CHAPTER 14 Endoscopic Distal Biceps Repair
Tears of the distal biceps tendon represent a diagnostic and imaging challenge for the orthopedic surgeon and sports physician.1–8 Complete tears of the distal tendon account for approximately 3% of all tears involving the muscle, and partial tears are less common, although their exact incidence is unknown.1–5 The symptoms may be subtle (e.g., antecubital pain) and signs difficult to illicit (e.g., weakness of elbow flexion and supination). Physicians who remain alert to the possibility are most likely to suspect the diagnosis. Use of correct imaging and of surgical endoscopy can lead to the correct diagnosis and management of the condition.
ANATOMY
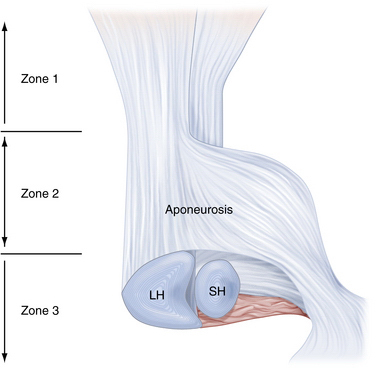
Biceps brachii is the most superficial of the muscles in the anterior compartment of the arm, and it has two heads of origin. It acts across three articulations: the shoulder, the elbow, and the proximal radioulnar joint.9 The short head takes a tendinous origin from the tip of the coracoid process of the scapula, immediately lateral to the origin of the coracobrachialis muscle. The long head arises from the supraglenoid tubercle and adjacent glenoid labrum. The two tendons expand into fleshy fusiform bellies, held together by loose epimysial tissue.9,10 As they traverse parallel through the upper arm, the belly of the short head always remains to the ulnar side and the long head to the radial side.9 It was once held that the two bellies fused below their main convexity, just above the elbow joint,4,9,10 but anatomic cadaver studies have revealed a variable amount of interdigitation.10 Eames and Bain10 also described the distal tendon as having two distinct components held together by loose adventitia, one arising from each belly. Eames and Bain10 further divide the distal biceps tendon into three zones.
In zone 1, the pre-aponeurosis, a variable amount of muscular interdigitation of the two bellies occurs, with many cadavers showing none at all (7 of 17 specimens). Where it was present, the raphe was easily overcome by blunt finger dissection (Fig. 14-1).
Zone 2, the aponeurosis or lacertus fibrosus, consists of three layers. The superficial layer arises from the anterior, radial aspect of the long head at the level of the distal musculotendinous junction. It spreads distally and ulnarward, coursing anterior to the musculotendinous junction of the short head. The middle layer acts as a mesentery to the short head tendon, embracing it before it passes distally and ulnarward and merges with the superficial layer. The deep layer arises from the deep radial aspect of the long head and sweeps distally and ulnarward, deep to the short head tendon. The three layers subsequently merge and continue distally as a single aponeurosis. The lacertus fibrosus has wide and deep involvement in the flexor compartment of the forearm—it completely encircles the flexors and has fascial attachments, particularly to the ulnar flexors, and it incorporates the median nerve and brachial artery.10
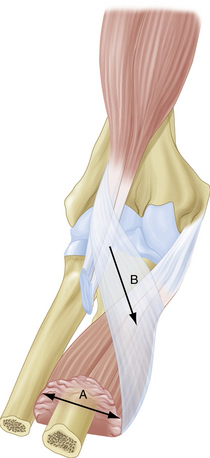
In zone 3, the post-aponeurosis, the two tendons continue distally past the lacertus fibrosus and insert onto the radial tuberosity. The distal biceps tendon footprint on the radial tuberosity is 2 × 14 mm.11 In all specimens, the long head tendon passed deep to the short and inserted more proximally.10 This point is also farthest away from the point of rotation of the radius. The tendon of the short head curves anterior to the long and inserts in a fanlike fashion on the distal portion of the radial tuberosity and extends distal to it (Fig. 14-2). With these different insertions, the long head provides greater supination power, and the short head may provide more flexion power, which can help in clinical evaluation of partial tears to localize the tear by power testing.
Surrounding the tendon insertions is the bicipitoradial bursa.7,8,10,12 This structure is of great clinical importance in endoscopic evaluation of the distal tendon after injury. Eames and Bain10 found that the bursa encircled the tendons in all cases of their anatomic study. They observed that the bursa was easily distended by approximately 7 mL of normal saline from its deep radial side. The bursa drapes over the tendons, is teardrop shaped, and lies between the groove in the brachialis muscle and the distal tendons with the elbow extended and between the proximal radius and biceps tendon during pronation (Fig. 14-3).8,10
PATIENT EVALUATION
History and Physical Examination
Complete tears of the distal biceps tendon are uncommon, accounting for 3% of all tears involving the biceps.1–5 Partial tears are less common, but descriptions of this type of tear in the literature is increasing, probably as recognition of the pathology improves. Maintaining clinical suspicion of tears of the distal tendon (particularly partial tears) is likely key, particularly in the presence of sometimes very subtle clinical signs.
The age of presentation of patients with partial tears is slightly higher than that of those with complete tears—mid-50s and mid-40s, respectively.10,13 Almost all complete tears reported in the literature have occurred in male patients, whereas partial tears have been reported for both sexes.1–3
In complete and partial tears, the dominant limb is most often affected.4 In the case of complete tears, the injury occurs through sudden, forced, eccentric contraction of the biceps muscle, such as a sudden and unexpected extension load on a flexed elbow.4,6,10,13 Partial tears are associated with mixed etiologic factors.
Partial tears are caused by acute traumatic and chronic degenerative mechanisms.1,2,4,13 The mechanism of injury of acute partial tears is the same as for complete tears, but the force causing the injury is interrupted before complete avulsion occurs. Various mechanisms for degeneration have been proposed, including abnormal friction forces, impingement, repetitive strain with supination and pronation, and vascular changes in the tendons.4,10 It is our experience that degenerate tears of the biceps tendon can occur in the older patient and occurs more often in female patients.
The patient often reports pain in the antecubital fossa, weakness of flexion or supination and possible limitation of elbow range of motion, particularly flexion.1-6,8,10,13 Inspection may reveal swelling and bruising at the antecubital fossa. This can be an inconsistent finding, particularly in partial tears.4 Tenderness is elicited on palpation of the antecubital fossa. Pain with resisted supination is a common finding. With complete ruptures, the distal biceps tendon is not palpable in the antecubital fossa, and the physician must be careful that the biceps tendon is being examined, not mistakenly an intact lacertus fibrosus.
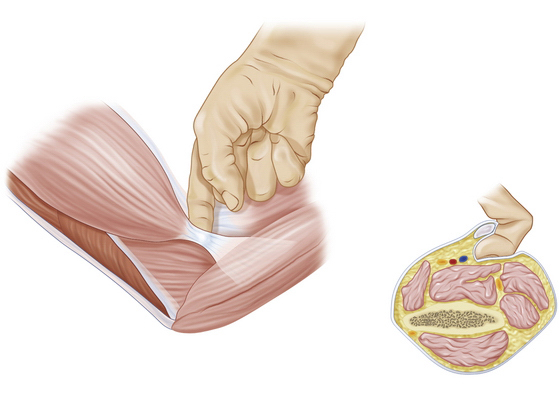
The hook test for distal biceps was described by O’Driscoll and colleagues.14 While the patient actively supinates with the elbow flexed 90 degrees, a positive hook test result permits the examiner to hook his or her index finger under the intact biceps tendon from the lateral side. With an abnormal hook test result, indicating distal avulsion, there is no cordlike structure under which the examiner may hook a finger (Fig. 14-4).14 The hook test is highly sensitive and specific for complete tears of the distal biceps tendon (as good as or better than magnetic resonance imaging), and it is easy to perform.
A large area of bursitis can compress the median nerve3 and may produce neurologic signs distally. Imaging can differentiate other diagnoses in the absence of trauma (e.g., antecubital lipoma, other tender lesions) from distal biceps tendinitis or bursitis.
Diagnostic Imaging
Plain radiography usually is not helpful in the diagnosis of distal biceps tendon tears. Some calcification of degenerate tendons may be seen at the radial tuberosity, but this is not a reliable diagnostic finding and has been reported only for complete tears.15
Traditional positioning techniques for MRI of the distal biceps tendon yielded images that were difficult to interpret,5,6 because axial images are obtained from an extended arm for a tendon with an oblique course in the antecubital fossa. Giuffre and Moss5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree