Environmental Issues for the Athlete
Mark D. Bracker MD
Marjorie Delo MD
Elise T. Gordon DO, CDR, MC, USN
Judy R. Schauer DO, CDR, MC, USN
Body temperature is maintained in a narrow range by an integrated system of internal and external processes.
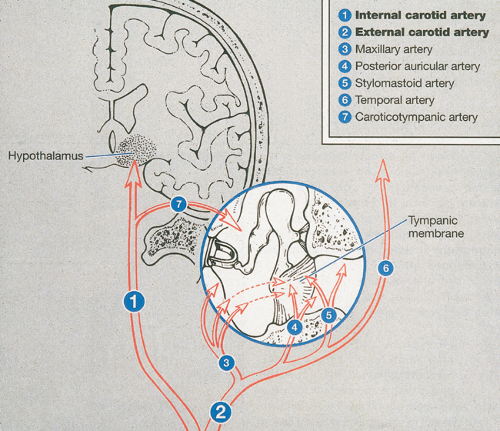
Internal homeostasis is controlled by the hypothalamus, with the parasympathetic nervous system regulating sweat gland function and the sympathetic nervous system controlling changes in skin blood flow and vasodilatation.
Evaporation of sweat is the primary means of cooling once the environmental temperature exceeds 68°F.
A large number of medications can decrease the ability of the athlete’s body to regulate internal temperature. Performance-enhancing supplements, such as ephedra, have been implicated as deleterious to the process.
The type of clothing worn and pre-existing medical conditions can also affect thermoregulation of the athlete.
An athlete who has acclimated to elevated temperature will need increased fluid intake because normal sweating rates may double.
Three primary heat illnesses—heat cramps, heat exhaustion, and heat stroke—are common to athletic populations.
In American high school athletics, heat stroke has been the third leading cause of death behind only head and neck trauma and cardiovascular disorders.
Individuals affected by heat cramps experience painful muscle contractions primarily in the arms, calves, and abdomen. Other symptoms include nausea, vomiting, fatigue, and lightheadedness.
Athletes with heat exhaustion present with symptoms of fatigue, inability to continue activity, mild confusion, nausea, vomiting, chills, piloerection, and profuse sweating.
It is imperative to begin treatment of heat exhaustion as soon as it is identified because this condition can progress to heat stroke, which is a medical emergency.
Symptoms of heat exhaustion and heat stroke are very similar, and therefore, on the field, efforts should be directed at cooling the patient immediately as though the patient has heat stroke. If in doubt, transporting the patient to the emergency department is the most prudent action.
Practices that may have contributed to the heat exhaustion episode (e.g., poor diet, insufficient fluids, etc.) should be examined, and corrective actions should be taken to prevent repeat occurrences.
Exertional heat stroke, a medical emergency, is defined by a core temperature greater than 104°F and severe central nervous system (CNS) disturbances, resulting in loss of homeostasis and damage to multiple organ systems.
In the field, a presumptive diagnosis of exertional heat stroke may be made when the patient is hot, environmental conditions are conducive to heat injury, and there are signs of moderate to severe CNS dysfunction.
CNS involvement is the hallmark, but the cardiovascular, integument, renal, splanchnic, and hepatic systems are also damaged by heat stroke.
People visit areas at altitudes greater than 2,500 m and engage in activities ranging from sedentary to strenuous. Physicians practicing in this setting should become familiar with the signs and symptoms of various high-altitude syndromes.
During ascent, increased sympathetic activity results in increased blood pressure, heart rate, cardiac output, and venous tone.
All of the acute mountain sickness syndromes are a result of neurohumoral and hemodynamic changes occurring when humans become hypoxic. First-line therapy, specifically descent and oxygen, is the same for any syndrome in the spectrum.
High-altitude illness risk can be decreased through slow ascent and wise choice of sleeping altitude.
Hypothermia and frostbite are the result of prolonged exposure to the elements without proper insulation, elemental protection, or energy stores.
Exposure to cold conditions can lead to disease on a local or systemic level. Local disease ranges from frostnip, which does not cause permanent damage, to deep frostbite, which leads to irreversible damage to bones, joints, and muscle tissues. Systemic cold injury, or hypothermia, affects the entire body’s metabolic and cellular function.
Hypothermia refers to a decline in core temperature below 35°C.
Winter sports enthusiasts and mountaineers are increasingly being treated for injury related to cold exposure.
The risk of dying from hypothermia increases at the extremes of age.
Emergency medical personnel can minimize injury from cold by rapidly removing the victims from further danger, insulating and immobilizing them, and transporting them to treatment facilities.
Recent high-profile deaths of high school, collegiate, and professional athletes from heat stroke have once again alerted physicians, athletic trainers, and coaches alike of the importance of recognizing and promptly treating heat-related illnesses (1,2).
Basic Science
Normal Human Temperature Regulation
Body temperature is maintained in a narrow range by an integrated system of internal and external processes. Internal thermal homeostasis is controlled by the hypothalamus, with the parasympathetic nervous system regulating sweat gland function and the sympathetic nervous system controlling changes in skin blood flow and vasodilatation (3) (Fig 57-1). As environmental temperatures rise, blood flow is diverted to the skin, and sweat production increases (3,4). The rate of sweat production is affected by, among other factors, the acclimatization of the athlete being challenged. In general, a sweat rate of 1 to 2 L per hour with a sodium content of 65 mEq per L is achieved in the nonacclimatized individual (3,5). With the physiological changes of heat adaptation, the sweat rate increases to 3 to 4 L per hour, and the sodium concentration drops to 5 mEq per L (5).
Mechanisms of Heat Transfer
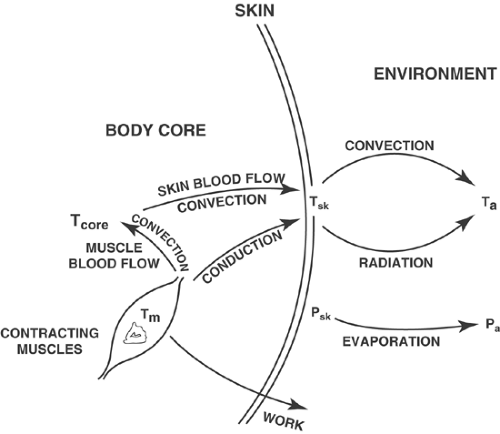
Available mechanisms of cooling include conduction, convection, radiation, and evaporation (Fig 57-2) (6). Conduction is the transference of heat from one body to another cooler one by direct contact. Air can act as an insulator to heat loss,
whereas water provides better conduction of heat, which is key in its use for immersion cooling.
whereas water provides better conduction of heat, which is key in its use for immersion cooling.
Convection is transfer of heat to the surrounding circulating air. With elevated ambient temperatures, as when the air temperature is greater than the skin temperature, heat can actually be transferred to the skin.
Radiation is dispersal of heat in the form of infrared electromagnetic waves. These first three mechanisms are most useful for cooling when the ambient temperature is less than or equal to the skin temperature (3). In humans, by far the most important method of heat dissipation is evaporation (7). As sweat forms on the skin, surrounding warmer air evaporates the fluid, thus providing cooling. Evaporation of sweat is the primary means of cooling once the environmental temperature exceeds 68°F (20°C) (8,9). Each milliliter of evaporated sweat cools the body by 0.58 kcal (3); evaporative losses are influenced by wind current and clothing and, most importantly, by the relative humidity. Sweat that is not evaporated, as when there is elevated humidity, but instead rolls off and/or is absorbed by clothing does not provide the needed cooling.
Other Influences on Thermoregulation
The ability of the athlete to function in a hot environment is determined by many factors. Two of them, the physiological mechanisms available for cooling and acclimatization of the individual, have been mentioned. Also affecting thermoregulation of the athlete is the clothing worn, medications that are being used, and pre-existing medical illnesses. Recent National Collegiate Athletic Association (NCAA) guidelines support the gradual introduction of heavier uniform items such as full padding during the acclimatization process (10). Lighter clothing allows sweat to be wicked away from the body as it is more easily evaporated.
A large number of medications can decrease the ability of the athlete to regulate internal temperatures. These include antihistamines, anticholinergics, benzodiazepines, alpha-adrenergics, beta- and calcium blockers, neuroleptics, phenothiazines, diuretics, and tricyclic antidepressants (6,11). In addition, drugs such as alcohol, cocaine, amphetamines, and ecstasy can adversely affect thermoregulation (4,6). Performance-enhancing supplements (e.g., ephedra) have also been implicated as deleterious to maintaining normal core temperatures (1). All medications and supplements must be identified to allow effective counseling with regard to performance and safety concerns.
Many pre-existing medical conditions can contribute to an individual’s inability to adapt and function in a hot environment. These include alcoholism, anorexia, cardiac disease, cystic fibrosis, dehydration, diabetes insipidus, extremes of age, febrile illnesses, gastroenteritis, hypokalemia, obesity, poor conditioning, sleep deprivation, sunburn, and sweat gland dysfunction (3,4,6). Of note, anorexia (along with other eating disorders), dehydration, and gastroenteritis are conditions that are commonly observed in young populations. Coaches, athletic trainers, and physicians must be ready to identify those at risk. Furthermore, these multiple and diverse risk factors for heat illness highlight the importance of preparticipation screening as well as periodic medical updates to allow appropriate and individualized levels of play and/or activity in hot environments.
A history of previous heat injury has been listed as elevating the risk of subsequent heat illnesses. While it is true that activity modification is necessary as the athlete recovers from an illness, recent studies have not shown that an episode of heat injury universally predisposes to future episodes (12,13).
Acclimatization
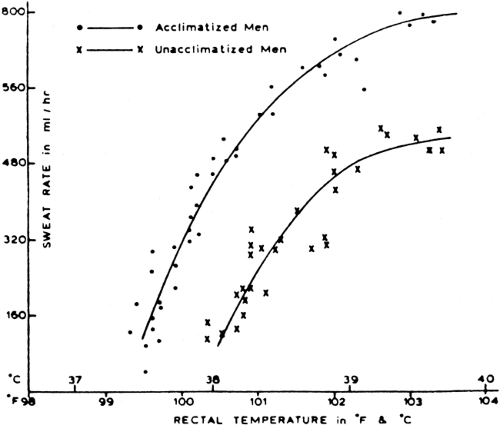
Gradual acclimatization to a warm, humid environment is an important process in preventing heat-related illnesses. Normally taking 10 to 14 days to accomplish, it is a series of gradual physiological adaptations to heat that occurs with regular exposure to and exercise in a hot environment (13,14). Physiological changes that improve tolerance to heat include an increase in blood volume, an increase in sweat rate with a faster onset of sweating, a wider distribution of areas producing sweat, and a decrease in the sweat sodium concentration (Fig 57-3).
There is a common misconception that, as the athlete acclimates to elevated temperature, there is a concomitant decrease in hydration requirement. The converse is true; normal sweating rates may double, thus significantly increasing the required fluid intake to maintain euhydration.
The significance of adequate hydration cannot be overemphasized. It has been estimated that for each 1% decrease in body weight secondary to dehydration, the core temperature increases by 0.15 to 0.2°C (7,15). Increased sweat rates add to the dehydrated state with hemodynamic instability resulting. Results of a recent study of high school athletes showed that over 60% began summer practice sessions in a dehydrated state, based on a initial urine-specific gravity of greater than 1.020 (16). Thirst is not a reliable indicator of volume status because a level of 2% to 3% dehydration is necessary to initiate this response (7). This level of dehydration is not uncommon with normal practice conditions and has also been noted to impair athletic performance. With thirst as the sole prompter of fluid ingestion, an athlete will only ingest one third to two thirds of fluid loss as sweat (17).
Measuring Heat Stress
Assessment of environmental conditions that increase risk of heat illnesses is another important step in injury prevention. A number of indices have been developed to attempt to define site-specific risk. One of the most widely known and used is the Wet Bulb Globe Temperature (WBGT) Index (13). Using three measurements to reflect dry temperature,
humidity, and radiant heat effects and weighting them for importance, the generated score is correlated to a certain degree of danger from heat exposure. In this way, activities can be modified to reduce potential harm (18). The National Weather Index is another tool to evaluate heat exposure but is not specific to the area of play (4). While a WBGT meter is expensive, a more affordable method uses a sling psychrometer, and a free program is available on the internet (19).
humidity, and radiant heat effects and weighting them for importance, the generated score is correlated to a certain degree of danger from heat exposure. In this way, activities can be modified to reduce potential harm (18). The National Weather Index is another tool to evaluate heat exposure but is not specific to the area of play (4). While a WBGT meter is expensive, a more affordable method uses a sling psychrometer, and a free program is available on the internet (19).
Clinical Evaluation
Three primary heat illnesses are common to athletic populations: heat cramps, heat exhaustion, and heat shock. The actual incidence of the first two is not known because these are often treated on the field with referral for recalcitrant symptoms only. For the years of 1990 to 1995, there were 84 deaths among U.S. football players attributed to heat stroke (20). In 1995 alone, there were five heat-related deaths among American athletes (21). In American high school athletes, heat stroke has been listed as the third leading cause of death, following only head and neck trauma and cardiovascular disorders (22). Four teenage football players died in early August 2004 with heat-related illnesses as the probable cause (1).
With heat stroke being a largely preventable cause of death and the opinion of many that there is a continuum in the severity of heat illness symptoms, it is important to recognize the characteristics of each and act accordingly to prevent progression to a more hazardous condition.
Heat Cramps
With heat cramps, affected individuals experience painful muscle contractions primarily in the arms, calves, and abdomen, with inadequate electrolyte intake being the probable etiology. Athletes complain of extremity cramping in the most worked muscle groups and often after the activity has stopped. Other symptoms include nausea, vomiting, fatigue, and lightheadedness. Risk factors for heat cramps include the use of diuretics (as caffeinated beverages), unacclimatized state, and inadequate sodium intake. A classic study of workers in several industrial settings demonstrated four characteristics of heat cramps that are still valid: (a) contractions occur after sustained heavy effort in a hot environment; (b) affected individuals sweated profusely; (c) fluid replacement consisted of large volumes of water; and (d) cooling seemed to precipitate the spasms because they began after cessation of work (23).
Clinically, patients may appear ill and uncomfortable secondary to the cramping, and sweating will be noted. If measured, the rectal temperature would be below 104°F. Treatment involves removal of the patient to a cool environment, encouraged oral hydration with electrolyte-containing solutions, and stretching/massage of affected muscle groups. If fluid replenishment cannot be accomplished orally secondary to vomiting, parenteral hydration can be initiated. An athlete can return to play if, after treatment, he can successfully participate at the level expected for the sport and position played (24).
Heat Exhaustion
Athletes with heat exhaustion present with symptoms of fatigue, inability to continue activity, mild confusion, nausea, vomiting, chills, piloerection, and profuse sweating. Heat syncope may occur, but there is no major neurological impairment. Hypotension, hyperventilation, and elevated rectal temperatures are objective evidence for heat exhaustion.
Physiologically, affected athletes may be either volume depleted or sodium depleted, although there is often an overlap between the two types of heat exhaustion (4). Water-depleted heat exhaustion is most often observed in elderly populations (as a result of medications that affect hydration status) and in active individuals who are inadequately hydrated for the activity level and the environmental conditions.
Sodium-depleted heat exhaustion, on the other hand, is seen in unacclimatized persons who have overhydrated, taking in sufficient free water, but have not accounted for sodium losses in sweat by altering intake. Acclimatization increases sweat rates but concomitantly decreases sodium content in sweat.
Treatment of heat exhaustion depends on the type and degree of impairment. For mild heat exhaustion, in which the patient is hemodynamically stable, removal to a cool environment, removal of excess equipment and clothing, and replenishment of fluids orally are usually sufficient. Electrolyte/salt replacement is provided as needed (4).
Patients with more severe manifestations (hypotension, cardiac arrhythmias, or deteriorating mental status) or those unresponsive to conservative measures must be transported to emergency medical facilities. Although intravenous hydration may be initiated prior to transport, the volume of saline administered must be modest until electrolyte concentrations can be accurately measured. Heat exhaustion patients who are hypernatremic will need cautious hydration to avoid the cerebral edema caused by too rapid a correction.
It is imperative to begin the treatment of heat exhaustion as soon as it is identified because this condition can progress to heat stroke, which is a medical emergency. Because heat exhaustion and heat stroke symptoms are so similar and assessment of core temperatures may not be possible on the field, efforts should be directed at cooling the patient immediately as if the patient has heat stroke. If in doubt, transport to the emergency department is the most prudent action.
The athlete must be hydrated and asymptomatic before being allowed to return to the field, preferably after being cleared by a physician. In general, delaying return to play to the following day is preferable to allow recovery. Practices that may have contributed to the heat exhaustion episode, such as poor diet, insufficient fluids, and so on, should be examined, and corrective actions should be taken to prevent repeat occurrences. If the primary deficiency is one of not
being acclimated, a practice and activity schedule should be engineered to ensure heat tolerance while maintaining conditioning (24).
being acclimated, a practice and activity schedule should be engineered to ensure heat tolerance while maintaining conditioning (24).
Heat Stroke
Heat stroke, a medical emergency, is a failure of internal and external thermoregulatory mechanisms to control the cumulative effects of exogenous heat on endogenous systems, with a subsequent loss of homeostasis and damage to multiple organ systems (3,13,25,26). The mortality of this illness depends primarily on the degree of heat experienced and the duration of the temperature elevation. This again emphasizes the importance of early recognition and treatment. Typically, onset is acute, and a high index of suspicion concerning nonspecific presenting symptoms is needed.
Classic Heat Stroke
Two types of heat stroke are recognized and they differ in important aspects. The better known classic heat stroke occurs most often in the summer and usually during heat waves, which are defined as 3 or more days of air temperatures exceeding 90°F (27). The target populations are the elderly and those with chronic medical conditions and persons who are unable to seek cooler environments usually because of infirmities or financial constraints (Table 57-1). The heat insult occurs over several days and results in hyperthermia, central nervous system (CNS) dysfunction, and anhidrosis. This last characteristic is a major distinction from exertional heat stroke, in which sweating, often profuse, continues. Between 1979 and 1999, 8,015 deaths were reported as heat related in the United States, with almost 50% occurring in the age group over 65 years old (27). Again, comorbidities contribute to the mortality of classic heat stroke. It is likely that the true incidence of this disease is higher because the resulting organ system failures (e.g., cardiovascular, renal, CNS) may be identified as the cause of death instead of the initiating heat injury.
Exertional Heat Stroke
Exertional heat stroke is defined by a core temperature greater than 104°F and severe CNS disturbances (see Table 57-1). Affected individuals are usually younger, more physically fit, and involved in physically challenging activities. For the 20% who have a prodromal syndrome, presentation may be similar to that of heat exhaustion (13). Symptoms may include dizziness, nausea and vomiting, frontal headache, confusion, drowsiness, disorientation, muscle twitching, ataxia, and psychiatric symptoms. More often, however, collapse is acute. Patients may experience syncope, seizures, and coma. Objectively, tachypnea, tachycardia, hypotension, and cardiac arrhythmias may be noted in addition to the elevated rectal temperatures. In the field, where a rectal probe may not be available, a presumptive diagnosis of exertional heat stroke may be made when the patient is hot, environmental conditions are conducive to heat injury, and there are signs of moderate to severe CNS dysfunction.
TABLE 57-1 Comparison of Symptoms of Classic and Exertional Heat Stroke | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
Immediate recognition of heat stroke is critical because no inherent internal thermoregulatory mechanism is adequate to combat the widespread effects. Although CNS involvement is the hallmark, other systems are also damaged, including the cardiovascular, integument, renal, splanchnic, and hepatic systems. The clinical picture has been likened to sepsis. A current theory for the global abnormalities seen postulates that, as skin blood flow increases to dissipate an ever increasing heat load, splanchnic circulatory support erodes to the point that gram-negative proteins are able to cross the blood–tissue barrier and cause decreased vascular resistance (28). It should be no surprise, given our unfolding knowledge that the inflammatory system involvement comprises multiple processes, that the current heat stress model attributes at least some of the tissue effects to circulating cytokines such as interleukin C. These modulators effect further changes, which serve to worsen the clinical situation.
With the normal shunting of blood from central to peripheral circulation exacerbated by pre-existing dehydration, the patient will demonstrate hemodynamic compromise via an elevated heart rate, a decreased blood pressure,
and CNS compromise. It is not hard to appreciate, then, that the dehydrated or insufficiently hydrated athlete would be more susceptible to heat injury.
and CNS compromise. It is not hard to appreciate, then, that the dehydrated or insufficiently hydrated athlete would be more susceptible to heat injury.
Treatment
The next critical step following recognition is immediate resuscitation and cooling (21,24,25,26). As with any emergency, attention to airway, breathing, and circulation is paramount. Simultaneously, cooling must be initiated, and the emergency medical system must be alerted.
Two basic methods presently advocated in the literature are cool water/ice immersion and evaporative cooling (13,24,29). More easily accomplished in the field, evaporative cooling involves removing the outer equipment and clothing (attempting to preserve modesty), spraying water over the patient, and creating air currents/increasing air flow with the use of devices such as fans. An advantage to this method is that other aspects of resuscitation, such as airway support and cardiac monitoring, are not hindered by the measures used to cool the patient.
Cold water or ice immersion has been shown to produce a cooling rate twice that of evaporative cooling but is not usually available in a prehospital setting. The skin vasoconstriction achieved by immersion techniques serves to shift skin blood flow back to the central circulation and improves the hypotensive states. Other more traditional approaches such as packing the axilla and groin with ice packs have not been shown to be as effective.
If effective cooling and other resuscitative measures can be promptly initiated and appropriate medical support is available on scene, the rule of thumb is to cool first and then evacuate to a medical facility. Intravenous hydration with normal saline is also recommended. If repeat rectal temperatures show a decrease to the target goal of 101 to 102°F, the patient should still be transported to monitor status and evaluate organ system damage.
Complications and Special Considerations
Following exertional heat stroke, guidelines for returning the athlete to activity are similar to those for heat exhaustion. The patient may have suffered complications that would contraindicate further participation in hot environments. The permanence of heat illness susceptibility after heat stroke is controversial, with some studies implying there is no increased risk.
The athlete must be completely asymptomatic and all laboratory abnormalities must be resolved before return to play/activity is considered (24). The physician must provide activity clearance after a recovery time appropriate to the injury suffered and specific guidance on exercise allowed. In cooperation with the athletic trainer, a gradual acclimatization schedule must be developed to ensure maximal tolerance to elevated ambient temperatures.
Conclusion and Future Directions
Of course, the goal should be to prevent heat injury and illnesses before they happen. To this end, various groups including the NCAA and the National Athletic Trainers’ Association (NATA) have issued guidelines on preventive measures. Education is the first step. Coaches and athletes alike must be informed as to proper evaluation and maintenance of hydration, as well as recognition and on-site management of heat-related illnesses.
Ensuring adequate hydration has been a focus of prevention and has been approached in various ways. First, the baseline weight of the athlete should be ascertained. Then, various techniques have been used to assess the change in hydration status with exercise and play. These include reweighing the athlete during and after practice, evaluation of urine-specific gravity, comparison of urine color to standardized charts, and actual measurement of urine output (17). Individuals should be able to determine their specific sweat rate and alter fluid/electrolyte intake to maintain homeostasis even during elevated ambient temperatures (17).
One recommendation is a buddy system where partners are educated on the symptoms of heat illnesses, know each other at baseline, and are alert to physical and mental status changes that may signal the onset of hyperthermic conditions (1).
Hydrating before, during, and after practice/activity has long been recognized as vital to encouraging adequate fluid intake. Although plain water is normally sufficient to replenish fluids, the addition of flavor and electrolytes has been demonstrated to increase voluntary hydration. Specific recommendations have been advanced to address hydration goals at various stages in activity. The current pre-exercise hydration regimen promotes ingestion of 500 mL of fluid 2 hours before exercise with the given provision that the athlete is already euhydrated (17).
Fluid intake during activity should be encouraged, with a minimum of 250 mL consumed every 20 minutes. This frequency is a general guideline and must be amended depending on the sport. Finally, replenishment of fluids after exercise should be determined by the weight lost, with the ideal being that the fluid volume ingested is equivalent to approximately 150% of weight change (17,30).
Prevention of heat injury is an ongoing process that begins with each new season. Background knowledge on heat illness should be explored with each athlete, and myths should be replaced with established and relevant facts. Only concerted teamwork with the athletes, coaches, athletic trainers, and providers can effectively alleviate heat-related morbidity and mortality.
People visit areas at altitudes greater than 2,500 m every year and engage in activities ranging from sedentary (hanging out in the lodge) to active (e.g., biking, skiing, boarding) and
strenuous (e.g., mountaineering). Physicians practicing in this setting should become familiar with the signs and symptoms of various high-altitude syndromes. In addition, trauma may occur concomitantly or as a result of high-altitude illness, making it necessary to recognize and treat both the orthopaedic injury and altitude-related illness in the same patient.
strenuous (e.g., mountaineering). Physicians practicing in this setting should become familiar with the signs and symptoms of various high-altitude syndromes. In addition, trauma may occur concomitantly or as a result of high-altitude illness, making it necessary to recognize and treat both the orthopaedic injury and altitude-related illness in the same patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree