion, the catheter is slowly flushed with 2 mL of preservative-free normal saline and the catheter is capped.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








