Environment
Thomas H. Trojian
Environment changes the outcome of athletic events on a regular basis. The effects of fog, rain, cold, heat, and altitude alter the performance of athletes, interfering with the body’s ability to maintain homeostasis. In this chapter, the effects of the environment on the human body are discussed. Ways of preventing environmental related illness are detailed. Treatments for these environmental illnesses are also addressed.
Heat Stress
Introduction
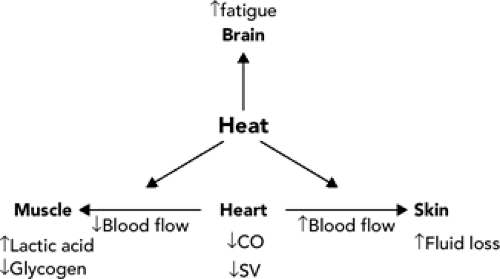
As heat stress increases, there is a reduction in physical performance (see Figure 21.1). Heat is a limiting factor during exercise, irrespective of dehydration or fuel availability status. The body must divert blood flow from muscles to the skin to regulate core temperature (1). This shunting causes a reduction in physical performance. Compounding the problem is the loss of fluid volume due to sweating causing a hypohydrated state. The diversion of blood flow from the muscles and loss of volume due to sweating leads to a decrease in cardiac function. A reduction in stroke volume and cardiac output occurs. This causes the muscles to use more carbohydrates, burning up stored glycogen and producing lactic acid (2). There is an increased perceived exertion and earlier onset of fatigue (3). All these factors bring about a decrement in physical performance.
The body’s ability to thermoregulate during exercise depends upon a myriad of factors (ambient temperature, humidity, and wind velocity, radiant heat from the sun, and the intensity and duration of exercise). To protect against the development of heat stress, exercise intensity and duration can be altered. Factors such as the weather cannot be altered, but they can be monitored. This is an important means of assessing environmental heat stress, an important factor in planning any outdoor sporting event.
Wet bulb globe temperature (WBGT) is the most efficient method (4) for determining environmental heat stress. The WBGT is determined by using several instruments: (a) a dry bulb thermometer, which measures ambient temperature (Tdb), (b) a wet bulb thermometer that measures humidity, (Twb) and (c) a black globe thermometer (Tg) that measures radiant heat. If the WBGT Index and wind speed are both measured, an effective temperature can be calculated. Table 21.1 correlates WBGT measurements and exercise safety. A useful website is http://www.smasa.asn.au/resources/hotweather.htm (September 2006.)
Thermoregulation
The main forms of heat loss in humans are evaporation, conduction, convection, and radiation. Evaporation is the loss of heat by evaporation of sweat from the skin. Conduction is the loss of heat passively through tissue to the periphery from the core. Convective heat loss occurs when heat is transferred from the core by the blood to the skin, warm air next to the body is displaced by cool air. The biggest factor contributing to convective heat loss is wind. Radiation is the loss of heat from the warmer body
to the colder environment. Exercising muscles produce a large amount of heat. Roughly, 75% of the energy produced by the utilization of carbohydrates and free fatty acids is converted into heat. The human body acts as a literal furnace. At rest, humans utilize different methods of regulating core temperature compared to times of activity. At rest, the body relies on radiation over evaporative heat loss. The normal percentages are 50% and 20% for radiation and evaporation, respectively, at rest compared to 5% and 80% to 90% when exercising. The change to heat loss by way of evaporation is necessary to maintain core temperature in a narrow physiologic range.
to the colder environment. Exercising muscles produce a large amount of heat. Roughly, 75% of the energy produced by the utilization of carbohydrates and free fatty acids is converted into heat. The human body acts as a literal furnace. At rest, humans utilize different methods of regulating core temperature compared to times of activity. At rest, the body relies on radiation over evaporative heat loss. The normal percentages are 50% and 20% for radiation and evaporation, respectively, at rest compared to 5% and 80% to 90% when exercising. The change to heat loss by way of evaporation is necessary to maintain core temperature in a narrow physiologic range.
TABLE 21.1 Guideline for Exercise in Heat | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
The human body maintains a core temperature in the range of 35°C to 40°C (95°F to 104°F). The core temperature increases with exercise reaching a plateau level of homeostasis tolerated by the athlete. This level can be as high as 41°C (105.8°F) in elite athletes. The maintenance of core temperature is accomplished by the use of thermodetectors in the hypothalamus, spinal cord and limb muscles to maintain and regulate core temperature during exercise. Well-conditioned athletes can produce and dissipate over 1,000 kcals/hour safely. Radiation and convection dissipate most heat when the ambient temperature is greater than 20°C (68°F) and less than 35°C (95°F). Radiation is very important when the ambient temperature is below the body temperature. The body uses conduction and convection to transfer heat less effectively.
Evaporation is the main defense against heat stress. The body sweats to remove heat. This is accomplished by the evaporation of the sweat from the skin. Evaporative heat lost can remove a large amount of energy with 1 L of sweat removing approximately 600 Kcal of energy. An athlete will sweat varying amounts with the normal range being 0.5 to 1.5 L/hour but enormous rates of 4 L/hour have been noted. Sweat is only useful when it is in contact with the skin. If it is wiped off or rolls off the body, then the heat cannot be transferred away from the skin by this method.
The body is able to compensate for the energy produced in exercise to a certain point after which the compensatory factors fail (5). This occurs when the amount of heat generated by the human furnace is greater than the amount possible to dissipate. This varies by the intensity of the activity and the surrounding environment. The core temperature increases as the body is unable to further remove heat by evaporation. The two main reasons for the inability to shed further heat by evaporation are (a) a high WBGT in which the humidity is such that evaporation is diminished, and (b) hypohydration or dehydration in which the production of sweat is decreased. As the loss of body fluid increases, the core temperature increases faster. Compounding the problem, with dehydration the core temperature during exercise that an athlete is able to tolerate is lower. This is due to the reduction in stroke volume as well as the reduction of the volume of blood to the skin and decrease in sweating with dehydration. Hypohydration, as low as 1%, can produce an elevation in core temperature during exercise (6). The amount of increase in core temperature ranges is significant with 0.1°C to 0.25°C (32.18°F to 32.45°F)/percent body weight lost. As the amount of hypohydration increases so does the core temperature.
Predisposition
Several factors increase the susceptibility of an athlete to heat stress (7). Dehydration is the prime factor as discussed in the previous section. Preventing dehydration is important in preventing heat stress. A few facts are important to understand. Regular replacement of fluids is needed because thirst is a poor predictor of fluid status. Most athletes do not develop thirst until they have loss more than 2% body weight. One should note that sweat is hypotonic. There is very little salt in sweat, as well as the amount of salt in sweat decreases with training and acclimatization. Therefore, cold water is the best replacement fluid during exercise. When prolonged activity of greater than 1 hour is performed, a hypotonic salt solution with a 6% to 7% glucose polymer will aid in absorption of fluids.
Acclimatization is important in dealing with heat stress during exercise. This develops with 7 to 10 days of exposure. The benefits of heat acclimatization come from improved skin blood flow rates, earlier onset of sweating, an increased plasma volume, and a lower metabolic rate. Exercising in the heat for 100 minutes is the most effective method of adapting. It is important to increase the core temperature during exercise to develop the adaptive effects quickly. Even sedentary people will adapt to heat but not as quickly as exercising people. The effect is transient and is retained for 2 weeks after last exposure, which proceeds to rapid lost of acclimatization over the next 2 weeks. The more fit an athlete is, the slower the loss of the adaptive benefits.
Clothing and equipment can be significant inhibitors of heat dissipation. Dry clothes soak up sweat and prevent evaporative heat loss. Dark clothes will cause radiant heat gains instead of loss. Football equipment prevents heat loss, thereby at a lower WBGT heat related problems can occur. Adjustments in practices are needed to protect against heat stress (8). These include using less equipment (such as helmet and shorts) during high WBGT and switching
practices to early morning or after sundown when the WBGT is lower.
practices to early morning or after sundown when the WBGT is lower.
There is a greater potential for heat stress during a febrile illness. These conditions can produce dehydration. Fever will cause an increase in the core temperature and decrease the body’s ability to compensate to the heat. Exercising with fever is a dangerous practice especially in the heat.
There are many prescription and over-the-counter medications that can augment the heat stress. Medications such as diuretics cause dehydration. Amphetamines and stimulants can increase metabolic rate and therefore heat production. Anticholinergic agents can decrease sweat production and therefore the evaporation of sweat and removal of heat. These medications should be avoided during exercise.
Women seem to have better thermoregulation than males. Variation in heat dissipation is noted over the menstrual cycle with a slight decrease in the luteal phase. This decrease does not appear to be clinically significant. Estrogen replacement therapy is falling out of favor for numerous reasons but it appears to give a minimal benefit in thermoregulation in postmenopausal women.
Heat Cramps
Heat cramps occur from involuntary contractions of exercising muscles. Calf muscles are by far the most common but any muscle in the body can be affected. The cause is presumed to be an electrolyte imbalance during exercise. However, there is evidence that a spinal neural mechanism may induce cramping that is unrelated to biochemical changes either in the blood or in the affected skeletal muscle (9). The best treatment is prevention with proper hydration, sodium, and calcium supplementation. The standard treatment of heat cramps involves rest, massage, passive stretch, and rehydration. Some people swear by the use of pickle juice or yellow mustard to relieve cramps. The reason for the anecdotal success of these two treatments is unknown but both are high in sodium.
Heat Syncope
The syncopal episode occurs in the elderly and the poorly acclimatized individual due to volume depletion, peripheral vasodilatation, and decreased vasomotor tone. The athlete is vasodilated with large pooling of blood in the leg muscles, the heart rate and cardiac output decreases, resulting in insufficient blood supply to the brain. This is made worse by dehydration or a poor cool down after running. Treatment involves elevating the legs (to increase preload and stroke volume), rehydration, and transfer to a cool shaded location. Cardiac and neurological causes need to be considered in the evaluation
Heat Exhaustion
Athletes with heat exhaustion present with fatigue, weakness, piloerection, lightheadedness, headache, and neuromuscular incoordination. They typically have elevated rectal temperatures below 104°F (40°C). The problem is due to inadequate cardiac response to heat stress. Blood is shunted to the muscles and the skin and there is a lack of cardiac preload to maintain cardiac output. Athletes may develop neurological symptoms of headache, irritability, and mild confusion. Treatment is the same as heat stroke.
Heat Stroke
Heat stroke is an emergency that needs to be recognized early (10). The athlete will present with an elevated rectal temperature more than 40°C (104°F) and altered mental status. The classic heatstroke patient will present with dry hot skin without sweating. The heat stroke athlete may still be sweating. Obtaining the rectal temperature of anyone with neurological symptoms is essential. The success of treatment is in early recognition. Difference in symptoms between heat cramps, heat exhaustion, and heat stroke is listed in Table 21.2.
Exertional heat stroke can cause major organ system problems. Acute renal failure, rhabdomyolysis, and disseminated intravascular coagulation are more common in victims of exertional heat stroke than in victims of classic heat stroke (elderly during heat waves). Laboratory abnormalities can include elevated white blood cell count, elevated liver function tests, and hypokalemia in the initial stages with hyperkalemia manifesting later. Sodium levels can be normal or slightly elevated, depending on the hydration status of the patient. Patients can also have
elevated creatinine phosphokinase (CPK) secondary to rhabdomyolysis. Patients who have peak CPK levels above 10,000 IU/L are at significant risk for the development of acute renal failure.
elevated creatinine phosphokinase (CPK) secondary to rhabdomyolysis. Patients who have peak CPK levels above 10,000 IU/L are at significant risk for the development of acute renal failure.
TABLE 21.2 Comparison between Heat Cramps, Heat Exhaustion, and Heatstroke | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
Acute reduction of the body temperature is the key to recovery and prevention of organ damage. This can be accomplished with ice water immersion or ice packs to the groin and axillary regions. Cool mist fans or alcohol rubs can aid in cooling. Unlike fever from infection in which toxins reset the hypothalamic set point, the elevation in temperature in this case, is due to excessive energy produced. Nonsteroidal anti-inflammatory medicines are not useful in these patients and should be avoided.
In a study of exertional heat stroke cases, ice water immersion lowered core temperature to less than 39°C (102.2°F) in 10 to 40 minutes (12). There were no fatalities in this group. In another study, ice water immersion cooled twice as fast as evaporative cooling (13). The author recommends rapid cooling using ice water immersion whenever possible.
The athlete with altered mental status may have a condition other than heat stroke such as infection, midbrain cerebral vascular accident, drug use, hyponatremia, and hypoglycemia. These other diagnoses need to be remembered when considering treatment. For example, the use of intravenous hydration (half normal saline) would be inappropriate for a runner with altered mental status caused by hyponatremia so obtaining a serum sodium level is important before rehydration is started.
In endurance athletes, hyponatremia can be found secondary to over rehydration with excessive free water. There are seldom mental status changes until the serum sodium level is less than 120 mEq/L. The athlete with a history of large fluid intake in a race or with a later finishing times (usually the less fit runners) is most susceptible. The athlete will have headaches, confusion, and seizures (rare). The same is seen in heatstroke and the rectal temperature is essential in differentiating. Normal temperatures and distal swelling (rings too tight) are reasons for further evaluation of hyponatremia.
Return to activity should be restricted for anyone with syncope, core temperature of greater than 39°C, and neurological symptoms. The person should acclimatize to the heat more and avoid high-intensity activities for 48 hours. Athletes with lesser heat illnesses need to be cooled and closely monitored. There is a higher risk for reinjury in athletes with prior heat illnesses.
Precooling
Prolonged exercise causes body temperature to rise; the increase in core temperature occurs rapidly and reaches steady state values when heat production matches heat loss. A critical limiting temperature exists; so to reduce the risk of cellular injury or heat related illness, athletes must reduce their exercise intensity so that exercise can continue. In hot conditions, the temperature gap between the start and the critical temperature is narrowed and the situation is exacerbated, often resulting in the termination of exercise. When exercising in high temperature environments, it would therefore be sensible to start exercise with a lower body temperature. Precooling (core body temperature cooling) before exercise would be expected to widen the temperature gap and delay the time before the critical limiting temperature is reached (14).
Studies confirm that increasing body heat is a limiting factor during exercise. Precooling is probably only beneficial for endurance exercise of up to 30 to 40 minutes rather than for intermittent or short-duration exercise (15,16,17). Studies show precooling before an endurance event may be worthwhile if the facilities are available. Precooling takes approximately 30 minutes to complete and can be done in either a swimming pool or a cold shower (18). Ice vests have been used and are more portable than immersion techniques. Precooling could be advantageous for endurance exercise in warm conditions (18).
Cold Stress
Physiology
During cold weather, the body tries to maintain core body temperature while heat loss continues to occur due to conduction and convection mechanisms. The wind chill index is a measurement used to evaluate the effects of increased wind speed on heat loss. Wind increases conductive heat loss, therefore increasing cooling. A difference in ambient temperature and body temperature increases conduction heat loss. The loss of body heat by conduction is 25-fold greater in water than in air (19). A person in 20°C (68°F) water will become hypothermic depending on clothes and size of person in 2 to 40 hours whereas a dry person in 20°C (68°F) temperature on dry land would not become hypothermic.
In an attempt to maintain core body temperature, basal heat production increases slightly in the cold. Yet, it is not sufficient to maintain body temperature. A layer of subcutaneous fat is helpful to act as an insulator against the cold, but again the benefit is small. Intake of calories and exercise is important to generate sufficient calories to stay warm.
Voluntary and involuntary methods of heat generation are used to maintain core temperature in humans. The body will produce 3 to 6 times the basal amount of heat by involuntary shivering. Shunting of blood from the skin to the core also occurs to prevent heat loss. Thermoreceptors in the skin signal the hypothalamus to increase heat generation both voluntarily and involuntarily and to constrict peripheral circulation.
Voluntary exercise can generate significant heat. The body acts as a furnace keeping the core temperature in the narrow physiologic range. Approximately 75% of muscle contraction energy is released as heat. The amount of energy
the body can generate diminishes as energy stores are used up. Mild to moderate intensity exercise produces sufficient heat and helps to keep the temperature in the physiologic range. It generates less heat than severe intensity exercise but longer duration exercise is possible. Mild intensity exercise often does not produce enough heat to prevent shivering.
the body can generate diminishes as energy stores are used up. Mild to moderate intensity exercise produces sufficient heat and helps to keep the temperature in the physiologic range. It generates less heat than severe intensity exercise but longer duration exercise is possible. Mild intensity exercise often does not produce enough heat to prevent shivering.
As the body’s core temperature starts to drop, a cold-induced diuresis occurs. This occurs because the cardiac output increases and the systemic vascular resistance is higher. The kidneys receive an increase in blood flow and an increased of amount of fluid is filtered. As the body’s core temperature drops lower, the renal perfusion decreases as cardiac output becomes less and less.
Hypothermia
Hypothermia is a seen in prolonged athletic events where the temperature is below 10°C (50°F), precipitation is occurring and wind speed is elevated. Most cases, in sports, will be mild but in extreme sports during winter, the severity of hypothermia can increase. Care needs to be implemented to maintain reheating of the individual.
Mild Hypothermia
Mild hypothermia is when the body core temperature is between 32.2°C and 35°C (89.96°F and 95°F) (20). The person will have confusion, slurred speech, impaired judgment, and amnesia. Cardiac output increases with tachycardia and increases preload secondary to the peripheral constriction. Shivering still occurs at these temperatures to stimulate heat. An athlete with confusion, dysarthria and ataxia with prolonged exposure to the cold should be considered to have hypothermia. A rectal temperature is needed to evaluate core temperature. It is useful to assess consciousness and shivering. A shivering conscious athlete probably has a core temperature above 31°C (87.8°F); whereas a severely disoriented or unconscious athlete not shivering is likely to have a core temperature below 31°C (87.8°F).
Moderate/severe Hypothermia
Moderate hypothermia presents with lethargy, disorientation, and unconsciousness. As the core body temperature lowers, cardiac output decreases and respiration is decreased and shallow. Before loss of consciousness, people have been known, paradoxically, to undress. This phenomenon is secondary to the loss of peripheral vasoconstriction and sudden warming of the extremity and sense of over heating. This severe impairment in judgment does not allow them to realize that this is a poor choice. Paradoxical undressing is a poor prognostic sign.
Severe hypothermia is often confused with death. The person has fixed dilated pupils, poor pulse that could be missed on palpation, severe muscular stiffness, and areflexia, even to noxious stimuli. Electrocardiography (EKG) may show asystole, ventricular fibrillation and other findings. The person without an EKG abnormality can have an arrhythmia triggered with sudden jarring. Careful assessment of the person with hypothermia is needed to guarantee no pulse before starting cardiopulmonary resuscitation (CPR). If possible, cardiac monitoring should be done.
Treatment
Treatment for hypothermia has common components for mild, moderate and severe forms. Further heat loss should be prevented (21). The person should have any wet clothes removed. Rectal temperature should be measured and monitored if possible. Prevention of worsening orthostatic hypotension is done by placing them supine. A barrier to the cold ground such as a sleep pad, blanket, or sleeping bag is needed to prevent conductive heat loss. All of these things should be done for every hypothermic patient.
The person with mild hypothermia needs to be kept warm, supplied with warm beverages and allowed to shiver. The shivering will effectively reheat the body. Exogenous rewarming is not needed. Actually, it may slow reheating. Heated humidified air is not going to add a significant temperature increase. It is important to prevent further heat loss.
Moderate to severe hypothermia needs close observation and cardiac monitoring. Careful transport to a hospital is the best option/action. Active external rewarming is needed in these patients once recooling can be prevented. The use of heat packs to the groin, axilla and neck, as well as feet in hot water or force heated air device (e.g., Bair Huggers, Arizant Healthcare Inc., Eden Prairie, MN) can be useful. Care is needed to avoid thermal burns.
For severe hypothermia, active internal rewarming is recommended. Warmed intravenous solution (normal saline) at 43°C (109°F), peritoneal lavage with warmed fluids and, if possible, warmed (42°C to 46°C [108°F to 115°F]) humidified oxygen during bag-mask ventilation is to be administered. If the victim is pulseless with no detectable signs of circulation, start chest compressions immediately. Follow advance cardiac life support principals (22).
Frostnip
Frostnip is what most people get when they go out in the cold and their nose, ears, toes, fingers, cheeks, or chin get white and cold. Often ice crystals will be seen on the surface of the skin. It occurs slowly and painlessly. Reheating occurs quickly and redness, pain, and hypersensitivity will develop over the affected area. There is no permanent damage after reheating. It is important to warm the affected area and keep the area warm to prevent further freezing and damage.
Frostbite
Frostbite is a problem in athletes exposed to freezing or near freezing weather such as those participating in orienteering, cross-country skiing, hiking, kayaking, skiing, ice climbing, and skating. Any sport performed outdoors can increase the risk for frostbite if the athlete is outdoors for prolonged
periods. Length of exposure is the most important risk factor in the severity of injury.
periods. Length of exposure is the most important risk factor in the severity of injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree